Introduction
For patients with lung nodules (LNs), preoperative computed tomography (CT)-guided approaches are frequently used to localize these nodules prior to video-assisted thoracic surgery (VATS) [1–3]. When successful, preoperative LN localization can improve the accuracy of subsequent wedge resection procedures while reducing rates of conversion to thoracotomy [4]. CT-guided localization strategies are easy to perform, minimally invasive, and associated with high rates of success [5, 6]. However, CT-guided localization is associated with high rates of pneumothorax, particularly for patients undergoing CT-guided hook-wire localization, who can exhibit pneumothorax rates of up to 48.5% [7].
Bronchoscopic dye localization has been established as a promising alternative approach to preoperative localization associated with lower rates of complications including lung hemorrhage and pneumothorax relative to percutaneous approaches [8, 9]. Bronchoscopic dye localization is generally conducted via either augmented fluoroscopic bronchoscopy (AFB) or electromagnetic navigation bronchoscopy (ENB) [10–12]. While several meta-analyses have examined outcomes and other parameters associated with CT-guided or bronchoscopic approaches to LN localization [5, 10], these were generally single-arm meta-analyses exhibiting high levels of heterogeneity and a corresponding risk of bias [5, 10]. Meta-analyses directly comparing the relative clinical efficacy of different LN localization strategies are required.
Aim
The present meta-analysis was developed to examine the relative efficacy and safety of CT-guided and bronchoscopic LN localization strategies.
Material and methods
Study selection
The present meta-analysis was performed following Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [13]. Searching for the relevant studies published in May 2022 was carried out by the PubMed, Cochrane Library, Embase, and Wanfang databases with the following search strategy: ((((computed tomography) OR (CT)) AND ((bronchoscope) OR (bronchoscopy))) AND (localization)) AND ((lung nodule) OR (pulmonary nodule)). This meta-analysis has been registered in INPLASY.COM (No. INPLASY202260068).
Studies meeting the following criteria were eligible for inclusion:
Study types: comparative studies;
Diseases: LNs patients;
Intervention type: CT-guided vs. bronchoscopic localization of LNs;
Languages: no limitations.
This study excluded single-arm studies, non-human studies, case reports, and reviews.
Study selection
Two investigators independently performed all study selection procedures, with disagreements being resolved through discussion with a third investigator. Following initial title and abstract screening, potentially relevant studies were then subjected to full-text review.
Data extraction
First author, publication year, country/region, study design, study quality, number of patients, number of lymph nodes, age, gender ratios, LN diameter, LN depth, localization technical success rates, complication rates, localization time, VATS time, and postoperative hospitalization time were extracted from relevant studies.
Assessment of study quality
Assessment for the randomized controlled trials was carried out using the Cochrane risk-of-bias tool and were assigned a high, low, or unclear risk of bias for each of the following: detection, performance, attrition, reporting, selection, and other bias.
The Newcastle-Ottawa scale (NOS) was used to evaluate all non-RCT studies by assigning them points based upon selection, comparability, and outcome criteria (4, 2, and 3 points, respectively). A study was regarded as outstanding quality if it had an NOS score ≥ 7.
Definitions
Localization time was defined as the time from patients lying on the bed of the CT scanner/bronchoscopy to completing injection of the localization materials [14, 15]. The VATS time was defined as the time from first incision to wound closure [16]. The postoperative hospitalization time was defined as the time from completing VATS to discharge. Pulmonary hemorrhage was defined as either intrapulmonary bleeding or airway bleeding due to the localization procedure [10]. Intrapulmonary bleeding was defined as an emerging area of consolidation developed in the track of the puncture in the lung parenchyma [10]. Airway bleeding was defined as bleeding seen in the airway during the bronchoscopic procedure [10].
Statistical analysis
Data from all endpoints were pooled using RevMan v5.3. Mean differences (MDs) with 95% confidence intervals (CIs) were used for the analysis of continuous variables, whereas odds ratios (ORs) with 95% CIs were used for the analysis of categorical variables. The heterogeneity of the study was evaluated using the I2 statistic and Q test, with I2 > 50% denoting significant heterogeneity. Through the random-effects models, the pooled analyses in the context of significant heterogeneity were conducted, whereas fixed-effects models were used when no significant heterogeneity was present. A leave-one-out approach was used to conduct sensitivity analyses aimed at identifying studies that contributed to detected heterogeneity. The risk of publication bias was assessed using funnel plots and Egger’s test in Stata v 12.0.
Results
Study selection
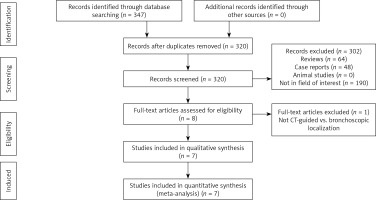
In all, 347 potentially relevant studies were found by the initial search strategy, of which seven were included in the final meta-analysis after a full-text review [14–20]. Figure 1 outlines the study selection process in detail. All 7 studies were retrospective in design, with 2 having employed a propensity score-matching (PSM) approach [16, 19]. All 7 studies exhibited a NOS scale of 8 consistent with their being high-quality studies (Table I).
Table I
Baseline data of the included studies
| No. | First author | Year | Country/area | Design | NOS |
|---|---|---|---|---|---|
| 1 | Anayama [14] | 2018 | Japan | Retrospective | 8 |
| 2 | Anayama [15] | 2021 | Japan | Retrospective | 8 |
| 3 | Kuo [16] | 2019 | Taiwan | PSM-Retrospective | 8 |
| 4 | Song [17] | 2019 | China | Retrospective | 8 |
| 5 | Tian [18] | 2020 | China | Retrospective | 8 |
| 6 | Yang [19] | 2020 | Taiwan | PSM-Retrospective | 8 |
| 7 | Yang [20] | 2021 | China | Retrospective | 8 |
These 7 studies included 321 patients with 353 LNs that underwent CT-guided localization and 220 patients with 244 LNs that underwent bronchoscopic localization (Table II). In 5 studies an ENB localization approach was employed [14, 16–18, 20], while 2 studies utilized an AFB localization approach [15, 19]. Indocyanine green (IG) was used as a localization material in 3 studies [14, 15, 20], while 3 used patent blue (PB) [16, 18, 19], and 1 employed a hook-wire approach in the CT group and PB in the bronchoscopic group [17]. The differences were not significant in age, gender ratios, LN diameter, LN depth, or other baseline data when comparing the CT and bronchoscopic groups in the included studies. The raw data of the localization and VATS related outcomes are shown in Table III.
Table II
Baseline data of patients in the included studies
| Author | Groups | Bronchoscopic types | Localization material | Patients | Nodules | Age | Gender (M/F) | Diameter [mm] | Nodule depth [mm] |
|---|---|---|---|---|---|---|---|---|---|
| Anayama [14] | CT | ENB | Indocyanine green | 15 | 16 | 61.5 y | 10/5 | 10 | 9.9 |
| Bronchoscopic | Indocyanine green | 22 | 23 | 64.4 y | 13/9 | 9.2 | 9.8 | ||
| Anayama [15] | CT | AFB | Indocyanine green | 15 | 16 | 65.0 y | 10/5 | 10 | 9.9 |
| Bronchoscopic | Indocyanine green | 24 | 30 | 66.0 y | 14/10 | 9.2 | 9.8 | ||
| Kuo [16] | CT | ENB | Patent blue | 30 | 48 | 56.3 y | 24/6 | 11 | 19 |
| Bronchoscopic | Patent blue | 15 | 24 | 54.4 y | 10/5 | 10 | 18 | ||
| Song [17] | CT | ENB | Hook-wire | 61 | 64 | 58.5 y | 24/37 | 10.8 | 15.1 |
| Bronchoscopic | Patent blue | 65 | 65 | 59.7 y | 29/36 | 11.3 | 14.9 | ||
| Tian [18] | CT | ENB | Patent blue | 105 | 105 | Not given | 57/48 | Not given | Not given |
| Bronchoscopic | Patent blue | 52 | 52 | Not given | 31/21 | Not given | Not given | ||
| Yang [19] | CT | AFB | Patent blue | 60 | 69 | 55.5 y | 28/32 | 9.7 | 17.4 |
| Bronchoscopic | Patent blue | 30 | 35 | 56.5 y | 13/17 | 10.8 | 17.5 | ||
| Yang [20] | CT | ENB | Indocyanine green | 35 | 35 | 55 y | 9/26 | 7 | 8.2 |
| Bronchoscopic | Indocyanine green | 12 | 15 | 56 y | 4/8 | 11 | 12.5 |
Table III
Raw data of the localization and VATS related outcomes
| Author | Groups | Technical success of localization | Pneumothorax | Pulmonary hemorrhage | Localization time [min] | VATS time [min] | Postoperative hospitalization [days] |
|---|---|---|---|---|---|---|---|
| Anayama [14] | CT | 100% | 20% | Not given | Not given | Not given | Not given |
| Bronchoscopic | 90.9% | 0% | Not given | Not given | Not given | Not given | |
| Anayama [15] | CT | 93.8% | 20% | Not given | Not given | Not given | Not given |
| Bronchoscopic | 93.3% | 0% | Not given | Not given | Not given | Not given | |
| Kuo [16] | CT | 90% | 36.7% | 43.3% | 26.3 ±14.0 | 110.7 ±21.3 | 2.7 ±0.8 |
| Bronchoscopic | 93.3% | 6.7% | 20% | 21.8 ±12.5 | 121.8 ±41.5 | 2.33 ±0.8 | |
| Song [17] | CT | 96.9% | 1.7% | Not given | 20.4 ±3.3 | Not given | 4.8 ±1.8 |
| Bronchoscopic | 100% | 0% | Not given | 17.2 ±4.2 | Not given | 4.8 ±1.6 | |
| Tian [18] | CT | 94.3% | 11.4% | 1% | 15.15 ±3.7 | Not given | Not given |
| Bronchoscopic | 100% | 0% | 0% | 21.29 ±4 | Not given | Not given | |
| Yang [19] | CT | 95.0% | 16.7% | 26.7% | 21.4 ±12.5 | 77.2 ±46.5 | 3.1 ±2.2 |
| Bronchoscopic | 96.7% | 0% | 3.3% | 24.1 ±8.3 | 96.1 ±43.4 | 4.1 ±1.7 | |
| Yang [20] | CT | 94.3% | 14.2% | Not given | Not given | Not given | Not given |
| Bronchoscopic | 100% | 0% | Not given | Not given | Not given | Not given |
Localization technical success rates
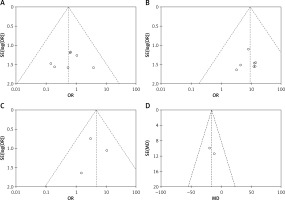
Localization technical success rates were reported in all 7 studies, with these rates being comparable in the CT and bronchoscopic groups (94.8% and 97.3%, p = 0.20, Figure 2 A). The heterogeneity was low in these included studies (I2 = 0%). Funnel plots and Egger’s test (p = 0.917) indicated a low risk of publication bias for this endpoint (Figure 3 A).
Pneumothorax
All seven studies reported pneumothorax rates, and pooled analysis revealed that these rates were considerably lower in the bronchoscopic group than in the CT group (0.5% vs. 14.0%, p < 0.001, Figure 2 B). These studies exhibited no significant heterogeneity (I2 = 0%). Funnel plots and Egger’s test (p = 0.201) indicated a low risk of publication bias for this endpoint (Figure 3 B).
Pulmonary hemorrhage
In three of the included studies, pulmonary hemorrhage rates were reported [16, 18, 19], with pooled analyses revealing these rates to be significantly lower in the bronchoscopic group relative to the CT group (4.1% vs. 15.4%, p = 0.005, Figure 2 C). No significant heterogeneity was detected among these studies (I2 = 0%). Funnel plots and Egger’s test (p = 0.601) indicated a low risk of publication bias for this endpoint (Figure 3 C).
Localization time
The localization time was reported in 4 of the included studies [16–20], with pooled analyses revealing no significant differences in this duration between CT and bronchoscopic groups (MD = –0.62, 95% CI: –6.96–5.72, p = 0.20, Figure 2 D). These studies exhibited a high degree of heterogeneity for this endpoint (I2 = 97%). While not all studies were located within the generated funnel plot, Egger’s test did not reveal any evidence of significant publication bias (p = 0.818). Sensitivity analyses were unable to identify sources of heterogeneity for this endpoint.
VATS time
In two of the included studies, the VATS time was reported [16, 19], with pooled analyses revealing this duration to be significantly shorter in the CT group than the bronchoscopic group (MD = –15.53, 95% CI: –30.21–0.85, p = 0.04, Figure 2 E). The observed heterogeneity among these studies was not significant (I2 = 0%). Funnel plots indicated a low risk of publication bias for this endpoint (Figure 3 D).
Postoperative hospitalization time
In three studies, the postoperative hospitalization time was reported [16, 17, 19], with pooled analyses revealing no difference in this duration between the CT and bronchoscopic groups (MD = –0.14, 95% CI: –0.86–0.57, p = 0.69, Figure 2 F). These studies exhibited a high degree of heterogeneity for this endpoint (I2 = 74%). While not all studies were located within the generated funnel plot, Egger’s test did not reveal any evidence of significant publication bias (p = 0.725).
An analysis of the sensitivity revealed that the article published by Yang et al. [19] was the primary source of heterogeneity. However, the pooled duration of postoperative hospitalization remained still comparable between the CT and bronchoscopic groups (p = 0.26) after removing this study [19].
Subgroup analyses based on ENB versus CT guidance
Subgroup analyses comparing ENB and CT-guided localization procedures did not detect any significant differences between these two groups with respect to pooled localization procedure duration, localization technical success rates, or duration of postoperative hospitalization (Table IV). In the ENB group, pooled pneumothorax and pulmonary hemorrhage rates were both significantly lower relative to the CT group (p = 0.001 and p = 0.02).
Table IV
Subgroup analyses based on ENB vs. CT guidance
Subgroup analyses based on AFB versus CT guidance
In pooled localization technical success rates, subgroup analyses comparing AFB and CT-guided localization similarly revealed no significant differences between these two groups (p = 0.81; Table V). The AFB group exhibited significantly lower pneumothorax rates than the CT group (p = 0.01).
Subgroup analyses based on IG localization material
Subgroup analyses performed for studies using IG as a localization material revealed comparable pooled localization technical success rates in the CT and bronchoscopic groups (p = 0.72; Table VI). The bronchoscopic group exhibited significantly lower pneumothorax rates relative to the CT group (p = 0.02).
Subgroup analyses based on PB localization material
Subgroup analyses performed for studies using PB as a localization material revealed comparable pooled localization procedure duration, localization technical success rates, and postoperative hospitalization duration values when comparing the CT and bronchoscopic groups (Table VII). Pooled pneumothorax and pulmonary hemorrhage rates were significantly lower in the bronchoscopic group than in the CT group (p = 0.001 and p = 0.005).
Table VII
Subgroup analyses based on PB localization material
Discussion
The present meta-analysis compared the relative safety and efficacy of CT-guided and bronchoscopic LN localization procedures. As the pooled technical success rates were similarly high for both of these approaches, this suggests that these two strategies can be reliably used for the preoperative localization of LNs.
A range of localization materials can be used to facilitate CT-guided localization, including radiolabeling materials, liquids, hook-wires, and coils [21–24]. In contrast, bronchoscopic localization strategies can only utilize liquid-based materials, including IG and PB [10]. While these liquid localization materials are limited by their rapid diffusion rates, the fact that bronchoscopic localization and subsequent VATS procedures can be conducted in a single room in the form of a one-stage operation can ensure high rates of successful LN localization [17]. The comparable localization procedure duration for both the CT and bronchoscopic groups further suggests that the operative difficulty for these two procedures is similar.
Pooled successful localization rates and localization procedure duration values were comparable in all subgroup analyses when comparing the CT and bronchoscopic groups. These results suggest that the different bronchoscopic techniques or localization materials employed had no impact on either of these procedure-related outcomes.
Localization-related complications were key endpoints in the present analyses. Overall, bronchoscopic localization was associated with a better safety profile relative to CT-guided localization. This is consistent with the fact that bronchoscopic procedures are less invasive than CT-guided interventional procedures [12]. Moreover, all bronchoscopic procedures can be performed in the operating room, thus reducing the interval between localization and VATS. In the CT group, in contrast, patients had to undergo transportation from the CT room to the operating room, increasing the risk of complications [18]. Subgroup analyses suggested that both ENB and AFB LN localization procedures exhibited better safety profiles than CT-guided localization procedures.
The pooled VATS duration for patients who underwent CT-guided localization was shorter in the present meta-analysis. However, these analyses were based on data from just two studies, suggesting that further studies of this endpoint are warranted. As the postoperative hospitalization duration was comparable for both of these localization approaches, these techniques had no impact on post-VATS recovery.
This analysis has some limitations. First, each of the included studies used a retrospective design. While two of these studies employed a PSM approach, the resultant data were still of a weaker level of evidence than that associated with data derived from RCTs. Second, one of the included studies compared CT-guided hook-wire localization and bronchoscopic PB localization [17]. The inconsistencies in localization materials may have contributed to selection bias, thus affecting the resultant data. Third, while these studies were published in different countries and regions, all were from Asian nations, underscoring the need for additional research conducted on other continents.