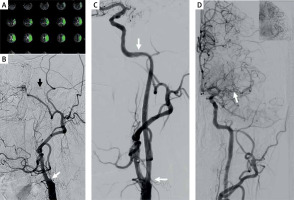
The risk of stroke in patients presenting with chronic occlusion of the internal carotid artery (COICA), despite the best medical treatment, is reported at the level of 10–20% per year [1]. Hypoperfusion of the brain either resulting from insufficient collateral circulation through the arterial cerebral circle or from occlusion of the cerebral arteries is the most common cause of such strokes. Although endovascular repair (ER) of the occluded artery remains a therapeutic option, success of such revascularization primarily depends on the location and length of the occlusion [2, 3]. ER of a long COICA is technically challenging, and the repair is associated with a risk of complications comprising distal embolization, perforation or dissection of the ICA, arteriovenous fistula to the cavernous sinus and hyperperfusion syndrome [3]. In patients presenting with a very tortuous course of the ICA in the carotid canal, navigating through the lesion and stent deployment are especially difficult. Fortunately, new guidewires, low-profile stents and balloons facilitate successful repair of symptomatic occlusions of the ICA, even in technically demanding cases. Here we present the treatment of a 73-year-old woman presenting with stroke resulting from occlusion of the left internal carotid artery. After conservative management (hypotension and double antiplatelet therapy, statin) her clinical status improved and the signs of cerebral ischemia receded. Still, during the following 3 weeks she had many recurrent 3–5-minute episodes of aphasia and hemiplegia, with several falls. Her National Institutes of Health Stroke Scale (NIHSS) score was 6–7 points. Angiography (Figure 1 B) revealed occlusion of the left ICA from its cervical (C1) to the lacerum/cavernous (C3/4) segment, and also occlusion of the horizontal (M1) segment of the middle cerebral artery, with collateral circulation to the distal segments of the middle cerebral artery coming from the anterior cerebral artery, which in turn received inflow from the posterior communicating artery. Computed tomography perfusion study (Figure 1 A) demonstrated hypoperfusion of the left cerebral hemisphere, with the mismatch volume of 112 ml. Considering the neurological status of this patient, we decided to attempt ER of the occluded ICA. After introduction of the 9F Mo.Ma proximal protection system (Medtronic, Mineapolis, MA, USA), over the V-14 ControlWire (Boston Scientific, Natick, MA, USA) guidewire, the 3MAX (Penumbra, Alameda, CF, USA) and Penumbra JET D (Penumbra, Alameda, CF, USA) reperfusion catheters were navigated into the cavernous/clinoid (C4/5) segment of the ICA. After aspiration and predilatation, two stents were implanted: the 5 × 30 mm RoadSaver stent (Terumo, Tokyo, Japan) distally, and the 7 × 40 mm Carotid Wallstent (Boston Scientific, Natick, MA, USA) proximally (the procedure was performed during dual antiplatelet therapy and heparin at a dose 50 U/kg). The final angiographic result of the procedure was good (Figure 1 C). The postprocedural course of this patient was uneventful. She was discharged home with the recommendation to use double antiplatelet therapy up to 6 months after the procedure. During the 9-month follow-up the patient did not develop new neurological symptoms. Follow-up CT and digital subtraction angiography (Figure 1 D), which were performed 6 months after endovascular revascularization, confirmed the good result of the procedure. It should be emphasized that even if the natural history of COICA is associated with a high risk of stroke, recanalization of this artery is technically very difficult and associated with potential complications. Currently reported success rates of such procedures vary from 25% to 100%. Still revascularization rates of occluded C4-C5 segments are not higher than 40%, while the procedures on the C1-C2 segments are usually successful [4]. On the other hand, the risk of serious adverse events after these procedures, including fatalities, is not higher than 3% [4]. From the technical point of view, three aspects of the procedure are pivotal: i. careful navigation through the occluded part of the artery; ii. proper placement of the guidewire in the true lumen distally from the occlusion; iii. choice of the proper stent. Therefore, endovascular recanalization of symptomatic COICA seems justifiable and safe [1, 4].
Figure 1
A – CT perfusion study – hypoperfusion of the left cerebral hemisphere with the mismatch volume of 112 ml; B – DS angiography with contrast injected to the left common artery: occlusion of the cervical segment of the internal carotid artery (white arrow) and a trace of flow in the cavernous segment (black arrow); C – final result of revascularization, implanted stents are between the arrows; D – follow-up angiography after 6 months (white arrow occlusion site of the middle cerebral arteries (MCA), in the upper right corner – distal part of MCA filled from the anterior cerebral artery)