A 57-year-old man, ex-smoker, with a background of hypertension, type 2 diabetes, previous myocardial infarctions and multiple previous percutaneous coronary interventions presented acutely with a posterolateral ST-elevation myocardial infarction. There were no available medical reports describing his previous procedures as the patient was a visitor from abroad.
Emergency coronary angiography revealed severe in-stent restenosis in the right coronary artery along with a severe de-novo lesion at the crux. The left anterior descending artery had a widely patent stent but severe disease distally. A large obtuse marginal of the left circumflex artery was occluded due to late stent thrombosis in the proximal segment, which was considered the culprit lesion (Figure 1 A – white arrow). The patient received loading doses of aspirin and ticagrelor.
Figure 1
A – Coronary angiogram, occluded left circumflex due to late stent thrombosis. B – Optical coherence tomography (OCT) demonstrating stent underexpansion and circumferential (360°) calcification behind the stent struts, extending around 0.5 mm in depth. C, D – “Dog-bone” appearance and residual waisting after aggressive NC balloon inflations. E – Repeat OCT run demonstrating an improved minimum stent area
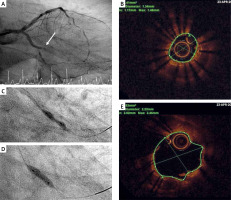
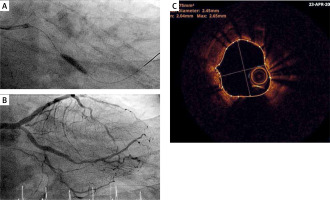
The lesion was crossed with a standard workhorse wire and after restoring flow using a 2 mm semi-compliant balloon, it was assessed by optical coherence tomography (OCT). A focal area of severe stent underexpansion with a minimum stent area (MSA) of 1.41 mm2 was revealed (Figure 1 B). There was also severe circumferential (360°) calcification behind the stent struts, extending around 0.5 mm in depth, but not any neoatherosclerosis in front of the struts. Dilatation of the underexpanded stent was undertaken, with a 3 mm non-compliant (NC) balloon inflated at 16 atm. However, the balloon appeared to have a “dog-bone” appearance (Figure 1 C). We then inflated more aggressively up to 26 atm, but the balloon inflation still had a degree of waisting (Figure 1 D). A repeat OCT run demonstrated an improved MSA of 3.9 mm2 in the culprit lesion (Figure 1 E). We did not have access to intravascular lithotripsy. Further attempts to treat the culprit lesion by repeated inflations of greater than 20 atmospheric pressures with a 3.5 mm NC balloon helped to achieve a better angiographic result with no residual stenosis (Figures 2 A, B). A repeat OCT run confirmed good stent expansion and an MSA of around 4.75 mm2 (Figure 2 C).
Figure 2
A – Inflation with a 3.5 mm NC balloon. B – Final angiographic result with TIMI III flow. C – Repeat OCT run confirming good stent expansion and a minimum stent area of around 4.75 mm2
At this point a decision was made to stop as further aggressive dilatation could result in coronary perforation in an already unstable patient. In addition, further lesion modification could result in no reflow, thus compromising the final result. The patient eventually remained stable with thrombolysis in myocardial infarction (TIMI) grade 3 flow and following an uncomplicated recovery he was discharged 4 days later.
Long-term outcomes of treating stent thrombosis/restenosis are worse as compared to treatment of de-novo lesions [1]. Inadequate preparation of a calcified lesion, resulting in stent underexpansion, is a common cause of stent thrombosis [2]. Calcified lesions with calcium arc > 180°, maximum thickness > 0.5 mm, and length > 5 mm represent a well-recognized risk factor for stent underexpansion [3].
Treatment of stent failure due to underexpansion involves aggressive dilatation of the stent, as a means to optimize expansion. The treatment of such lesions can be extremely challenging, especially when there is underlying calcification, as they often do not respond to high-pressure balloon angioplasty with conventional non-compliant balloons. The pattern of calcification, as recognized by intravascular imaging, allows optimization of plaque modifying strategies. Hence, treatment escalation with more sophisticated devices such as scoring and cutting balloons, ultra-high-pressure balloons, rotational atherectomy, excimer laser coronary atherectomy or intravascular lithotripsy may be necessary in order to achieve an acceptable and durable result [2]. Intravascular lithotripsy appears to be a feasible, safe alternative for the management of stent underexpansion in heavily calcified coronary arteries, and it has been described in case reports and case series, although not licensed for treating stent underexpansion at the moment [4].
In conclusion, treating calcific stent underexpansion can be extremely challenging especially in an unstable patient. The use of intracoronary imaging and access to a wide range of technology can help in this challenging lesion subset. Sometimes though appropriate sizing of noncompliant balloons, by OCT, and high pressure balloon inflation can be sufficient to achieve acceptable stent expansion and lumen area.








