Introduction
In adult populations, atrial fibrillation (AF) is the major arrhythmia and successful treatment rates are low [1]. In recent years, left atrial appendage occlusion (LAAO) has become an alternative method for stroke prevention in patients in whom oral anticoagulation (OAC) is ineffective or contraindicated or in patients with life-threatening complications [2, 3]. Previous studies have demonstrated that the LAAO procedure is safe and effective in the prevention of thromboembolic events, including in high risk patients [4–10].
In the medical market, there are a number of available devices including endocardial and epicardial devices [4, 5, 9]. However, in some cases, the anatomy of the left atrial appendage (LAA) may constitute a contraindication to implantation of these devices. The LAmbre device is a novel system, designed especially for LAA closure when problematic morphology is present [11, 12].
Material and methods
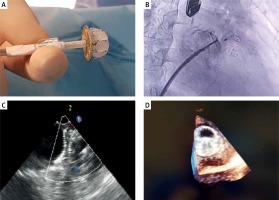
A retrospective, single-center study was performed in 24 consecutive patients with non-valvular AF, who underwent LAAO with the LAmbre device (Lifetech Scientific Corp., Shenzhen, China) between 2016 and 2018 (Figure 1). The LAmbre occluder system was previously described [13]. LAmbre device selection was based on operators’ decision. All procedures were performed under general anesthesia. Patient characteristics are presented in Table I. The LAA anatomy was assessed with computed tomography angiography before each procedure. Oral anticoagulation therapy was discontinued and unfractionated heparin was used during the procedure. After the procedure, aspirin (75 mg/dose/day) and clopidogrel (75 mg/dose/day) for 6 months were recommended in each patient. Leak was defined as the presence of flow from the left atrium to the LAA < 3 mm [14].
Table I
Patient characteristics (n = 24)
Figure 1
LAmbre occluder connected to the sheath (A), fluoroscopy (B), transesophageal echocardiography (C) and 3D echocardiography (D) of the LAmbre occluder after release and correctly placed in the left atrial appendage
Follow-up visits, including transesophageal echocardiography, were performed at 3 and 6 months post-procedure. Data on mortality, causes of mortality and serious adverse events (SAE) were collected.
Results
All procedures were successfully completed with no perioperative complications. The LAAO procedure or device related mortality was 0%. The mean time for the procedure was 62.92 ±14.21 min. Eleven different sizes of occluder were implanted during the procedures, depending on the size and shape of the left atrial appendage. The choice of device size was made by the operator during the procedure based on intraprocedural transesophageal echocardiography (TEE) examination. There was a 100% success rate with no complications. No post-procedural leaks were observed. Half of the patients were discharged from hospital on the second or third day following the procedure.
The overall follow-up was 349 months. During the follow-up period, there were 4 (16.7%) deaths; 1 case with acute exacerbation of chronic renal failure complicated by heart failure (5 months after the procedure); 1 case of out-of-hospital cardiac arrest (5 months after the procedure), 1 case of post neurosurgery complications due to cerebral artery aneurysm (15 months after the procedure) and in 1 case, the cause of death was unknown. There were no deaths connected to the procedure. Gastrointestinal bleeding were observed in 2 (8.34%) cases. There was 1 (4.17%) case of transient ischemic attack and 1 (4.17%) case of stroke, 16 and 3 months after the procedure, respectively. In both cases control TEE examination showed no device thrombus. In the remaining patients follow-up TEE showed no device thrombi or LAA leaks (Table I).
Discussion
We present the first results in Poland of the LAAO procedure with LAmbre devices, with a 100% success rate and with no perioperative complications. From our initial experience, implantation is associated with a high success rate and good clinical outcomes.
Our results are similar to the most popular endocardial devices such as the Watchman or Amplatzer [4, 15]. Surprisingly, in our study, there was a larger number of postprocedural bleeding episodes, which were observed in 8.34% of patients, compared to other endocardial trials [4, 15]. However, in our study, patients had a very high risk of bleeding (HAS-BLED score 4) and, in more than 60% of patients, the indication for LAAO was previous bleeding episodes. Of note, all bleeding episodes were among patients who were receiving antiplatelet therapy, and none were receiving OAC.
The observed mortality rate (16.6%) was also higher than that reported in other endocardial device trials [4, 15]. However, none of the deaths were related to the procedure. Boersma et al. observed a 9.8% mortality rate at 12 months of observation in a Watchman device trial [4]. Importantly, all deceased patients were free of thrombus on the occluder and from postprocedural leak at 3-month and 6-month visits. Additionally, no device thrombi were observed, despite not receiving OAC, even in transient ischemic attack (TIA) and stroke patients. Similar data were obtained by Huang et al. [14].
The LAA morphology, including the LAA shape, ostium width and depth, plays a critical role in the choice of device. The most popular devices such as the Watchman, with its umbrella-like shape, should be avoided in shallow or multilobar LAAs. The second most commonly used device, the Amplatzer ACP, should be avoided in shallow LAAs because of the relatively proximal position of LAA implantation [13]. The LAmbre device is available in a larger range of device sizes (16–36 mm) compared to the Watchman (21–30 mm) and ACP (16–34 mm) devices. It is also highly adaptive to many LAA sizes due to its smaller umbrellas with larger covers. Therefore, the larger choice of sizes and favorable device properties may make the LAmbre device more suitable for complex LAA anatomies, such as chicken wing or shallow LAA [13].







