Spontaneous coronary artery dissection (SCAD) is a rare phenomenon, mostly occurring amongst young women under the age of 50 [1, 2]. The pathophysiology of SCAD is unknown, but correlations with hypertension, dyslipidemia, female sex hormones, pregnancy, and emotional stress have been found [1, 3]. The disease manifests itself with chest pain typical for acute coronary syndrome. Pregnancy-associated SCAD represents less than 5% to 17% of SCAD cases overall, mainly occurring in the peripartum period [2, 4]. Recently, the number of SCAD cases has increased due to greater awareness of the disease and use of better imaging methods [1, 3].
The day after giving birth, a 38-year-old woman was admitted to the cardiology ward with suspicion of acute myocardial infarction. The patient reported stenocardial chest pain and slight numbness of the left arm. Blood tests showed an elevated troponin hsT level (3624 ng/l) and N-terminal pro-B-type natriuretic peptide level (509 pg/ml). In electrocardiography (ECG), a new right bundle branch block (RBBB) was present.
Emergency coronarography revealed SCAD in the left main coronary artery (LMCA) progressing to the anterior descending artery (LAD) and circumflex artery (Cx) with preserved, slower flow in the circuit of LAD and Cx (Figure 1 A). The right coronary artery was dominant, without any lesions. With LMCA being involved, the risk of total closure of the vessel during intervention was significantly increased. The patient was deemed eligible for conservative treatment after consultation with a cardiac surgeon. Transthoracic echocardiography (TTE) showed hypokinesis of the basal and middle segments of the intraventricular septum. A week later, a computed tomography coronary angiography (CCTA) showed a semilunar, hypoattenuating cuff around the LAD in the seventh segment (12 mm length) of the LAD, with an image corresponding to a coagulated intramural hematoma (Figure 1 B). During hospitalization, she was diagnosed with arterial hypertension, obesity, and mixed hyperlipidemia. The patient was discharged home in good condition after 14 days of hospitalization on 75 mg of acetylsalicylic acid.
Figure 1
A – Coronary angiography showing: SCAD in the left main coronary artery (LMCA) progressing to anterior descending artery (LAD) (white arrow) and circumflex artery (Cx) with preserved, slower flow in circuit of LAD and Cx – first hospital admission. B – Computed tomography angiography showing: semilunar, hypoattenuating cuff around LAD in seventh segment (12 mm length) of LAD (white arrow), image corresponding to a coagulated dissection – first hospital admission. C – Semilunar, hypoattenuating cuff around the LAD in longitudinal view – hospital readmission. D – Semilunar, hypoattenuating cuff around the LAD in transverse view – hospital readmission
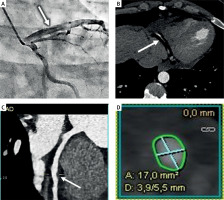
Four days later, the patient was admitted to our ward due to a recurrence of non-specific retrosternal chest pain with mild exertion. The patient reported similar stenocardiac symptoms as at the first admission. Troponin tests were borderline positive, without a dynamic increase in serial measurements. TTE indicated a preserved left ventricle ejection fraction. Follow-up CCTA was performed, and coagulated intramural hematoma of a length of 10 mm was indicated in LAD. The hypotensive, semilunar cuff was less perceptible than in the previous examination. It did not cause significant stenosis in LAD, LMCA, or Cx (Figures 1 C, D).
No recurrence of retrosternal pain was observed during hospitalization. Due to the patient’s bradycardia, metoprolol was discontinued. In ECG, the patient had a first-degree atrioventricular block, RBBB, and left anterior hemiblock. The patient was discharged home after 6 days on 75 mg of acetylsalicylic acid. No more symptoms occurred after discharge.
Pregnancy-associated SCAD patients tend to have a more severe onset of disease, including impaired left ventricular function, shock, or even multivessel dissections [4]. It was reported that 10% to 22% of patients with SCAD face reoccurrence of dissection but in different, previously unaffected arterial parts [1, 3, 4]. Therefore, it is important to investigate the factors influencing the development of SCAD, in order to implement preventive measures. Currently, there are no randomized trials because of the small group of patients affected by SCAD, so there are still many uncertainties surrounding this condition. Physicians should maintain high awareness of SCAD in patients meeting the criteria and circumstances mentioned in the manuscript.








