The case we report is a rare example of a fistula originating from the descending branch of the left coronary artery to the pulmonary trunk in a 76-year-old woman. The prevalence of coronary artery fistulas (CAFs) in the general population ranges from 0.17% to 0.68%, depending on the source [1, 2]. Single anomalies originating from the left anterior descending artery (LAD) are the most frequent [3, 4]. According to the latest research, CAFs primarily drain into the pulmonary artery [5]. Most CAFs are detected incidentally due to their asymptomatic course, often resulting from a small diameter. Consequently, a significant number of them remain clinically silent [6]. The treatment options for CAFs are either surgical closure of the anomaly or less invasive percutaneous procedures. The techniques include the use of a fabric-covered stent graft, coil embolization, plug closure, detachable balloon technique and the use of cyanoacrylate glue [7, 8].
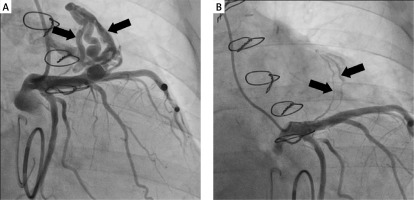
The cardiac surgery clinic received a referral for surgical treatment of a complex heart defect in a 74-year-old female patient with heart failure classified as NYHA II/III due to mitral regurgitation and tricuspid regurgitation. The patient also had type II diabetes and persistent atrial fibrillation. Over the past 5 years, the patient had reported a decline in exercise tolerance and intermittent chest pain. During preoperative diagnosis, echocardiography revealed dilatation of the heart cavities, dilatation of the tricuspid and mitral annuluses, along with left ventricular systolic dysfunction. Coronary angiography showed no significant stenosis in the coronary arteries, but it did reveal a coronary-pulmonary fistula originating from the LAD to the pulmonary trunk, which was classified as a hemodynamically significant defect (Figure 1 A). The entire diagnostic and therapeutic process was based on the coronary angiography. Therefore, the use of multislice computed tomography (MSCT) was unnecessary. Mitral valve plication and tricuspid valve plication were performed, with implantation of a 32 mm CE Physio ring for each. Due to the complexity of double-valve surgery, the prolonged duration of the operation and the non-visibility of the fistula outlet, no further action was taken in order to avoid serious post-operative complications. The enlargement of the fistula, chest pain and exertional dyspnea supported the hemodynamic significance of the anomaly. The patient was deemed eligible for an attempt at percutaneous closure of the coronary-pulmonary fistula, which was successful. The procedure was carried out via the left radial artery using a 3.5 6F EBU catheter and a Papyrus 4.5 × 15 stent graft. The stent graft was implanted at a pressure of 16 atm, tightened at 18 atm, and the entire length of the stent was finally balloon inflated to a pressure of 22 atm. Closure of the fistula lumen was achieved, with residual contrast retention visible in the vessel. A small vessel undergoing trace contrast was preserved outside the perimeter of the length of the stent graft (Figure 1 B). There were no complications during the procedure, and the patient was discharged without any complaints. During follow-up coronary angiography, the procedure’s effect was maintained, and the patient was prescribed conservative treatment with acetylsalicylic acid and apixaban for 6 months. After that, due to persistent atrial fibrillation, treatment with apixaban was continued. The use of acetylsalicylic acid was justified by the implantation of a stent graft. There are no algorithms regarding the treatment of rare anomalies such as CAFs and antiplatelet therapy. An individual approach is crucial in each case. Further annual monitoring with MSCT is recommended. Over the course of the 2-year follow-up period, the patient has exhibited neither signs of illness nor cardiovascular complications. Nevertheless, in the event of any coronary-related symptoms, heart failure, or the emergence of a new murmur, follow-up coronary angiography is recommended. Currently, the patient feels well; hence, no such procedure is planned.
Figure 1
Coronary angiography images of a coronary-pulmonary fistula originating from the LAD to the pulmonary trunk before (A) and after the procedure (B)
Coronary-pulmonary fistulas are rare anomalies of the coronary arteries. As a result, there are no clear guidelines on how to conduct the patient’s therapeutic process, especially if these anomalies are hemodynamically significant. When undertaking surgical closure of a fistula, the patient’s therapeutic process should be individually planned, combining the experience and skills of the operator due to the numerous difficulties during the procedure. The presented case demonstrates how percutaneous techniques offer more precise treatment than classical techniques.








