Summary
This is the first meta-analysis based on strict enrollment and outcome definition criteria in order to select only homogeneous studies and investigating immediate bleeding complications after dental extractions in patients on single (SAPT) or double (DAPT) antiplatelet therapy. Although the majority of studies report no excess bleeding on DAPT, we have proven that when pooling these data there is an increased risk of immediate bleeding, especially on acetylsalicylic acid and clopidogrel therapy.
Introduction
The management of dental extractions in patients on single (SAPT) or double antiplatelet therapy (DAPT) by dentists has raised major concerns since these therapies have become more widely used among patients after percutaneous coronary interventions. The number of patients receiving antiplatelet therapies is increasing annually [1]. The duration of these therapies for individual patients varies but is usually between 1 and 12 months for DAPT and sometimes lifelong for SAPT [2]. Moreover, new generations of more potent antiplatelet drugs have been introduced onto the market and recommended by the European Society of Cardiology (ESC) guidelines [2, 3]. The fear of potential bleeding risk during tooth extraction has been weighed against the fear of acute stent thrombosis, which is strongly linked to discontinuation of DAPT and may become fatal [4].
Safety of dental extractions in patients on chronic antiplatelet therapy either with only acetylsalicylic acid (ASA) or clopidogrel or with both combined has been a matter of debate for some time [5]. No clearly conclusive studies have been published either way, mainly due to low sample size. However, the results of the majority of them have proven the safety of dental extractions in the setting of antiplatelet drugs in comparison to naïve patients [6]. Unfortunately, only observational studies are available since no randomized clinical trials have been conducted.
In 2016 a position paper of cardiologists and dentists was published, which encourages maintaining single or double antiplatelet therapy in patients undergoing small surgical dental procedures [7]. The consensus advocates that management in such clinical scenarios should follow the scarce evidence that has been provided so far rather than putting patients at risk of cardiovascular events.
Aim
The aim of this paper was to perform a meta-analysis of published observational studies that met specific inclusion/exclusion criteria as described in the PICO Scheme below in order to study the effect of single and double antiplatelet therapy in comparison to controls on the occurrence of immediate local bleeding complications during dental extractions.
Material and methods
A systematic review and meta-analysis was conducted in order to answer the following focused question: “Do patients on antiplatelet therapy (single or dual) who undergo dental extractions without discontinuation of treatment when compared with healthy subjects experience more post-extraction bleeding complications?”
The following PICO scheme was applied.
Population
Inclusion criteria: Patients with dual antiplatelet therapy (ASA and clopidogrel) or single antiplatelet therapy (ASA or clopidogrel) during tooth/teeth extraction who did not terminate or withheld their treatment for the extraction procedure.
Exclusion criteria: Liver disease, alcoholism, current anticoagulant therapy, current non-steroidal anti-inflammatory drugs (NSAID) therapy or any chronic disease that could impact bleeding after extraction. Patients on ticlopidine (not recommended by the ESC guidelines) and prasugrel (only 2 patients in the entire meta-analysis population) and ticagrelor (no patients) were excluded from the analysis.
Intervention
Simple tooth/teeth extractions (without raising a mucoperiosteal flap) with the use of local anesthesia which treated primarily with local hemostatic measures that are usually applied by dentists (bite on a pressure gauze pad and/or placement of local hemostatic agent such as oxidative cellulose gauze, collagen or gelatin sponge, etc.)
Outcome
Postoperative bleeding event occurrence as defined by Lockhart et al. or based on this definition [8]. Prolonged immediate bleeding was defined as the need to use hemostatic gauze when blood extended beyond the tooth socket after 30 min of biting on a pressure pack. Studies where only VAS (Visual Assessment Scale) for bleeding severity was used were not included.
On May 3rd 2018 a PubMed, Scopus and EMBASE database search with no time-of-publication limits was performed. The search was conducted independently by two investigators. In case of any discrepancies the committee was organized with a third member to minimize selection bias. We used the following English phrases:
dual[All Fields] AND antiplatelet[All Fields] AND (“therapy”[Subheading] OR “therapy”[All Fields] OR “therapeutics”[MeSH Terms] OR “therapeutics”[All Fields]) AND (“tooth extraction”[MeSH Terms] OR (“tooth”[All Fields] AND “extraction”[All Fields]) OR “tooth extraction”[All Fields]) and
dual[All Fields] AND antiplatelet[All Fields] AND (“therapy”[Subheading] OR “therapy”[All Fields] OR “therapeutics”[MeSH Terms] OR “therapeutics”[All Fields]) AND (“tooth extraction”[MeSH Terms] OR (“tooth”[All Fields] AND “extraction”[All Fields]) OR “tooth extraction”[All Fields] OR (“dental”[All Fields] AND “extraction”[All Fields]) OR “dental extraction”[All Fields]).
We also searched the database with the additional words “aspirin”, “clopidogrel”, “prasugrel” and “ticagrelor” in the search phrase instead of “dual antiplatelet therapy” so as to extract all possible publications.
Due to the established strict PICO definition, for inclusion in the analysis, only papers which fulfilled patient inclusion and exclusion criteria as well as outcome measures described below were finally considered suitable to be used in qualitative and quantitative analysis. Only studies with all intergroup comparisons (DAPT, SAPT with ASA, SAPT with clopidogrel, controls) were included in the analysis. The above-mentioned process is also presented in the PRISMA flowchart (Figure 1). The risk of individual study bias was minimized due to strict study selection criteria and similarity of populations and outcome measurements in studies. Patients selection in all studies was based on consecutive patient (prospective or retrospective) enrollment. No external funding was used to perform this meta-analysis. All three studies entered into meta-analysis were approved by local bioethics committees. External funding was only reported for the Lu et al. study, which was supported in part by a CMRP research grant from the Chang Gung Memorial Hospital, Kaohsiung, Taiwan (CMRPG8C0642) [9].
Statistical analysis
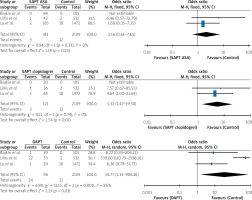
For each arm of all 3 trials the number of patients who experienced bleeding was collected as well as the total number of patients. The summary for all patients with bleeding events was presented as a percentage. The standard errors from arm-based data were transformed into standard errors for pairwise comparisons and the percentages were recalculated into odds ratios with the control as a reference group. Each of the considered trials presented results for each of the considered arms (SAPT with ASA, SAPT with clopidogrel, DAPT and control); hence all comparisons were direct head-to-head comparisons. The similarity of selected trials was assured with the detailed PICO scheme that allowed application of rigorous criteria to study population, design, outcome measures as well as patients’ characteristics and treatment – well known effect modifiers. Heterogeneity was assessed using Cochrane’s Q; the percentage of variation across studies due to heterogeneity rather than chance was expressed using the I 2 statistic. Random or fixed arm-based models were calculated depending on observed heterogeneity. Results were presented both with and without continuity correction (default value of 0.5) as sensitivity analysis. Results were visualized using forest and network plots [10–13]. Statistical analysis was performed by experienced statistician (KM) in R 3.3.2 (R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.) using the packages “meta” 4.9–2 “metafor” 2.0-0 and “netmeta” 0.9–8 as well as Review Manager [14]. P-values less than 0.05 were considered to indicate statistical significance.
Results
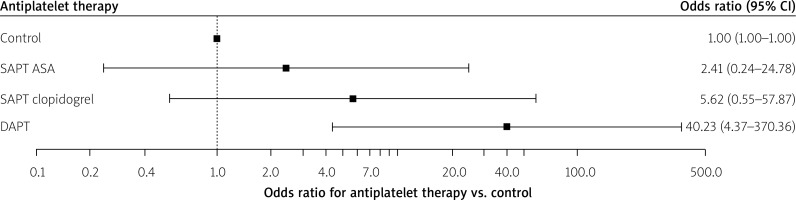
The search revealed 22 papers (21 in English and 1 in German). Nine papers were excluded from further analysis because they were review articles. Altogether 13 full papers were evaluated by the authors for potential meta-analysis. In total, three studies were finally included in this meta-analysis (Tables I, II). The three studies that were analyzed included 2673 patients and observed 42 patients with immediate bleeding events (1.59%). All these events were minor bleeding complications. Numerical data used for this meta-analysis were extracted and retrieved from the final PDF versions of all 3 papers (tables and text) and were available for all evaluated subgroups. Each of the analyzed studies included all considered arms; hence head-to-head comparisons were possible. Without applying continuity correction the analysis showed that patients receiving SAPT with clopidogrel and DAPT with ASA and clopidogrel had significantly greater odds for bleeding than the control patients. Such a result was not observed in terms of SAPT with ASA (Figure 2). Applying the continuity correction the result holds for and DAPT with ASA and clopidogrel only. The odds for SAPT with ASA as well as SAPT with clopidogrel were not significant when compared to the control group (Figure 3). The overall heterogeneity was significant with p-value for Cochrane’s Q test of 0.0002. As compared to the control group, the use of DAPT was associated with on OR of 40.23 (95% CI: 4.37–370.36) increase in risk of bleeding events occurrence (p = 0.0011). Significant heterogeneity was observed (p < 0.001; I 2 of 76.7%).
Table I
Papers included in the meta-analysis
| Author | Study type | IRB approval | Funding | Groups | Outcome |
|---|---|---|---|---|---|
| Lillis et al. | Prospective observational | Yes | None reported | SAPT with ASA, SAPT with clopidogrel, DAPT, Controls | Lockhart definition of bleeding applied [11] |
| Lu et al. | Retrospective registry | Yes | The study was supported in part by a CMRP research grant from the Chang Gung Memorial Hospital, Kaohsiung, Taiwan (CMRPG8C0642) | SAPT with ASA, SAPT with clopidogrel, DAPT, Controls | Immediate bleeding definition based on Lockhart [11] |
| Bajkin et al.* | Prospective observational | Yes | None reported | SAPT with ASA, SAPT with clopidogrel, DAPT, Controls | Lockhart definition of bleeding applied [11] |
Table II
Results of selected trials
| Study | Group | Number of patients with bleeding | Total number of patients | Percentage of patients with events (%) | OR (95% CI) vs. control* |
|---|---|---|---|---|---|
| Lu et al. | SAPT ASA | 2 | 185 | 1.1 | 1.60 (0.3474–7.3491) |
| SAPT clopidogrel | 2 | 65 | 3.1 | 4.64 (0.9960–21.6277) | |
| DAPT | 1 | 24 | 4.2 | 6.36 (0.7811–51.7263) | |
| Control | 10 | 1472 | 0.7 | – | |
| Lillis et al. | SAPT ASA | 1 | 42 | 2.4 | 6.46 (0.5739–72.7878) |
| SAPT clopidogrel | 1 | 36 | 2.8 | 7.57 (0.6701–85.5487) | |
| DAPT | 22 | 33 | 66.7 | 530 (110.7251–2536.9137) | |
| Control | 2 | 532 | 0.4 | – | |
| Bajkin et al. | SAPT ASA | 0 | 84 | 0.0 | 1.25 (0.0245–63.5811)^ |
| SAPT clopidogrel | 0 | 20 | 0.0 | 5.15 (0.0993–266.8422)^ | |
| DAPT | 1 | 39 | 2.6 | 8.22 (0.3279–206.1241) | |
| Control | 0 | 105 | 0.0 | – |
Discussion
The key finding of this meta-analysis is that there seems to be a significant increase in local bleeding complications in patients undergoing dental extractions treated with double antiplatelet therapy with ASA and clopidogrel in comparison to controls, which is contradictory to previously published results, which however were each time based on a small sample [9, 15–18].
There is a limited amount of published data concerning the topic of our analysis. The studies which are available are only observational prospective and retrospective samples of patients. On the other hand, even though our sample comprised over 2000 cases, the overall observed incidence rate of local immediate bleeding complications was very low (1.6%). A recently published meta-analysis concluded similarly that DAPT vs placebo carries additional risk for postoperative bleeding [19]. The main difference with our analysis is the inclusion of studies with various outcome measures defining bleeding. We also used only studies with direct SAPT, DAPT and control group comparisons.
Even though the majority of available observational data seem to support the safety of dental extractions in antiplatelet regimes, many dentists still fear the effect the antiplatelet therapy may have on bleeding complications [20, 21]. It is vital for the community of cardiologists to provide evidence-based recommendations for dentists (e.g. review or meta-analysis of existing data) in order to diminish the practice of possible discontinuation of DAPT or SAPT for dental extractions [7]. On the other hand, with the introduction of new, more potent antiplatelet drugs such as prasugrel and ticagrelor there is only one direct comparison in dental extractions, which revealed that prasugrel was associated with a considerably longer bleeding time than clopidogrel [22]. A recent study, which was not included in the meta-analysis due to conflicting outcome definitions, concluded that using ticagrelor as part of DAPT does not increase the bleeding risk after extraction [23].
In our opinion based on the published data and the results of this meta-analysis, the crucial factor influencing potential bleeding complications is not the antiplatelet therapy itself (no platelet testing for its real efficacy in the discussed papers was evaluated) but the extraction procedure and the management of the wound [5, 7, 8]. The operators’ skills and following strict dental algorithms to minimize the risk of bleeding (gauze pads, thrombin, sutures etc.) irrespective of the concomitant antiplatelet therapy play a key role in the success of dental extractions and preventing bleeding complications. It is also worth noting that the observed bleeding events were minor and did not carry additional risk for patients’ safety in all 3 papers included in the meta-analysis.
In order to minimize publication and data bias, we included in the meta-analysis only papers with a homogeneous outcome and clear extraction procedure descriptions and definitions. Only papers with all inter-group comparisons available with control groups were included in the meta-analysis. Statistical measures were undertaken so as to minimize the heterogeneity of the data. However, the small number of trials made it impossible to construct informative funnel plots and the test for symmetry was not performed following the recommendation by Sterne et al. [24].
The main limitation of this analysis is the lack of randomized clinical trials which could be included in the meta-analysis. However, in the face of a lack of randomized data we felt it is reasonable to investigate the existing data. It is also troublesome to pool published data since different outcome measures are applied in various papers. It also seems that the baseline profile of patients may play a potential role in the incidence of bleeding, e.g. the frequency of renal failure [18]. We tried to minimize this bias and finally included 3 papers so as to follow strict inclusion/exclusion criteria and similar outcome measures used in each manuscript.
Conclusions
Dental extractions following strict procedural protocols in patients on double antiplatelet therapy with clopidogrel and ASA are associated with an additional risk of immediate local bleeding complications. Based on our results there seems to be no controversy over the safety of dental extraction on SAPT. However, new studies with prasugrel and ticagrelor are desired in order to confirm the effect also in the new generation of antiplatelet agents, preferably in a randomized manner.