Pulmonary artery aneurysms have proven to be a very rare entity. The association with structural cardiac abnormalities, structural vascular abnormalities, pulmonary hypertension, vasculitis and infection has been noted. Surgical intervention of symptomatic aneurysms is recommended. Here, we report a case of pulmonary artery aneurysm undergoing surgery in our center and a brief review of the existing literature on this topic. The case concerns a 56-year-old patient with a diagnosis of pseudoaneurysm at the origin of the pulmonary trunk, sacciform aneurysm of the common trunk-pulmonary artery left branch (diameters (dt) lateral-lateral (LL) 58 mm × antero-posterior (AP) 67 mm × cranial-caudal (CC) 65 mm) and ectasia of the right branch (34.5 × 30 mm).
Pulmonary artery (PA) and trunk aneurysms are a rare entity. They have been associated with structural cardiac anomalies (in particular congenital heart disease), structural vascular anomalies, vasculitis, pulmonary hypertension and infection, but idiopathic pulmonary artery aneurysms (PAA) have also been identified. Recently, the reports and identification of these clinical entities have increased thanks to advances in diagnostic imaging methods such as computed tomography (CT), magnetic resonance imaging (MRI) and echocardiography. However, their natural history has not been extensively studied and remains largely unknown.
Here, we present a case of a surgically treated pulmonary artery aneurysm addressed in our center, with reference to the existing literature on the subject.
The case concerns a 56-year-old patient with previous inferolateral STEMI with coronary angiography of subocclusion of the middle right coronary artery and percutaneous transluminal coronary angioplasty (PTCA) and a drug-eluting stent (DES) on it. CT performed during this occasion showed marked dilatation of the trunk of the pulmonary artery (maximum dt approximately 55 mm) and lobar branches (right branch maximum dt approximately 33 mm; left branch maximum dt approximately 37 mm).
Since then he has reported dyspnea due to mild exertion, intermittent pain in the left hemithorax, dizzying episodes and asthenia.
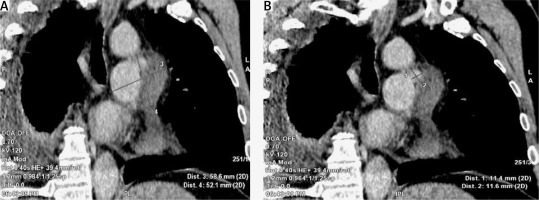
In relation to symptomatology, he underwent CT examination showing sacciform aneurysm of the common trunk and left pulmonary artery with dt LL 58 mm × AP 67 mm × CC 65 mm. At diagnostic completion, he underwent CT with contrast medium (12/6 ultrasound, US) which showed at the origin of the pulmonary trunk in the endoluminal site the presence of probable pseudoaneurysm formation (23 mm) with some hypodense linear images of not univocal characterization; minimum fluid level in the upper pericardial recess; sacciform aneurysm of the common trunk-left artery pulmonary branch (dt LL 55 mm × CC 69 mm × AP 94 mm approximately), and ectasia of the right branch (34.5 × 30 mm).
Admitted to our center, the patient underwent pre-operative diagnostic tests: coronary angiography, new CT scan of the chest with contrast medium and a transthoracic echocardiogram.
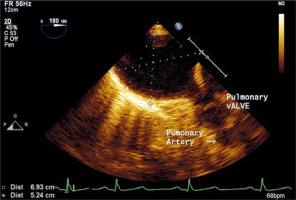
The coronary angiography showed a coronary circle free from angiographically significant lesions. The echocardiographic examination confirmed the sacciform aneurysmal dilatation of the left branch of the pulmonary artery (60 × 67 mm) and ectasia of the right branch (30 × 35 mm) in absence of pulmonary hypertension. The CT examination revealed the presence of a likely pseudo-aneurysmal formation (23 mm), common trunk sacciform aneurysm-left pulmonary artery branch (55 × 69 mm) and right branch ectasia (35 × 30 mm).
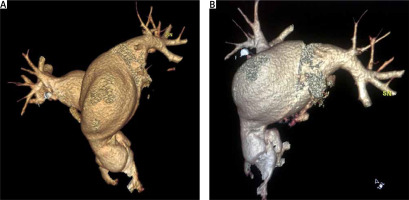
We report below the echocardiographic and CT study images performed pre-operatively (Figures 1–3).
In relation to the clinical and instrumental picture, it was decided to subject the patient to surgical excision of the pseudoaneurysm. A standard longitudinal sternotomy was performed and the patient underwent cardiopulmonary bypass.
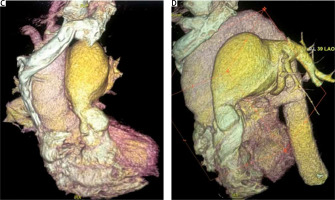
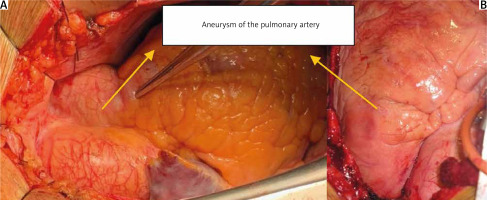
At the opening of the pericardium, the aneurysm of the pulmonary artery trunk (65 mm) extended mainly to the left branch; and ectasia of the right branch in its sub-aortic portion (Figure 4).
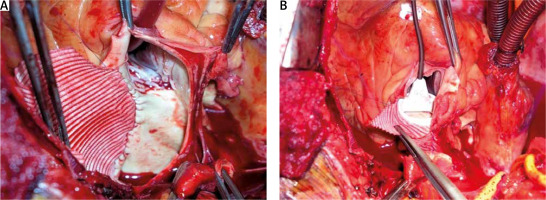
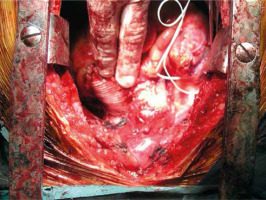
A reduction of the aneurysm of the trunk and left branch of the pulmonary artery was performed. Enlargement, with autologous pericardium patch, of the supravalvular tract of the pulmonary artery with resuspension of the pulmonary valve (Figures 5, 6).
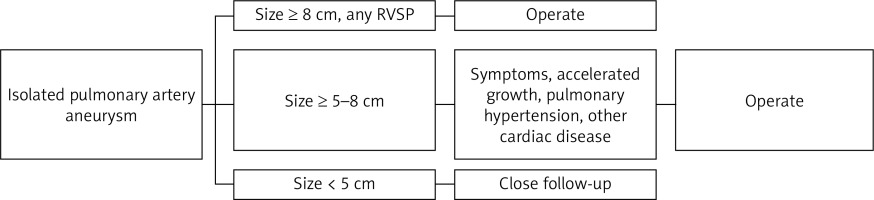
Pulmonary artery aneurysms have proven to be a very rare entity. The association with structural cardiac abnormalities, structural vascular abnormalities, pulmonary hypertension, vasculitis and infection has been noted. Surgery of symptomatic aneurysms is recommended (Figure 7).
The presence of pulmonary artery aneurysms has been linked to the presence of pulmonary hypertension and medial cystic necrosis.
Medial cystic necrosis, understood as a congenital lesion and determining pulmonary hypertension, is considered the main cause of the development of aneurysms.
Diagnosis using instrumental methods such as echocardiogram, CT or cardiac MRI is essential.
The treatment in cases of symptomatic aneurysms of size > 50 mm is surgery. If left untreated, complications such as rupture into the pleural or pericardial cavity and dissection can occur. Surgical treatment consists of replacing the aneurysmal part with a Dacron tube.
The gold standard is represented by surgery plus the elimination of the causes of pulmonary hypertension.
There are also idiopathic forms. The left pulmonary artery is involved more frequently because of its anatomy which makes it subject to greater blood flow. For aneurysms secondary to vasculitis or syphilitic disease, the main option is conservative treatment with antibiotics and glucocorticoids. In the case of small idiopathic aneurysms, medical therapy with b-blockers, diuretics and echocardiographic or CT monitoring is preferred. In the case of large aneurysms, associated with pulmonary hypertension or rapid growth and compression of adjacent structures, the treatment is surgical (aneurysms > 5.5 cm). Dilation can be focal or diffuse. In the case of focal extension, the dilated part is excised. In the case of diffuse dilatation, the entire pulmonary trunk is replaced with an allograft or synthetic graft. The results of the surgery are satisfactory, according to the literature. Surgery is inadequate for patients with severe primary pulmonary hypertension, in whom there is widespread injury to the pulmonary arterioles; in these patients the only solution is lung transplantation. Surgery is recommended in cases of aneurysm with moderate pulmonary hypertension; but in this field there is still little experience [1–9].