Percutaneous coronary interventions (PCI) are among the most frequently performed medical procedures. Like any invasive procedure, PCI carries a risk of periprocedural complications. Advances in non-invasive coronary artery imaging techniques offer hope for minimizing the risks associated with coronary angiography. However, complications such as dissections, vessel perforations, and access site-related issues remain inherent risks of the procedure [1, 2].
We present a case of iatrogenic dissection leading to occlusion of the left coronary artery (LCA) following diagnostic catheterization, successfully treated using the ping-pong technique, which is typically employed in the management of coronary artery perforations.
An 82-year-old female patient with a history of hypertension and type 2 diabetes was admitted to the cardiology department due to resting chest pain. Laboratory tests showed elevated troponin levels. Due to persistent symptoms, invasive coronary angiography was performed via the right radial artery. The angiogram of the right coronary artery showed no significant stenosis. After switching to a left catheter (Boston Impulse JL 4.0, 6F, inner diameter 0.056ʺ), angiography revealed a critical stenosis of the left anterior descending (LAD) artery. In a subsequent projection, complete occlusion of the LAD with dissection of the left main coronary artery (LMCA) was observed. The patient experienced chest pain and developed cardiogenic shock, leading to the diagnosis of iatrogenic LCA dissection (Figure 1).
Figure 1
A – Dissection of the LM and LAD with LAD occlusion, RAO 18°; cranial 27,1°; time: 10:01 AM. B – Guidewire passage into the true lumen of the LAD, RAO 13.2°; cranial 4.8°; time: 10:17 AM. C – Status after stenting of the LAD with visible flow in the vessel, RAO 18.3°; cranial 27.4°; time: 10:23 AM. D – Guiding catheter and diagnostic catheter in the LM ostium, RAO 22.2°; cranial 17.2°; time: 10:33 AM. E – Removal of the diagnostic catheter, LAO 12.5°; caudal 23.4°; time: 10:35 AM. F – Final effect, LAO 6.9°; caudal 16.1°; time: 11:05 AM
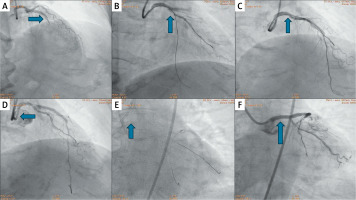
Management included vasopressor infusion. A polymer-jacketed guidewire (Fielder XT-A) was advanced through the diagnostic catheter. The side branch was secured with a second guidewire (Sion Blue). After successfully crossing into the true lumen, a drug-eluting stent (DES Biotronik Orsiro 3.0/35 mm) was implanted in the LAD. Post-stenting contrast injection confirmed restored flow in the LAD but persistent LMCA dissection. Due to the inability to advance a larger stent through the diagnostic catheter and to minimize procedural risks, the right femoral artery was punctured, and a guiding catheter (JL 4.0, 7F) was introduced into the LM ostium using the ping-pong technique. Following the path of the existing guidewires, two polymer-jacketed guidewires were placed into the LAD and the left circumflex artery (LCX). The diagnostic catheter and guidewires were then removed. With optimal access achieved, PCI of the LM and LAD was performed, and another drug-eluting stent (DES 3.5/28 mm) was implanted. The procedure was optimized using intravascular ultrasound (IVUS), confirming adequate stent apposition. The intervention was successfully completed with TIMI 3 flow.
The following day, PCI of the mid-LAD was performed with DES implantation. The patient remained stable during the subsequent days and was discharged on postoperative day 7 in good general condition.
The ping-pong technique played a crucial role in managing iatrogenic LMCA dissection, enabling rapid and safe intervention when standard single-access PCI was insufficient. A second femoral access and guiding catheter stabilized vascular access, improved maneuverability, and ensured optimal stent deployment. This novel use of the ping-pong technique – typically for coronary perforation – minimized procedural risk and prevented emergent surgery. IVUS optimization further enhanced stent apposition and safety. This case underscores the value of adapting interventional techniques to complex scenarios, improving PCI outcomes and patient safety [3–5].








