Introduction
Stage IV disease has been traditionally managed on a palliative basis with limited hopes for curative treatment. However, surgical resection is increasingly offered for selected patient cohorts with a limited metastatic disease burden with curative intent to render them disease-free [1, 2]. Pulmonary metastasectomy (PM) has been established as a therapeutic option for pulmonary metastases of extra-thoracic solid organ malignancies – which can develop in approximately 30% of patients with known primary solid cancer – in order to improve survival [3–5]. However, this claim has been challenged by a lack of solid evidence-based results from randomized controlled trials (RCTs) [6]. Perquisites for potential survival advantages from PM include isolated limited pulmonary metastases which are amenable to complete resection without major lung function compromise after proper control of the primary tumor [1]. Despite wide practice of PM over decades – almost 10% of the daily activity of thoracic surgery clinics – the standard approach for PM is still debated [7, 8].
The choice of surgical approach is determined by many factors, including:
Lesion(s) characteristics: location, size, number, involvement of one or both lungs and associated mediastinal lymphadenopathy.
High-quality imaging availability.
Underlying functional reserves of the patient and performance status.
There is a shifting trend toward minimally invasive surgery, which is even rapidly evolving. Video-assisted thoracoscopic surgery (VATS) has been incorporated in various diagnostic and therapeutic aspects in the field of thoracic surgery. Shifting from conventional multi-port surgery to single-port surgery (uniportal VATS) with its modifications including subxiphoid VATS and increased application of robotic-assisted thoracic surgery (RATS) is steadily progressing in different benign and malignant disease entities.
It is worth mentioning that the topic of pulmonary metastasectomy is still debated in all its different aspects from the very basic question about the true survival benefit of surgical resection, the ideal surgical approach, either open or thoracoscopic, treatment strategy in bilateral disease, and finally which minimally invasive approach offers the best outcomes to patients. Considering the sparse conclusive data from RCTs, we are carrying out this review of the literature aiming to seek the best available evidence or consensus for practice, focusing on applications of subxiphoid uniportal VATS in pulmonary metastasectomy.
Level of evidence for survival advantage in pulmonary metastasectomy
Despite wide practice of PM, there is a paucity of well-powered studies demonstrating its beneficial role in multimodality therapy of cancer patients with lung metastasis. Data are derived from retrospective and small prospective studies and registry data with absence of RCTs or satisfactory comparative analysis to provide a convincing evidence base for such wide practice (accounts for 10–20% of workload in thoracic units) [6]. This limits extrapolation of these data to all patients with pulmonary metastasis. Meticulous weighing of the potential survival benefits against the potential hazards of surgery, particularly delay of systemic therapy until recovery, is of utmost importance. The ethical question of exposing such a vulnerable cohort of patients to surgical risk without solid evidence of survival advantage remains a valid question until today.
The popularity of practicing PM was probably derived from data of an important landmark publication from the International Registry of Lung Metastasectomy (IRLM) in 1997 which reported 5206 lung metastasis patients of different disease primaries who underwent PM [4, 9]. It showed that irrespective of the primary type, complete surgical resection of all detectable metastases was associated with significant survival advantage (36% in patients with complete resection compared to 13% in patients with incomplete resection). Further advantages were observed in patients with fewer metastases and longer disease-free interval [4]. This concept has been validated and confirmed in multiple retrospective reports. However, this landmark publication, as well as these reports, has been criticized owing to the inherent flaw of selection bias. Patients in these studies are surgical candidates with favorable prognostic criteria such as limited number of metastases, long disease-free interval and good performance status. Patients with these advantageous prognostic factors are likely to survive longer irrespective of treatment offered to them. In the absence of well-matched control cases, in well-powered RCTs, it is hard to conclude that the observed survival benefit is truly due to surgical intervention and not due to favorable tumor biology in these highly selected patients. In other words, did longer survival provide opportunity for more PM operations or were PM operations the cause of longer survival?
Increased uncertainty about the value of PM was further supported by the data which can be indirectly driven from RCTs comparing intensive vs. less intensive surveillance practice after resection of primary colorectal cancer. Two large meta-analyses of RCTs showed that surveillance successfully increased the rate of detection of metastases up to 2 years earlier, which led to more surgical interventions, but there was no overall survival benefit [10, 11].
To overcome this dilemma, a call for a well-designed RCT addressing this question was made. A study protocol was made by PulMiCC trial authors to compare PM vs. no surgery in patients with lung metastasis from colorectal cancer. Based on the assumption that a 10% difference in overall mortality at 3 years is the minimally important clinical difference and the inferiority margin for the design of the PulMiCC non-inferiority trial, the authors declared that a sample size of 300 would provide 78% power to detect an increased relative risk of mortality in the non- interventional arm to 1.3. The study was stopped due to low recruitment (65 patients). The small number of trial participants prevents a conclusive answer to the research question. The estimated survival in this study was 38% (23–62%) for patients with metastasectomy and 29% (16–52%) in well-matched controls [12]. A full report in 2020 gave survival data in all 93 randomized patients (46 PM and 47 controls). The authors concluded that there is no survival benefit for PM over non-surgical approaches because the survival of well-matched control patients is better than that previously reported in non-comparative studies. The solid belief in the advantage of PM should be revised. Large, definitive RCTs, investigating the possible benefits of the practice of PM for any tumor type, are clearly needed [13].
Role of VATS in pulmonary metastasectomy
Both VATS and open thoracotomy (OT) are widely accepted as appropriate approaches for carrying out PM [14]. On one hand, OT has demonstrated enhanced detection and hence, resection of more metastases than VATS techniques, especially for nodules deeply seated within lung parenchyma [14–16]. On the other hand, VATS has been considered a preferable approach due to superior functional outcomes, offering less pain, decreased analgesic demands, enhanced recovery, shorter hospital stay, shorter duration of chest tube drainage, decreased blood loss and transfusion requirements, decreased post-operative morbidity, less impact on pulmonary functional reserve and early recommence of systemic therapy [17].
In addition to these advantages, resection of pulmonary nodules through a minimally invasive technique induces minimal trauma to the tissues and subsequent immune response. The decreased immune response may be transferred into a delay in disease progression [18]. Moreover, at least 40% of patients with pulmonary metastases from sarcoma may experience ipsilateral or contralateral pulmonary disease relapse after surgery [19]; several studies have indicated that repeated resection is beneficial for patients with recurrent pulmonary metastases [20, 21]. Repeated thoracoscopic resections are better tolerated than OT resections regarding the pulmonary functional reserve [18]. In addition, thoracotomy is reported to carry a high rate (some studies report up to 76%) of unnecessary resections of benign nodules with the surrounding lung parenchyma [7].
The ideal access for VATS in pulmonary metastasectomy is a matter of discussion. Various techniques ranging from multiport VATS with or without utility incision, uniportal VATS, subxiphoid VATS, a hybrid approach combining VATS and an open approach to robotic-assisted technique have been reported in the literature [22, 23]. The principle of VATS is to avoid rib spreading and to perform complete resection with correct identification of the lesions.
Although no randomized controlled trials have been completed in this field, several comparative reports have examined this topic. The primary limitation for VATS PM is missing nodules as it depends on pre-operative imaging alone. The missing rate was reported in early series up to 56% of patients after attempted VATS resection [24]. However, this rate significantly dropped after improvements in CT scanning slice thickness and the expanded role of integrated PET-CT in oncology. Eckardt et al. in their prospective work sequentially operated on 89 cases with pulmonary metastasis by VATS then OT approaches [25]. The VATS team members were asked to revise imaging studies of patients then try to localize all image-detected nodules as well as any other nodules that could be found by VATS surgery. VATS surgeons were asked to record their findings but not to resect any lesions. Afterwards, the OT team implemented the surgery to resect all identifiable nodules. Their report showed that out of 140 nodules that were identified on preoperative CT, the VATS team was successful in identifying 122 (87%) nodules, while OT was able to identify all radiographically detectable nodules along with 67 additional nodules. Two-thirds of these nodules (64%) were found to be benign lesions while one-third (33%) of nodules were true metastases. The authors concluded that VATS is inadequate for the management of pulmonary metastatic disease. In a related work, Macherey et al. reported greater detection of nodules in OT compared to pre-operative imaging, though 48.5% of these lesions were found to be benign [26]. Despite the enhanced detection of additional lung nodules, resulting survival rates were reported to be comparable in thoracotomy and VATS patients [27–29]. It should be cautiously interpreted that the data are primarily derived from retrospective studies with selection bias for thoracoscopic candidates.
Lack of tactile feedback makes localization of deep nodules challenging. When lesions are difficult to localize with visual inspection or finger palpation, a number of alternative localization techniques are available, to minimize the need for conversion to thoracotomy.
These localization techniques can be categorized into four groups according to the materials used:
localization with metallic materials: hook-wire [30–32], microcoil or spiral coil [33, 34],
localization with dye: methylene blue [35, 36], India ink [37] or indigo carmine [38],
localization with contrast agents: lipiodol [38], barium [39],
radioguided occult lesion localization (ROLL) with radiotracers [40].
Other systems used are: image-guided VATS (iVATS) [41] and virtual-assisted lung mapping (VAL-MAP), which has evolved from bronchoscopic dye localization [42]. In spite of their aid to optimize thoracoscopic resection, their use is surgeon/center-dependent. There is no consensus as regards the optimal method of preoperative localization [43].
The rate of pulmonary recurrence, especially ipsilaterally, which can reflect the possibility of missing small lung nodules using VATS, is still a debated issue. Data from previous studies showed that ipsilateral pulmonary recurrence for OT was in the range 14–15% compared to 12–20% for VATS. Moreover, total pulmonary recurrence for OT was 25.7–40%, as compared to 22.9-36% for VATS [44, 45]. In more than 80% of cases, recurrence is located in the non-operated, contralateral lung or at a distant extra-thoracic site [46, 47].
In a meta-analysis of observational studies, Meng et al. reported eight studies which included 337 patients in the VATS group, and 485 in the OT group. Although not statistically significant, survival was in favor of the VATS group, and no difference was found in recurrence-free survival [48]. In another related article, Murakawa et al. reported data of 1,047 patients [49] comparing survival between VATS and OT groups. VATS metastasectomy showed a better overall survival than the open approach [49].
In a recent survey including 22 centers with expertise in VATS surgery, 88% of surgeons considered that VATS should be considered for isolated pulmonary metastasis [50]. The Society of Thoracic Surgeons proposed an expert consensus stating that a minimally invasive PM could be an effective alternative to traditional OT for selected patients due to the better postoperative recovery and enhanced quality of life outcomes [51]. However, these authors added that if a complete resection and pulmonary parenchymal sparing could not be achieved by a minimally invasive technique, open techniques should be preferred. Even without strong evidence in the literature, these recommendations reflect a change in paradigm in favor of less invasive approaches, at least for solitary lesions.
To conclude, the level of evidence supporting superiority of one approach over the other is still limited. Therefore, PM should be a trade-off between benefits to improve survival and risks of compromise to pulmonary functional reserve. A definitive approach should be tailored according to patient/disease characteristics including number, size and location of nodules, associated mediastinal nodes and underlying pulmonary functions.
Dilemma in bilateral lung oligometastases
Although the approach to bilateral lung metastasis is more debated, the basic principles remain the same; complete surgical resection is the ultimate surgical goal. Oligometastatic disease is defined as up to five nodules or nodules amenable to a therapeutic approach with curative intent [52, 53]. Median sternotomy, “clamshell” thoracotomy (i.e., a bilateral anterior thoracotomy with a transverse sternotomy), sequential bilateral thoracotomies, and simultaneous bilateral posterolateral thoracotomies have all been reported as accepted surgical approaches to the resection of bilateral pulmonary metastases [54]. No consensus has been reached on the optimal approach. In a relevant survey among members of the European Society of Thoracic Surgeons (ESTS), Internullo et al. asked members “Which is your preferred approach for clinical bilateral disease?” Among responders, two thirds perform bilateral staged thoracotomies. Median sternotomy (one-fourth) and bilateral sequential thoracotomies (one-fifth) came next. Bilateral VATS (staged or one stage) and clamshell thoracotomy were performed less frequently [55].
Van der Veen et al. advised median sternotomy as the procedure of choice for lung metastasis. Advantages are the possibility for bilateral simultaneous staging, detection of occult metastases, complete surgical clearance in one setting and decreased pain and morbidity [56]. However, advances in imaging made anticipatory exploration of both lung fields a less favorable option unless definitely indicated. In their experience of 131 patients, Regal et al. reported that median sternotomy reduced morbidity and allowed earlier resumption of systemic therapy [57]. Nonetheless, access to posterior aspects of both lungs and the lateral part of the left lower lobe may be challenging. Better angulation for stapling devices can be gained by use of lateral small incisions which are used for chest drains after surgery [58].
Bilateral thoracotomies offer excellent access to both lung fields but at the cost of postoperative pain. Some authors emphasize better access to the lymph node stations for proper staging with thoracotomies [59]. If a staged resection is assumed, then the side with the greater number of metastases is operated on first. In terms of time frame, a minimum of a 2- to 3-week interval is accepted but waiting 4 to 6 weeks is preferred. Although bimanual palpation of both lungs may reveal occult disease otherwise missed by preoperative imaging, no survival advantage was reported compared to the unilateral approach if disease is evident on one hemithorax on diagnostic imaging [60]. If further exposure is required, a transverse transection of the sternum is carried out, thereby converting to a clamshell incision [60].
Due to its minimally invasive nature, thoracoscopic resection is better tolerated and associated with superior recovery of pulmonary functions compared to open procedures. Carrying out VATS for bilateral pulmonary metastasis can, similarly, be a simultaneous or staged procedure. There are no conclusive data about superiority of one approach over the other. Classic 3-port VATS is widely performed in thoracic units for thoracoscopic management of lung metastasis. However, over the past decade, uniportal VATS (uVATS) has become a new area for enhanced development in minimally invasive thoracic surgery [61]. uVATS is viewed as a less invasive approach which allows major thoracic procedures to be performed using a single small incision through which the thoracoscope and all instruments can be applied. Reported advantages of uVATS include reduced surgical trauma, decreased degree of pain, faster recovery, providing superior cosmetic outcomes and improved patient satisfaction [62]. However, the lack of long-term data of outcomes of uVATS, concerns about operative safety and technical challenges (limited manipulation of surgical instruments and loss of triangulation) represent some limitations to practice of uVATS. In their meta-analysis which included 8 articles, Harris et al. reported statistically significant reduction of the overall rate of complications, length of hospital stay and duration of postoperative drainage for patients who underwent uniportal VATS lobectomy. There were no significant differences between the two treatment groups regarding mortality, operative time, perioperative blood loss and rate of conversion to open thoracotomy [63]. It can be assuredly anticipated that with consistent reports of excellent short results, uVATS – through a small, 4 cm or less, incision – will become more and more widely accepted [64, 65].
Subxiphoid uniportal VATS surgery
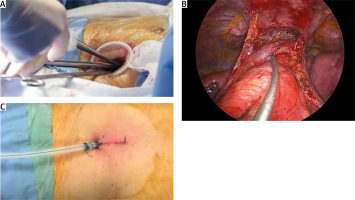
Although postoperative pain and paresthesia can be reduced with uVATS due to its minimally invasive nature, they often still occur when an incision through the intercostal space is utilized. Advances in technology and innovative surgical devices have led to the development of a novel uVATS involving a subxiphoid approach which includes a 3–4 cm skin incision at the subxiphoid area, through which a thoracoscope and specialized instruments can be applied to provide access to one or both lung fields simultaneously (Figure 1) [66]. Advantages of subxiphoid uVATS include those reported for uVATS in general (reduced surgical trauma, enhanced recovery, and improved patient satisfaction) in addition to decreased degree of pain owing to avoidance of intercostal incision and superior cosmetic outcomes with no visible chest scar [66].
Figure 1
Operative views of subxiphoid uniportal VATS: A – Instruments’ application through the same incision using a wound protector; B – operative view showing both lung fields accessed simultaneously in subxiphoid uVATS thymectomy; C – post-operative view showing intercostal tube applied from the incision
Hybrid transthoracic VATS and the transxiphoid hand-assisted approach using a subxiphoid incision was first reported by Mineo et al., in 1999, for management of pulmonary metastasis [67]. Suda et al. reported in 2012 the use of a subxiphoid 3.5-cm incision for thymectomy in an 81-year-old woman with myasthenia gravis complicated with a thymic cyst [68]. Two years later, the author et al. reported a 3-cm single-incision subxiphoid approach for bilateral pulmonary metastasectomy [69]. In 2015, Wu et al. reported their first six consecutive thoracoscopic extended thymectomies performed through a single subxiphoid incision with no conversion to sternotomy. They concluded that the procedure is safe and feasible, with good cosmesis and promising short-term results [70].
Initially, this procedure was applied to metastasectomies, bullae disease for pneumothorax operations and anterior mediastinal tumor resections. Since then, the use of subxiphoid uVATS approaches has steadily progressed to include lobectomies. Liu et al. reported a subxiphoid uniportal VATS left upper lobectomy in 2014 [71]. In their single-center experience over one year duration, Yang et al. compared 37 patients who consecutively underwent subxiphoid uVATS lobectomies to 68 patients who underwent traditional three-port VATS. They concluded that subxiphoid uVATS lobectomy is a safe and feasible surgical procedure, associated with reduced surgical trauma and postoperative visual analog scale (VAS) pain scores as well as improved cosmetic results compared with traditional VATS. On the other hand, operative time was longer in the subxiphoid uVATS group than in the traditional three-port VATS group. The authors reported no perioperative mortalities, and no significant differences were found in the number of retrieved lymph nodes, number of explored nodal stations, blood loss, drainage time, postoperative complications, or length of hospital stay between the two groups [72].
In another study, Song et al. in 2016 reported 96 cases of patients who underwent unilateral operation and 9 who underwent bilateral lung operations. Among the 9 cases undergoing synchronized bilateral resections, each case received unilateral lobectomy with contralateral pulmonary wedge resection. Right upper lobectomies represented 44.8% of all cases. All procedures were successfully performed with a complication rate of 10.5%. The average pain scores were significantly lower than those in the control group (standard intercostal uniportal VATS) (p < 0.001). The authors concluded that subxiphoid uVATS lobectomy is safe and reliable, which is appropriate for bilateral lung diseases, and significantly relieves postoperative incision pain [73].
Subxiphoid lung segmentectomies were reported by Aresu et al., who described 79 consecutive patients, who underwent 84 subxiphoid segmentectomies for malignant or benign pulmonary diseases (45 segmentectomies on the right side and 39 segmentectomies on the left side). Five (6.3%) cases experienced conversion (4 to thoracotomy and 1 to conventional VATS) [74]. The same authors reported their experience in subxiphoid VATS bilateral segmentectomy for synchronous bilateral lung adenocarcinomas in a 60-year-old female patient who received right upper lobe upper segmentectomy and left upper lobe apical trisegmentectomy [75].
Hernandez-Arenas et al. reported subxiphoid uVATS surgery for major lung resections. Of the 153 patients operated on, 105 had lobectomies and 48 had segmentectomies. Among these, 5 cases were converted to conventional VATS due to technical difficulties, and 8 cases were converted to thoracotomy due to major bleeding [76]. Ibrahim et al. reported a modified subxiphoid incision with addition of a small 5–10 mm separate incision at the 6–7 midaxillary line for the camera. Their study included 50 cases of different types of benign and malignant disease including anatomical resections (16 lobectomies and 9 segmentectomies) [77].
Subxiphoid uniportal VATS for pulmonary metastasectomy
Potential advantages for subxiphoid uVATS in PM are providing access to both lung fields simultaneously, avoidance of staged procedures (with inherent surgical risks attributed to any surgical procedure/anesthesia), decreasing postoperative pain scores and enhanced rehabilitation [66]. Nevertheless, the approach is limited to case reports/series. Bilateral pulmonary metastasectomy performed by a combination of transthoracic VATS and tumor palpation through a subxiphoid incision was first reported in 1999. This approach used an 8 cm incision with transxiphoid manual palpation of both lung fields in 6 cases with pulmonary metastasis [67]. The feasibility and long-term results of this approach were further validated in 2007 [78].
In 2014, Suda et al. reported a case of a single 3-cm incision for bilateral wedge resection metastasectomy using the subxiphoid uVATS [69]. One year later, Liu et al. reported their first two pulmonary metastasectomy cases by subxiphoid uVATS [79]. A 43-year-old female patient was admitted for resection of bilateral lung metastases for previous nasopharyngeal carcinoma. PET-CT showed five lung nodules suggestive of metastatic deposits, two nodules in the right lower lung, two in the left upper lung, and one in the left lower lung, with tumor sizes ranging from 0.7 to 1.3 cm. One of the five lesions was deep seated and required preoperative localization with the aid of methylene blue. Using a 3.5-cm subxiphoid vertical incision, with the patient placed in the supine position, all lesions were successfully resected with resection margins of the removed lesions being free from cancer. The other case was a 38-year-old female patient with breast cancer who underwent salvage right middle lobectomy for pulmonary metastasis. Kermenli T and Azar C reported a case of subxiphoid uniportal video-assisted thoracoscopic surgery for synchronous bilateral pulmonary metastasis in a 39-year-old female patient with osteosarcoma who had right lung lower lobe basal segment and left lung upper lobe posterior segment nodules and received bilateral wedge resections [80].
Proper patient selection is essential for optimal outcomes. Resectable metastatic pulmonary nodules located in the peripheral lung are excellent candidates. Deep tumors, which are not directly beneath the pleura, are difficult to localize and to confirm adequate length of surgical margins. This makes them unsuitable for subxiphoid uVATS unless preoperative marking is properly done [66].
Subxiphoid uVATS has certain challenges and limitations:
Subxiphoid uVATS is not suitable for complex thoracic procedures, such as sleeve lobectomies, vascular reconstructions, redo surgery and surgery in a previously irradiated chest.
Control of any bleeding is difficult to achieve.
Passage of instruments to the left hemithorax may induce cardia arrhythmia and hypotension during surgery.
Access to the posterior lung anatomy is difficult. However, it can be overcome by good lung retraction and optimizing the position of the scope.
Working on the left pleural cavity can be very challenging, especially in the case of cardiomegaly.
There remain several segments that are not amenable to resection via subxiphoid VATS, particularly S2 and S6 segmentectomies on the left and S9 and S10 bilaterally.
Proper lymph node dissection, especially station 7, is challenging. Earlier reports of subxiphoid VATS were limited to LN sampling but with increased experience the number of lymph nodes dissected gradually increased. Systematic lymph node dissection with removal of lymph nodes from at least 3 N2 stations (as per the International Association for the Study of Lung Cancer “IASLC” classification) can be done.
This approach opens the pleura bilaterally and connects the left and right thoracic cavities with each other. After surgery, if air leakage, pneumothorax or malignant pleural effusion occurs on one side, bilateral pneumothorax or effusion may result.
Conclusions
Pulmonary metastasectomy is viewed by many thoracic surgeons as a potential chance for cure that should be offered to pulmonary metastasis patients, based on data from observational studies and registry databases. However, there is a marked paucity in the literature of solid evidence from well-powered, proper-sized RCTs. The advances in the thoracic surgical field and prioritization of quality-of-life outcomes make thoracoscopic resection a more favorable approach to PM owing to enhanced recovery. There are limitations that face VATS resection and must be well addressed to achieve a broad consensus about its universal applications in PM, particularly the possibility of missing or incomplete resection of deep-seated lung nodules. uVATS, either transthoracic or subxiphoid, is increasingly applied in pulmonary resections due to the accumulating evidence of functional and cosmetic advantages over traditional VATS. Use of subxiphoid uVATS in PM is still limited to case reports of a small number of patients. There is room for improvements in subxiphoid uVATS due to reported technical challenges and limitations. Larger sample prospective studies are needed to further evaluate this emerging technique in different types of pulmonary resections, particularly PM.






