Introduction
Obesity has been recognised by the World Health Organization (WHO) as a disease of civilisation, and the fight against it is now one of the most important health policy goals worldwide. Obesity, defined by the body mass index (BMI) above 30 kg/m2, according to data from 2020 affects 21% of women and 28% of men in Poland; class II obesity (BMI > 35 kg/m2) [1] affects more than 600,000 inhabitants of Poland and meets the criteria for selection for bariatric surgery, the only method with proven effectiveness, confirmed by worldwide organisations bringing together specialists who treat patients with pathological obesity. The performance of approximately 6,000 to 7,000 bariatric operations per year in Poland indicates that the efforts made to combat this epidemic are far from sufficient.
As part of the prevention and treatment of obesity and its consequences, a number of treatment and prevention initiatives have been launched. One of these is a multi-centre nationwide pilot programme, Comprehensive Specialist Care – Bariatrics (KOS-BAR) – developed substantively by experts in bariatric surgery, gathered in a working group around the Faculty of Health Sciences at Lazarski University, who have developed a multidisciplinary comprehensive model of care for patients with pathological obesity. The project has gained approval from the Ministry of Health and has been implemented in 15 centres in Poland which declare that they meet the requirements of the programme based on the 2020 Polish bariatric standard [2].
The programme covers patients aged 18 to 65 years with a diagnosis of obesity due to excessive energy intake (E66 according to ICD-10). The inclusion criterion for the programme is a BMI ≥ 40 kg/m2, and a BMI of 35–40 kg/m2 for those in whom surgically induced weight reduction has the potential to improve obesity-related diseases. In the KOS-BAR programme, the patient receives comprehensive care at all stages of treatment: pre-operative care covers 3–6 months, during which the patient is prepared clinically and psychologically for bariatric surgery. The first module of the programme consists of the initial selection for bariatric surgery, nutritional, laboratory and hormonal tests, imaging studies, and consultation with a surgeon, internist, anaesthetist, dietician and psychologist.
After a preparatory period in which the patient should reduce their body weight by 10% of the initial weight, the patient is scheduled for surgery, after which he or she is included in the post-operative care process, the main goals of which are behavioural activation, physiotherapist care and dietetics to improve performance and maintain the reduced body weight as permanently as possible.
Another disease of civilisation, the importance of which is increasingly highlighted in the world today, is depression. Given the serious consequences of depressive disorders related to functional impairment, disability, increased mortality, and worsening of comorbidities, correlations between the incidence of specific diseases of civilisation, including obesity and depression, are increasingly becoming a subject of study. Milaneschi et al. summarised the mechanisms common to depression and obesity. Both diseases involve chronic stress, chronic inflammation, dysfunction of the hypothalamic-pituitary-adrenal axis, abnormalities in the regulation of carbohydrate metabolism by leptin and insulin, and common genetic, environmental, and socioeconomic factors such as poor diet, sedentary lifestyle and poor economic circumstances. The role of an inappropriate microbiome in the pathogenesis of obesity and depression is also increasingly pointed out [3, 4].
A study by Kalarchian et al. found that approximately 60% of patients selected for bariatric surgery had a history of mental disorders, and 38% had them at the time of selection [5].
Investigating the interplay between obesity and depression showed that depressive disorders were present in 19% of patients selected for bariatric surgery. The effect of preoperative depression on weight loss outcome was inconclusive. Depressive disorders occurring after bariatric surgery definitely had a negative impact on the outcome of this treatment.
In the context of an eating disorder diagnosis, approximately 16% of patients eligible for surgery met criteria for an eating disorder, mainly in the form of paroxysmal overeating. Effective treatment of these disorders is crucial to reduce preoperative weight and maintain the effect of surgery [5].
Aim
The aim of this study was to assess the prevalence of mental disorders diagnosed de novo, verify the diagnosis and evaluate the efficacy of pharmacotherapy used in patients remaining under psychiatric treatment, selected for bariatric surgery under the KOS-BAR programme.
Taking into account the above literature data as well as the multidisciplinary evaluation including psychiatric evaluation in a group of patients with unsuccessful bariatric surgery, Module I of the KOS-BAR project was enriched with psychiatric evaluation and, if indicated, pharmacological treatment and psychotherapeutic care. The aim of these interventions is to:
– identify patients who are at increased risk related to a potential lack of cooperation after treatment,
– optimise the process related to the inclusion of antidepressant pharmacotherapy in patients with a diagnosis of affective disorders,
– provide patients access to group psychotherapy within the cognitive-behavioural approach,
– draw particular attention to the group of patients who, on psychiatric examination, present relative contraindications to treatment and to extend to them care aimed at eliminating or reducing these contraindications,
– cancel or defer bariatric surgery among patients with a mental disorder not recognised at the initial selection.
Material and methods
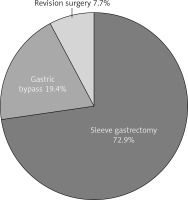
It must be noted that this study is focused on assessing psychiatric diseases in a population of patients with obesity selected for bariatric surgery. As a result, it concentrates on the population distribution of such diseases. Because this is a pilot study, not enough data to seek differences between sexes, age and other characteristics were gathered. This should be corrected when new data are acquired; the population will also be extended by a subpopulation of patients aged between 16 and 18 years. As this is a population study, comparing the study with another population of patients, i.e. with eating disorders but without obesity, is pointless from the point of view of a surgeon and doubtful from the view of a psychiatrist, as there are too many differences between the groups in the genesis, course and influence on physiology and neuronal pathways. The study has so far enrolled 180 patients, over 18 years of age, with a BMI > 40 kg/m2 or a BMI of 35–40 kg/m2, in whom surgically induced weight reduction may bring improvement in obesity-related diseases. The selection for surgical treatment followed the Polish standard of care for bariatric patients SChMiB – TChP [6, 7] (Figure 1). Psychiatric factors excluding patients from surgery were acute psychosis, acute depressive episode, unstable bipolar affective disorder, unregulated eating disorder, suicidal thoughts and intentions and active substance abuse. 131 persons were selected for sleeve gastrectomy (LSG), and the remaining 35 for gastric by-pass, of whom 30 were selected for one anastomosis gastric by-pass (OAGB), and 5 for Roux-en-Y gastric by-pass (RYGB). Of the patients eligible for surgery, 14 had previously undergone LSG at other centres and were referred for revision surgery (R-OAGB) due to significant weight gain. It must be noted that insufficient weight loss and recurrence of obesity are the most common reasons for bariatric resurgery [8]. Patients under 40 years of age with undeveloped metabolic concomitant disease and patients with a BMI greater than 50 kg/m2 were eligible for LSG. Patients diagnosed with type 2 diabetes mellitus (T2DM) or gastro-oesophageal reflux refractory to conservative treatment were offered OAGB. Patients diagnosed with advanced reflux lesions, including Barrett’s oesophagus, were referred for RYGB [9].
As part of the selection for surgery, all patients at our centre were cared for by a psychiatrist who was included in the preparatory module of KOS-BAR I.
The psychiatric examination focused on the current assessment of the mental state with the aim of diagnosing patients not previously under psychiatric treatment (de novo diagnosis), optimising the treatment of patients under the care of a psychiatrist, as well as providing long-term care for patients who have been on antidepressant pharmacotherapy in the past and are currently in full symptomatic remission.
The assessment of the mental state, in addition to the currently collected history, included an analysis of the available medical records of psychiatric treatment and was verified by supplementing the interview with psychometric scales: MADRS and the Beck scale for assessing the severity of depressive symptoms, the Strelau Temperament Questionnaire, and the Barratt Impulsivity Scale.
Patients meeting criteria for depressive disorders were started on pharmacotherapy with drugs from the serotonin reuptake inhibitor (SSRI) group, most commonly fluoxetine, due to its positive effect and registration with co-occurring compulsive eating disorders.
In the case of ineffectiveness of pharmacotherapy with SSRIs, it was decided to include bupropion, a norepinephrine and dopamine reuptake inhibitor, which, by affecting the activation of the reward system, reduces the need for emotional eating in addition to its antidepressant effect.
For patients meeting criteria for eating disorders, a six-session psychotherapeutic protocol in the cognitive-behavioural approach was applied, aiming to identify dysfunctional thoughts and beliefs related to eating, encourage behavioural change related to better control of emotions that trigger compulsive eating attacks, work with cognitive distortions and build a more adaptive pattern of perception of one’s body.
Results
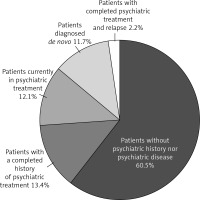
Among the 180 patients studied to date, 108 (60%) are patients who have never been under the care of a psychiatrist before and who were not diagnosed with any mental illness or disorder on the day of the examination. The remaining 72 (40%) patients were patients with a history of psychiatric treatment or previously untreated patients who were diagnosed with a mental disorder during the psychiatric consultation in the KOS-BAR programme (Figure 2).
In the group of patients requiring psychiatric treatment, we distinguished four subgroups:
patients with a completed history of psychiatric treatment in whom there was no indication of any psychiatric diagnosis on the day of selection – 24 patients (13.3%) (Figure 3),
patients currently under psychiatric treatment – 23 patients (12.7%) (Figure 4),
patients with a history of completed psychiatric treatment who were diagnosed with relapse or had another psychiatric diagnosis on the day of the examination – 4 patients (2.2%) (Figure 5),
patients who had never received psychiatric treatment before and were diagnosed with a mental disorder for the first time (de novo diagnosis) – 21 patients (11.6%) (Figure 6).
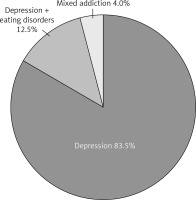
In the first group of patients, 20 patients were diagnosed with a depressive episode (83.3%), three of them had a depressive episode co-occurring with an eating disorder diagnosis (12.5%), and 1 (4%) patient remained in pharmacological and psychotherapeutic treatment for mixed addiction.
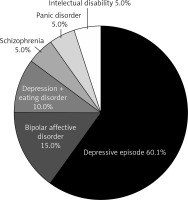
In the group of patients who remained in psychiatric treatment during the selection process for surgery, 12 (52.2%) patients were diagnosed with a depressive episode, 3 (13%) patients were treated for bipolar affective disorder, and 3 (13%) patients remained in treatment for sleep disorders. Two (8.7%) patients had a co-occurring depressive episode with an eating disorder diagnosis. One (4.3%) patient had been treated for schizophrenia for years (currently in complete remission of psychotic symptoms), a single patient (4.3%) was diagnosed with paroxysmal anxiety syndrome, and 1 (4.3%) patient had a moderate intellectual disability.
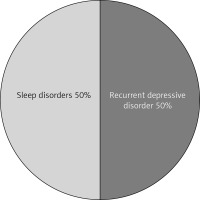
In the third group of patients, 2 (50%) patients had a diagnosis of recurrent depressive disorder, while 2 (50%) had been on pharmacotherapy with antidepressants in the past and were now eligible for sleep disorder treatment.
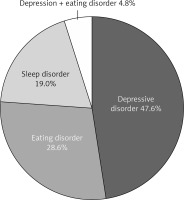
In the group of patients who had never received psychiatric treatment before, 10 (47.6%) patients were diagnosed with a depressive episode. Six (28.6%) patients had an eating disorder, including 4 patients with compulsive eating syndrome without compensatory behaviour, 1 patient meeting criteria for bulimia, and 1 for night eating syndrome (NES). In this group of patients, 4 (19%) had a diagnosis of sleep disorders, and 1 (4.7%) patient had a dual diagnosis of a depressive episode and compulsive eating syndrome.
The prevalence of suicidal thoughts, which were present in 15 (8.3%) patients, and self-injurious behaviour, which was present in 7 (3.9%) patients, was also assessed in the study group.
When selecting patients for surgery under the KOS-BAR programme, the most interesting observation, which may make a significant difference in thinking about the long-term prospect of maintaining a lower weight, is that in the group of 14 patients selected for revision surgery due to insufficient success of LSG, the vast majority (57.1% ) of them had indications for psychiatric treatment due to a diagnosis of depressive disorder or compulsive eating syndrome. This observation is consistent with the authors’ as yet unpublished findings of studies in a group of patients with unsuccessful bariatric surgery who developed significant weight gain 2 to 5 years after surgery, with a previously unidentified psychiatric factor being the main determinant of weight gain.
Discussion
The prevalence of mental disorders in the group of people selected for bariatric surgery at our centre does not differ significantly from that currently reported worldwide [5]. Affective disorders in the preoperative period are associated with less motivation in preparation for surgery and a longer period of time needed for the 10% of baseline weight reduction required for selection. In the post-operative period, patients present poorer co-operation, have more difficulty adhering to dietary rules and present inappropriate strategies for emotion regulation, often resulting in achieving mood improvement through eating.
Morgan et al. found that the use of psychiatric counselling increased in patients after bariatric surgery especially in those who had previously been diagnosed with a mental disorder or were experiencing complications after surgery [10].
The risk of developing or relapsing into depression may be related to unfulfilled expectations of the effects of surgery, intolerance to lifestyle changes after surgery, lack of effective mood regulation mechanisms after cessation of overeating, or changes in the absorption and action of psychotropic drugs (mainly sertraline, duloxetine or lithium) [11–14].
In the group of young adults undergoing bariatric surgery, several literature reports indicate an increased risk of suicidal thoughts. After the case analysis, we note that these reports relate to a group of patients who, prior to being found eligible for bariatric surgery, had been treated for affective disorders, secondary to which pharmacokinetic changes in the pharmacotherapy used may have had a significant impact on the decompensation of the mental state in the postoperative period [15–17].
Our previous observations and experience in a group of patients with obesity indicate that surgery should be postponed in patients who have not yet achieved remission of depressive symptoms, in whom pharmacological treatment should be potentialised, and in a group of patients with a diagnosis of eating disorders, psychotherapeutic care should be provided.
There is a major difficulty in assessing readiness for treatment in the group of patients with a diagnosis of substance abuse. Active addiction is a contraindication to surgery because of the risk of postoperative complications and lack of therapeutic cooperation, and this approach is not very controversial [18, 19].
A more difficult group is that of addicted patients who are abstinent at the time of selection. Difficulties in emotion regulation mechanisms are particularly common among these patients and may be indirectly associated with a higher risk of obesity and/or addiction relapse in the postoperative period. There also appears to be a significantly higher risk of cross-addiction in these patients.
One person in the study group was diagnosed with intellectual disability. Cognitive impairment to the extent that it significantly impedes therapeutic cooperation may be a relative contraindication to bariatric surgery due to the high risk of postoperative complications and reduction in treatment efficacy. Selecting such a patient for surgery requires a careful assessment of the social support and assistance that can be provided to such a person in terms of therapeutic compliance. In such cases, a thorough assessment of auto- and hetero-aggressive behaviour, use of psychoactive substances and verification of the pharmacotherapy in use is essential. Due to doubts about independent functioning after surgery, the patient was referred to a multidisciplinary consortium to assess whether the potential risks arising from reduced cognitive function outweigh the expected metabolic benefits of surgery.
Auto- and hetero-aggressive behaviour alone is a serious problem and a contraindication to bariatric surgery. Suicidal thoughts and intentions can be immediately life-threatening and require immediate attention. All cases of suicidal tendencies identified in patients in the study group were related to the past and no safety hazard was found. Self-aggressive behaviour (self-harm) is usually not life-threatening but is a predictor of inadequate therapeutic cooperation both before and after treatment. These behaviours, like suicidal thoughts and intentions, are usually a manifestation of unstable mental disorders. Because of the particular importance of these behaviours, we decided to introduce a separate register of them.
In the group of patients studied, 3 were identified as being treated for bipolar affective disorder. All these patients remained in stable remission, which was not a contraindication to bariatric surgery.
Worth noting is the large proportion of patients following sleeve gastrectomy currently referred for revision bariatric surgery due to inadequate weight reduction or to weight regain, who require psychiatric care. One of the most potent mechanisms of bariatric surgery is the induction of a metabolic effect in which, due to a change in the anatomy of the gastrointestinal tract, there is a change in the activity of hormones secreted by the stomach or small intestine, which are potent signals that influence the anorexigenic responses taking place in the hypothalamic centre of hunger and satiety regulation [20, 21]. Despite such a strong mechanism, some patients ignore the signal coming from the gastrointestinal tract, and one of the most common factors influencing this is compulsive reaching for food as a mechanism of abnormal regulation of emotions, tension reduction, or the need to improve mood rather than the need to satisfy hunger. Based on observations in a group of patients with insufficient success of bariatric surgery, it seems very important to capture patients in whom the mechanism of emotional eating prevails over the classical one related to the satisfaction of a physiological need. An individualised model of psychiatric care in this group of patients, consisting of the inclusion of pharmacotherapy and support by the process of psychotherapy in the cognitive-behavioural approach, seems to be one of the important factors in the process of achieving readiness for bariatric surgery as well as minimising the risk of failure.
To date, the selection procedure for bariatric surgery has focused on consultation with a psychologist to exclude acute psychotic conditions that are an absolute contraindication to surgery. Psychiatric examination was not a routine/compulsory part of this procedure. Our understanding of the role of the psychiatrist in the team treating the obese patient goes beyond the standard assessment of contraindications to bariatric surgery. The psychiatrist’s role is also to identify factors that trigger or exacerbate obesity (anorexia as a symptom of a mental disorder or an adverse effect of psychotropic medication; eating as a mechanism of emotion and mood regulation) and to assess the individual patient’s needs affecting the effectiveness of bariatric surgery (optimising pharmacotherapy, adding psychotherapy, improving cognitive functions, stabilising mood). Our approach is consistent with how the role of the psychiatrist is currently perceived in the interdisciplinary team treating people with obesity [22–24].
Long-term obesity outcomes are clearly better in patients receiving psychiatric treatment [25], which provides an additional argument for the validity of our modification of the standard of care for patients with obesity. The effects of including psychiatric treatment in the comprehensive long-term care for obese patients in the COSBAR programme will be the object of further research at our centre. This is the first publication based on a relatively large group of Polish patients and concerns an important pilot programme which, if evaluated positively, can be implemented as a regular comprehensive obesity care service.
Conclusions
Given the prevalence of mental disorders in the group of patients selected for bariatric surgery, psychiatric care is an important link in the process of comprehensive treatment of obesity and should be included in the assumptions of standards describing the management of patients with pathological obesity.
Early diagnosis of patients requiring pharmacological treatment, as well as greater psychotherapeutic attention in preparation for surgery, may contribute to minimising the risk of bariatric surgery failure.
It seems necessary to include patients undergoing revision surgery in an individualised preparation model, taking into account personality and temperamental characteristics, which may be among the important factors, alongside metabolic factors, contributing to the failure of the first bariatric surgery.
Among patients with a potential risk of failure of bariatric surgery, close collaboration of a multidisciplinary team, reinforcing a full, coherent agreement on the selection of these patients for surgery, seems very important.
Establishing a definitive model of comprehensive specialist care which comprises the role of the psychiatrist requires further follow-up of patients within the KOS-BAR group 2 to 5 years after surgery.