Introduction
Regardless of its effectiveness, veno-arterial extracorporeal membrane oxygenation (VA-ECMO) support is not a risk-free method. Its use is associated with high complication and mortality rates, especially in patients with comorbidities. The success of this method and prognosis depend on a number of factors, and correct patient selection and early recognition of predictors of method failure are essential to ensure optimal support outcomes. In addition to cardiorespiratory failure, the most frequently discussed predictors of VA-ECMO failure include the presence of other diseases, age, and the patient’s general health status before starting support.
Aim
The aim of this analysis was to evaluate the results and explore factors that might act as predictors of VA-ECMO failure as a method in critical patients. It focuses on clinical indicators and available anamnestic data that may facilitate early identification of patients at high risk of support failure, and possible intervention to ensure a better prognosis for patients with severe cardiovascular failure.
Material and methods
This is a retrospective single-center study conducted at the Cardiac Surgery Clinic of the University Hospital Olomouc within the ECMO center. A cohort of 124 patients supported by VA-ECMO with critical cardiorespiratory failure in the period 2012–2021 was analyzed. Ten patients were excluded from this cohort – patients supported with ECMO as a “back up” during extremely high-risk percutaneous interventions, especially procedures on the last patent coronary artery or due to technically unsuccessful cannulation. A series of 114 full support ECMO cases were analyzed.
Data collection and outcomes
The cohort included 114 patients supported between 2012 and 2021: 86 (75.4%) men and 28 (24.6%) women, median age 58 years (range: 8–81 years), median age 58 years (range: 8–77 years), median age 59.5 years (range: 18–81 years).
The distribution of patients according to the indications for VA-ECMO cardiopulmonary support is shown in the results.
Statistical analysis
The data are presented as percentages for categorical variables and as medians. Statistical analysis was conducted using IBM SPSS Statistics version 23 (Armonk, NY: IBM Corp. USA). The Mann-Whitney U test was used to analyze continuous variables in independent samples. Spearman correlation analysis and the χ2 test (Fisher’s exact test) were used. The level of statistical significance was set at p = 0.05 for all analyses. We test the normal distribution using the Shapiro-Wilk test. Figures were created using Microsoft Excel for Office 365 (Microsoft, Redmond, WA, USA).
Results
Indications
The indications for VA-ECMO support can be classically summarized as cardiorespiratory failure; however, the individual conditions encountered while determining the indications for support are listed below in Table I. The largest indication cluster is acute coronary syndrome, followed by heart failure after cardiotomy. Patients with unclear etiology of heart failure in critical condition formed a significant indication group. The statistical assessment of the association between hospital exit, 30-day, 90-day and 12-month survival with the indication diagnoses was performed. Statistical assessment of the association between hospital exit, 30-day, 90-day and 12 month survival with the indication diagnoses in our patient group did not show a correlation.
Table I
Summary of indications for VA-ECMO
Comorbidities
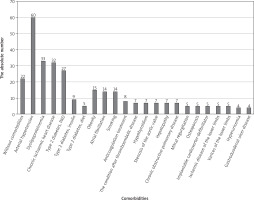
A list of diagnosed comorbidities in patients with severe cardiorespiratory failure at the time of the decision to provide VA-ECMO support is presented in Figure 1. The graph shows the nosological units and absolute numbers of comorbidities observed in patients for whom VA-ECMO support was indicated before the introduction of support itself.
Comorbidities with a frequency of 3 or less in the cohort are not listed in the chart (bronchial asthma, cardiomyopathy, rheumatoid arthritis, stroke, sleep apnea syndrome, chronic renal insufficiency, acute bronchitis, history of viral hepatitis, abdominal aortic aneurysm, deep vein thrombosis, Crohn’s morbus, acute lymphoblastic leukemia, pulmonary hypertension, acute myeloid leukemia after transplantation, history of splenectomy, alcoholism, malignancy removed within 30 days prior to ECMO, and some others).
Only 22 (19%) patients had no comorbidities in the whole cohort.
Statistical analysis was performed in terms of the correlation of each comorbidity with patient survival after VA-ECMO support.
Only hospital discharge and 12-month survival were borderline correlated with atrial fibrillation (significance level p = 0.049). Atrial fibrillation occurred significantly less frequently in patients who died during hospitalization than in patients who did not die during hospitalization. Atrial fibrillation occurred significantly more frequently in patients who survived 12 months than in patients who did not survive 12 months (significance level p = 0.049). Statistical processing of the total number of comorbidities in individual patients was performed – this parameter does not correlate with in-hospital mortality or 30-day, 90-day, or 12-month survival.
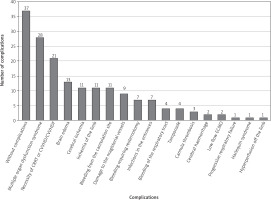
Complications
Complications occurred in 77 patients, which is almost 68% of the treated patients. Almost a quarter of patients had multiorgan dysfunction. One fifth of the patients required the use of an elimination method – continuous renal replacement therapy (CRRT), continuous veno-venous hemodialysis (CVVHD) or continuous veno-venosus hemodiafiltration (CVVHDF). Cerebral edema was diagnosed in 13 patients (14.4% of all complications related to the given support; in almost 93% of them, the outcome was fatal). Furthermore, limb ischemia accounted for almost 10% of major complications. The severity of this complication is mainly due to the risk of limb loss, which occurred in 2 of the 11 patients (18%). The full list of complications and the percentage distribution are shown in Figure 2.
No correlations of complication rates with in-hospital mortality and survival were demonstrated.
Analysis of complication rates in relation to hospital mortality and median survival (Fisher’s exact test) is shown in Table II.
Table II
Complication rates in relation to hospital mortality and survival
Statistical analysis
Statistical analysis of data on complications associated with VA-ECMO support showed that discharge on admission correlated with limb ischemia and infection on admission. A significantly lower incidence of both complications was found in patients who died during hospitalization. Survival at 30 days correlated with multiple organ dysfunction syndrome, brain edema, and infection on admission: patients who survived 30 days were found to have a significantly lower incidence of multiple organ dysfunction syndrome (MODS) and brain edema and a significantly higher incidence of infection on admission. Survival at 90 days correlated with infection on admission: patients who survived 90 days showed a significantly higher incidence. Survival at 12 months correlated with ischemia of the limb and infection on admission: patients who survived 12 months were shown to have a significantly higher incidence.
Assessment of the association between hospital exit, 30-day, 90-day and 12-month survival with the incidence of complications (Mann-Whitney U test) is shown in Table III.
Table III
Assessment of the association between hospital discharge, 30-day, 90-day, and 12-month survival with the incidence of complications
Discussion
Among the factors that affect patient prognosis and overload are the number and severity of comorbidities. These variables could in some way act as predictors of failure of the VA-ECMO method, possibly serving in combination with clinical prognostic factors at the time of decision-making in indications for VA-ECMO support.
In the original research papers in-hospital mortality rates of up to 70% were reported [1]. According to our viewpoint, here lies a certain margin in the change of in-hospital mortality among VA-ECMO-supported patients. An analysis from the original work involving 12,637 ECMO-supported patients using multivariable logistic regression and performing a multivariable linear regression analysis showed that 78% of patients developed at least one complication; it also showed that one complication was associated with a 165% increase in the odds of mortality. Two or three complications resulted in 375% or 627% higher odds of mortality [2].
Major complications such as bleeding and limb ischemia significantly prolong ICU and hospital stays and increase transfusion requirements [3]. Some reports describe vascular complications in up to 81% of patients [4].
In a retrospective study involving 367 patients, they analyzed subacute groin complications associated with ECMO cannulation. Overall, these complications occurred in 22.3% of ECMO patients, including 30.5% of seromas/lymphoceles, 39.0% of hematomas, 22.0% of infections, and 8.5% of unspecified files [5]. The results are comparable to our data.
A 2021 retrospective study reported life-threatening mechanical complications in 4.0% of cases. The most frequent was accidental decannulation (1.3%), followed by sudden drops in circuit flow (1.1%), pump failure (1.1%), circuit rupture (0.4%), and air in the circuit (0.2%) [6].
A 2020 meta-analysis showed an overall rate of neurological complications of 27% (95% CI: 0.17–0.39%), with 17% (95% CI: 0.12–0.23%) developing brain death [7]. A 2021 observational study reported neurological events in 37.5% of patients [8]. The total number of severe neurological complications in our study, including edema, cerebral ischemia and cerebral hemorrhage, was 22.8%.
In another retrospective cohort study from the same year, 15% of patients were diagnosed with non-hemorrhagic cerebral infarction during ECMO treatment, and in a stepwise multivariable analysis, VA ECMO showed the only independent risk association with the development of non-hemorrhagic cerebral infarction (p = 0.002, ΔR² = 0.098, odds ratio (OR) = 4.86 (95% CI: 1.8–13) [9].
According to a retrospective study that included 856 ECMO procedures, ECMO-related vascular and cerebrovascular complications were not associated with an increased risk of in-hospital death in adult patients [10].
Harlequin syndrome (also known as North-South syndrome) is a complication of VA ECMO that can occur when left ventricular function begins to recover [11]. This complication has been successfully managed by converting the ECMO circuit to a veno-venous-arterial (VV-A) configuration.
A retrospective analysis across three ICUs showed no difference in 90-day survival or bleeding incidence between patients receiving VA-ECMO after systemic thrombolysis and those without thrombolysis. The authors concluded that recent thrombolysis alone should not be viewed as a contraindication to VA-ECMO in high-risk pulmonary embolism [12].
There are elective VA-ECMO programs available at some centers. Prophylactic VA-ECMO is a viable strategy during high-risk PCI in patients deemed inoperable, if a clear clinical benefit is expected [13].
Regarding the correlation between complications and survival, we reasonably assume that the time factor plays an important role in the development of infectious complications in admissions, especially exposure to intensive care units and the development of antibiotic resistance. In the case of limb ischemia, we consider that a larger number of these complications are attributable to disconnected and surviving patients. Prevention of limb ischemia includes the addition of distal antegrade perfusion catheters [14]. Distal protection is routine in our center. The resulting decrease in cardiac output after decannulation plays a role in the perfusion of peripheral tissues of the affected limb, as do reconstructive procedures on the main vessels when support is disconnected. Conversely, patients who survived at least 30 days had fewer cases of MODS and cerebral edema because these complications are much more severe and often fatal. With their development, short- and medium-term survival rates decline.
This study provides important insights into the outcomes of using VA-ECMO in critically ill patients requiring external cardiopulmonary support, often in the pre-diagnostic and diagnostic stages within a single ECMO center over a period of 10 years, the development of method implementation, and the prospects of identifying predictors of method success or failure.
The present study is a single-center retrospective analysis with limited information on long-term postoperative survival. There is no detailed information on late complications.
Conclusions
Among the comorbidities in the study group, a correlation was found between atrial fibrillation and hospitalization mortality and 12-month survival: atrial fibrillation occurred significantly less frequently in patients who died during hospitalization than in patients who did not die during hospitalization. Also, atrial fibrillation occurred significantly more frequently in patients who survived 12 months than in patients who did not survive 12 months. There was no effect of the number of complications on in-hospital mortality and short- and medium-term survival.
There was a significantly lower incidence of end-limb ischemia infection at the cannulation site in patients who died during hospitalization. Survival at 30 days correlated with multiorgan dysfunction syndrome, cerebral edema and cannulation site infection: patients who survived 30 days were found to have a significantly lower incidence of multiorgan dysfunction syndrome and cerebral edema and a significantly higher incidence of cannulation site infection. Survival at 90 days correlated with the incidence of infection at the inlets: a significantly higher incidence of infection was found in patients who survived 90 days. Survival at 12 months correlated with limb ischemia and infection at admission: patients who survived 12 months were shown to have a significantly higher incidence.