Introduction
There is a lot of evidence showing that minimally invasive inguinal hernia repair (transabdominal preperitoneal – TAPP or totally extraperitoneal – TEP) is a more relevant surgical method than open surgery due to less postoperative pain and faster recovery [1]. However, acute postoperative pain remains one of the most common problems following laparoscopic or endoscopic hernia repair. Avoiding predictive factors of acute pain after surgery or prescribing additional analgesia for patients with risk factors that cannot be removed are some of the options that can be used to reduce acute postoperative pain. The HerniaSurge Group recommends a laparo-endoscopic procedure for male patients with primary unilateral hernia due to both lower postoperative pain incidence as well as reduction of chronic pain incidence [1]. It means that one of the acute pain risk factors can be eliminated by choosing a minimally invasive technique for inguinal hernia repair. Also, some studies indicate significant affecting factors for acute pain such as the patient’s younger age, previous chronic pain, presurgical anxiety, and the rumination component of pain catastrophizing [2]. However, there is a lack of clinical studies that evaluate predictive factors for postoperative pain after TAPP and TEP surgeries.
Aim
The aim of the study is to identify independent risk factors predicting pain after laparoscopic and endoscopic inguinal hernia repair.
Material and methods
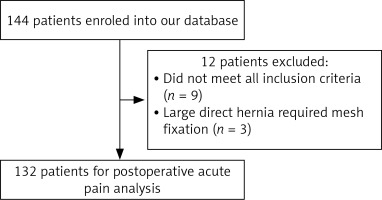
The study protocol was evaluated and approved by the Ethics Committee of the Lithuanian University of Health Sciences (protocol Nr. BEC-MF-415). A prospective, randomized clinical trial included 144 male patients aged 18–80 years, undergoing elective minimal invasive primary inguinal hernia repair. All patients gave their written informed consent. Exclusion criteria were age older than 80 years, ASA class IV and above, strangulated hernia, and patients with neurological or psychiatric disorders. Twelve patients were excluded because they did not meet all inclusion criteria or a large direct hernia required mesh fixation. Finally, 132 patients were included, and their data were analysed (Figure 1).
The study was carried out by single-blind randomisation of patients into 2 groups (transabdominal preperitoneal approach (TAPP) and total extraperitoneal approach (TEP)) depending on the type of minimal invasive inguinal hernia repair surgery. An envelope with an operation method was blindly chosen immediately before the surgery for all patients that were hospitalised for selective minimally invasive inguinal hernia repair.
Basic characteristics (age, body mass index, leading diseases, previous surgeries), symptoms related to hernia (tension in groin area, bulging), and duration of symptoms were recorded, along with potential factors that could affect the formation of hernia (smoking, occupation, prostate diseases).
All surgeries were performed by experienced surgeons following the same protocols. Operations were done under general anaesthesia, and the same painkillers were used in each surgery. The 3D MAX Light mesh was used for TAPP hernia repair, and a 10 × 15 cm Parietene mesh was used for the TEP technique. No mesh fixation was used in either type of hernia repair. Intra-operative findings (hernia type, size, nerve identification, duration of the surgery, intraoperative complications) were recorded after surgery. Postoperative pain was evaluated 3 h after surgery using a visual analogue scale (VAS) when the patient was moving. Nonsteroidal anti-inflammatory drugs (Ibuprofen) were prescribed only when the pain was greater than 3 points according to VAS 3 h after surgery. Groups of patients that felt mild pain (VAS 0–2) and patients that felt average or severe pain (VAS 3–10) were then compared.
Statistical analysis
Data were collected and processed, and statistical analysis was performed using IBM SPSS Statistics 26.0 program. The assumption of normality of a continuous variable was verified using the Kolmogorov-Smirnov test. If the distribution of the variable met the assumption of normality of the distribution, Student’s (t) criterion or Pearson correlation was applied to compare the quantitative values of the 2 independent groups, and one-way analysis of variance ANOVA was used to compare more than 2 groups. Data are presented as means ± standard deviation. Statistically significant differences were assessed when p < 0.05. The chi-square (χ2) criterion was used to compare the nominal data. Nonparametric statistical calculation methods were also used – the Kruskal-Wallis nonparametric test of independent samples was performed. The study used multivariate logistic regression analysis using the backward stepwise method to calculate the odds ratio (OR).
Results
A total of 132 male patients were included in the study: 68 patients in the TAPP group and 64 in the TEP group. The average age of all patients was 56.1 ±13.9 years, and there was no significant difference in average age between the 2 groups. Other general characteristics, such as body mass index (BMI), were similar in both groups. The main symptoms before surgery were tension in the groin area, bulging, or both, a few patients had incarcerated hernia and/or urination disorders, and 1 patient had a hernia that was previously strangulated. Symptoms lasted less than 1 year for more than half of the patients. There was no significant difference in duration of surgery in the TAPP and TEP groups. The most common hernia type, according to EHS classification, was lateral hernia with a defect of less than 1.5 cm, there were no cases of large direct hernia with defect diameter larger than 3 cm. No significant intraoperative or early postoperative complications were recorded. The majority of patients were released the day after surgery (Table I).
Table I
General characteristics, pre-operative and peri-operative data
The impact of intraoperative and postoperative factors on acute postoperative pain
In the data analysis we compared early postoperative pain 3 h after surgery, dividing the patients into 2 groups according to their pain intensity: the 1st group experienced no or mild pain (0–2 VAS scores), and the 2nd group experienced moderate or strong pain (3–10 VAS score). The age difference between patients that felt mild/moderate and those who felt strong/acute postoperative pain was not significant. Analysis shows that patients with duration of symptoms of more than 1 year felt significantly stronger pain 3 h after surgery and required analgesia. Smokers reported moderate or strong acute pain more commonly than non-smokers. Patients who worked in physical jobs felt significantly less intense acute postoperative pain when moving 3 h after surgery. However, combined physical and mental or only mental occupation did not significantly increase postoperative pain (Table II). Also, patients who underwent TAPP surgery complained about stronger pain significantly more often (Table III).
Table II
The influence of risk factors on acute postoperative pain
Table III
Average pain after different types of surgery
| Average pain score (VAS) 3 h after surgery | P-value | |
|---|---|---|
| TAPP (n = 68) | TEP (n = 64) | |
| 4.2 ±1.9 | 2.8 ±0.7 | 0.017 |
Multivariate analysis
The influence of all the criteria on the strength of acute postoperative pain 3 h after surgery was evaluated using the backward stepwise method of multivariate logistic regression. The results suggested that disease duration of more than 1 year, smoking, as well as TAPP surgery significantly increased the risk of moderate and strong pain 3 h after surgery. Conversely, disease duration of less than 1 year as well as physical occupation decreased the risk of pain by more than 3 points according to the VAS (Table IV).
Discussion
Minimally invasive hernia repair methods are preferable to the open approach due to less acute postoperative pain and faster recovery [1]. However, pain remains one of the most common complaints following hernia repair [3]. Prevention of acute postoperative pain risk factors and the administration of adequate analgesia at the right time are both important because there is evidence that patients who feel average or severe pain immediately after surgery are faced with a 6-fold higher risk of chronic pain development [4]. Our study analysed pain scores according to VAS 3 h after surgery. Although postoperative pain was also evaluated 6 and 9 h after surgery, these results were not analysed because of the administration of painkillers that were prescribed for patients who recorded pain score of more than 3 – this could have distorted the postoperative pain results.
Knowledge of risk factors for acute postoperative pain may prevent or help reduce pain after surgery as much as possible [5]. However, we found only a few studies that showed predictive factors for acute pain after both types of procedures: open or minimally invasive. Chronic pain seems to receive more attention. Unsurprisingly, even HerniaSurge Group guidelines state that laparoscopic or endoscopic surgery is the method of choice, because it causes less postoperative pain. Based on this, we decided to find out the risk factors that can predict stronger postoperative pain after minimally invasive surgeries (TAPP or TEPP).
In a large prospective study that was announced in 2007, risk factors for acute pain after open hernia repair were listed as young age, BMI > 25 kg/m2, day surgery, and the use of Radomesh, which is no longer used [6]. Comparing to minimally invasive methods (laparoscopic, robotic), open inguinal hernia repair is more often associated with acute postoperative pain and is one of its predictive factors [7]. Clinical factors associated with a significantly higher pain score after TEP include mesh fixation by stapling, female sex, and age ≤ 65 years [8]. The latest similar study of 807 patients of laparoscopic and endoscopic surgery indicated that pain before operation, younger age, and staple mesh fixation were all associated with stronger acute postoperative pain, especially on the first day after surgery [9]. In our study we could not evaluate acute pain prediction by sex, because all of our included patients were male. We made this choice based on inguinal hernia presenting much more commonly in males (about 90% of patients undergoing hernia repair are typically male) and due to the potential risk of female inclusion in making the study groups too inhomogeneous [10]. Published metanalysis showed that mesh fixation significantly increased the rate and intensity of pain and was recommended only in large direct hernias during TAPP or TEP surgeries [1, 11]. Taking this into account, no mesh fixation was used in our study. Also, to eliminate as many of the factors as possible that could have made our study groups inhomogeneous, we used only 2 types of lightweight meshes for all of the surgeries. As a result, we could not evaluate mesh fixation and mesh type as predictive factors for acute pain, despite them presenting as significant risk factors in other clinical studies.
As mentioned earlier, in most studies younger age appears to be one of the predictive factors for acute postoperative pain [6, 8, 9]. Younger age acts as a predictor not only for pain after hernia repair, but also for acute pain following other types of surgery [12]. The same tendency was apparent in our study; patients who felt average or severe pain after surgery were typically younger, but no significant difference was found.
Another predictive factor for stronger postoperative pain is the duration of groin hernia appearance prior to surgery. This may be due to the more difficult tissue and hernia sac dissection that is typical in such cases. This risk factor is poorly discussed in other studies, and an option to minimize postoperative pain could be surgery performed as soon as possible after the diagnosis [13].
Smoking has been suggested as a causative factor for hernia formation [14]. Our study shows that smoking is also one of the risk factors for more severe pain after minimally invasive hernia repair. There are no data suggesting that quitting smoking prior to hernia repair could help reduce pain after surgery, but smoking patients can be included in the risk group, and additional tools such as transversus abdominis plane block and rectus sheath block or TENS procedures can be used to minimize acute pain after surgery [15–18].
Physical effort, especially physical occupation, can also be one of the factors for inguinal hernia formation [12]. However, our study shows that physical occupation is significantly associated with less pain after minimally invasive hernia repair. This factor is not discussed in similar studies and may be suggested as one of the advantages for patients who undergo minimally invasive hernia repair. However, there was no significant difference found in pain intensity between patients with mental or combined mental/physical occupation.
One of the most debatable questions on minimally invasive hernia repair is which surgical technique should be chosen. There are many studies that compare TAPP and TEP techniques and show some advantages for each type of surgery, but there is no final consensus as to which method is more favourable. Similar operative times, overall complication risks, postoperative acute and chronic pain incidence, and recurrence rates make the choice of the surgery type a decision based on the surgeon’s expertise [1]. In our study, patients who underwent TAPP hernia repair complained about average or severe pain significantly more often and needed additional analgesia 3 h after surgery, making the TAPP technique one of the predictive factors of acute postoperative pain. We therefore suggest that the TEP technique may be discussed as the first choice of surgery, especially for patients presenting with other predictive postoperative acute pain factors.
This study is ongoing, to collect larger groups for stronger results and to evaluate predictive factors for chronic pain. The exclusion of some factors such as sex, mesh fixation, meshes of different types and weight, which have been shown by previous studies as predicting factors for acute pain after minimally invasive hernia repair, may be considered a limitation of this study. However, we excluded these factors to make the study groups as homogeneous as possible. Moreover, for repair we used 2 meshes that are similar in materials and weight but are from different producers and have different features. We should stress that the use of different types of mesh for the 2 approaches might influence the results. Finally, data on pain intensity should be collected at 7 and 30 days postoperatively, to evaluate not only immediate pain after surgery, but also acute pain when painkillers should no longer be used.
Conclusions
This study shows that duration of groin hernia appearance, smoking, physical occupation, and TAPP technique are all possible predictive factors for acute postoperative pain after minimally invasive inguinal hernia repair. Hence, we suggest that some factors, such as type of surgery, can be avoided, especially for patients that have more than one predictor of acute pain. Lastly, for patients with risk factors that cannot be avoided, additional medicaments or physical analgesia tools can be used in the early postoperative period to prevent severe acute pain.