Introduction
Extracorporeal membrane oxygenation (ECMO) is a method utilized in ECMO centers as a rescue measure for support critically ill patients, often during ongoing cardiopulmonary resuscitation. However, new data and studies are emerging regarding the use of this method in providing cardiopulmonary support to critical patients, especially in cardiogenic shock. Increasingly, decisions are being made to use support already at the diagnostic stage as a “bridge to diagnosis” in critical patients.
Using a veno-arterial configuration of ECMO bypasses pulmonary circulation but provides cardiac support, allowing the heart to rest and recover while organ perfusion takes place. Such an approach is a bridge to “recovery, decision, or transplant” [1].
A meta-analysis including only observational studies demonstrated positive outcomes among patients in cardiac arrest or in cardiogenic shock supported with ECMO in the VA configuration compared with controls [2]. It is important to be aware of the risks that arise for patients at the moment of deciding on mechanical support – the risks of complications. It is already established and proven that the use of more robust systems and devices to provide cardiopulmonary support carries with it a greater number of risks of complications, especially severe ones. This is associated, not least, with the use of larger cannulas in the connection of support [3]. There are different opinions in the professional literature regarding the use of short- and medium-term mechanical cardiac supports overall and particularly in cardiogenic shock. The ECMO systems used for cardiovascular support (Centrimag, Abbott, Chicago, IL, USA and Cardiohelp, Maquet, Rastatt, Germany) cover complete cardiopulmonary support of patients, especially hemodynamic and gas exchange. The problem of randomized clinical trials comparing the results and efficacy of these methods lies in their limited number, the small number of patients and the prevalence of patients with myocardial infarction in these trials [4].
As long as there are no adequate clinical trials assessing meaningful clinical endpoints, the use of percutaneous mechanical circulatory support devices including ECMO support should be restricted to cases of refractory cardiogenic shock. For the time being, the reliance on our own experience in individual specialized centers also remains valid [5].
Aim
The purpose of this study was to evaluate hospitalization survival, short-term, and medium-term results in the ECMO patient group, with secondary objectives including identifying predictive factors influencing patient survival during VA-ECMO support.
Material and methods
This retrospective single-center study was conducted at the Cardiac Surgery Clinic of the University Hospital in Olomouc within the ECMO center. An analysis was performed on a cohort of 124 patients treated with VA-ECMO (119 peripheral and 5 central cannulations) for critical cardiopulmonary failure between 2012 and 2021. Ten patients were excluded from this cohort, as ECMO support was not initiated either due to cannulation for “back up” during extremely high-risk coronary interventions on the last patent coronary artery or due to technically unsuccessful cannulation. The analyzed dataset thus comprised 114 cases of full ECMO support.
In the dataset, age of the patients was secondarily analyzed for its correlation with duration of VA-ECMO support, length of hospitalization, hospitalization mortality, and survival.
Data collection and outcomes
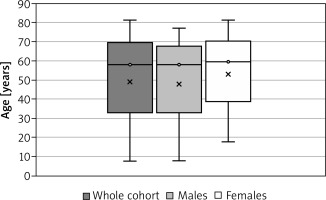
The cohort of 114 patients treated between 2012 and 2021 comprised 86 (75.4%) males and 28 (24.6%) females. The median age in the cohort was 58 years (range: 8–81 years), with a median age of 58 years for males (range: 8–77 years) and a median age of 59.5 years for females (range: 18–81 years).
The indications for VA-ECMO support are listed in Table I.
Table I
Indications for VA-ECMO support
Statistical analysis
The data are presented as percentages for categorical variables and as medians. Statistical analysis was conducted using IBM SPSS Statistics version 23 (Armonk, NY: IBM Corp. USA). The Mann-Whitney U test was used for analyzing continuous variables in independent samples. Spearman correlation analysis and the χ2 test were utilized. The level of statistical significance was set at p ≤ 0.05 for all analyses. We tested the normal distribution using the Shapiro-Wilk test. Figures were created using Microsoft Excel for Office 365 (Microsoft, Redmond, WA, USA).
Results
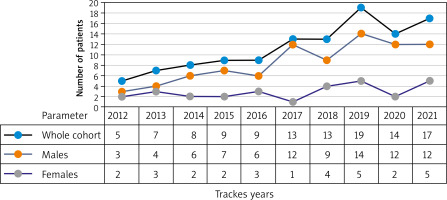
There was an annual increase in the total number of patients supported with VA-ECMO (Figure 1).
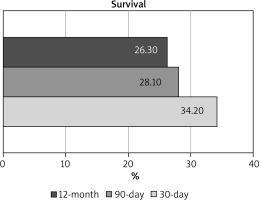
Overall hospitalization mortality was determined to be 73.7% (84 patients out of 114). The 30-day survival rate was 34.2%, the 90-day survival rate was 28.1%, and the 12-month survival rate was 26.3%. The results of overall hospitalization mortality, short-term, and mid-term survival are illustrated in Figure 2.
Figure 2
Survival of patients supported with VA-ECMO, percentage data: 30-day survival, 90-day survival, 12-month survival
The median duration of VA-ECMO support was 2.6 days. The median length of hospitalization after VA-ECMO support explantation was 2.5 days (range: 0–210 days), with a median hospitalization length of 4 days for males (0–210 days) and 0.4 days for females (0–102 days).
The representation of the age structure of patients is shown in Figure 3.
Analysis of duration of VA-ECMO support and length of hospitalization of patients in relation to age is presented in Table II.
Table II
Difference between males and females in age, duration of VA-ECMO support, and length of hospitalization after support explantation
No significant difference was found between males and females in age, duration of VA-ECMO support, and length of hospitalization after ECMO support explantation.
In the analysis of hospitalization mortality, short-term survival, and medium-term survival in relation to gender, no significant difference was observed (Table III). However, it is important to note that males comprised 75.4% of the analyzed patient group.
Table III
Difference in hospitalization mortality and survival at 30 days, 90 days, and 12 months between males and females
No significant difference was found between males and females in hospitalization mortality, short-term survival, and medium-term survival.
Another subject of analysis was the correlation between duration of VA-ECMO support and length of hospitalization after support explantation in relation to age. The results are presented in Table IV.
Table IV
Correlation between duration of VA-ECMO support, length of hospitalization after explantation, and age
| Age vs. | Duration of VA-ECMO support [days] | Length of hospitalization after explantation [days] |
|---|---|---|
| Correlation coefficient | 0.055 | –0.038 |
| P-value | 0.563 | 0.685 |
No significant correlation between duration of VA- ECMO support, length of hospitalization, and age of patients was found.
Analysis of the relationships between hospitalization mortality, survival at 30 days, 3 months, or 12 months, and age of patients is provided in Table V.
Table V
Correlation between hospitalization mortality, survival at 30 days, 3 months, or 12 months, and age of patients
No significant correlation was found between hospitalization mortality, survival at 30 days, 3 months, or 12 months, and age of patients.
The statistical analysis of patient survival in relation to the indication diagnosis in the given cohort showed no correlation and no significant difference.
Discussion
The most significant outcome of our study is the results of 10 years of experience in the ECMO program, including overall hospitalization (not just institutional) mortality of this patient group, short-term survival, and medium-term survival: (I) there is high hospitalization mortality among patients in this group; (II) no significant difference in hospitalization mortality or duration of ECMO support was found between males and females of varying ages; (III) no significant difference was found between males and females in survival at 30 days, 90 days, and 12 months; (IV) no significant association was found between duration of ECMO support and length of hospitalization in relation to patient age; (V) no significant correlation was found between hospitalization mortality and survival at 30 days, 90 days, and 12 months; (VI) no significant correlation was found between indications and survival at 30 days, 90 days, and 12 months.
No randomized controlled trials exist to date comparing Impella versus VA-ECMO because of difficulties in recruiting patients due to the acute nature of the condition. A number of non-randomized comparative studies have been published, most of which have been based on significantly different disease characteristics. Studies using propensity score matched/adjusted studies can reduce confounding by accounting for differences in important covariates that affect outcomes [6].
A systematic review from 2023, which included four randomized controlled trials, showed that the use of ECMO support was associated with an increase in 90-day to 1-year survival and a reduction in all-cause mortality at these intervals, but also a threefold increase in the risk of bleeding. However, the certainty of this result was only low to moderate, which is related to the small number of small studies, clinical heterogeneity of patients, and differences in study designs [7]. Venoarterial extracorporeal membrane oxygenation is one of the most aggressive forms of temporary mechanical circulatory support in current clinical practice because it is able to assume the function of both the lungs and heart. Therefore, the indication criteria for VA-ECMO are limited.
A high mortality rate is reported for patients with cardiogenic shock. Mortality from cardiogenic shock (most commonly associated with acute coronary syndrome, more specifically acute myocardial infarction) has been described as around 50% regardless of the availability of advanced ventricular assist devices [8].
According to a study comparing early ECMO support in cardiogenic shock with an early conservative approach allowing subsequent use of VA-ECMO in cases of worsening hemodynamics, early coupling did not improve clinical outcomes [9].
An important factor correlating with in-hospital mortality and survival is the number of patients treated annually. Centers with a higher number of patients treated (more than 100) have been shown to have lower mortality rates, including patients with previous cardiopulmonary resuscitation (CPR). For patients with previous CPR, the 30-day in-hospital mortality rate was estimated to be as high as 68.1%, which was significantly higher than the overall cohort [10].
Interesting results of a systematic review and metaanalysis were published by Bian W, 2023. This meta-analysis demonstrated that mild hypothermia (33–35°C) lasting at least 24 hours can greatly reduce short-term mortality and improve short-term neurologic outcomes in VA-ECMO-assisted patients without bleeding-related risks [11]. But the certainty of the evidence is still relatively low. Multiple randomized controlled trials are needed.
The subject of research among the key factors of survival of ECMO patients remains the question of nosocomial infections. Many studies pay close attention to this factor and show increased mortality in this group of patients.
The length of ECMO support as well as the length of treatment in the intensive care unit is longer in patients with infection compared to non-infected patients. According to a meta-analysis published last year and including 19 studies, nosocomial infection increases the risk of death (relative) among adult patients treated with ECMO by 32% [12].
Another important predictive factor that influences survival of patients after ECMO is the length of support. The technical feasibility of modern ECMO has increased the number of cases that have longer duration. Long-term management of ECMO results in an increased risk of complications associated with ECMO support. Anticipation of life-threatening mechanical complications and their management are essential for safe ECMO. The incidence of all life-threatening mechanical complications is reported to be around 4.0% [13].
The slight decrease in 2020 and 2021 is influenced by the emergence of the SARS-CoV-19 pandemic and its demands on the utilization of personnel and equipment at the clinic for VV-ECMO support of patients with acute respiratory failure, as well as a decrease in cardiac and other acute events such as acute heart failure and cardiogenic shock due to reduced population activity.
Limitations. This study provides important insights into the outcomes of using VA-ECMO in critically ill patients requiring external cardiopulmonary support, often in the pre-diagnostic and diagnostic stages within a single ECMO center over a period of ten years, the development of method implementation, and the prospects of identifying predictors of method success or failure.
The present study is a single-center retrospective analysis with limited information on long-term postoperative survival. There is no detailed information on late complications.
Conclusions
In our study, no difference was observed between men and women in terms of age, duration of support, or length of hospitalization after ECMO explantation. There was no difference between men and women in hospitalization mortality or survival rates, but the percentage of men in the study group was higher compared to women.
In the analysis of the ECMO patient group, a high overall hospitalization mortality rate was observed. One reason for this is the monitoring of survival not only within the institution but also tracking overall survival, including patients discharged from the clinic to other institutions or facilities. The 30-day survival rate was determined to be 34.2%, indicating a potential for reducing hospitalization mortality.
It is necessary to focus on predictors of effectiveness and failure of the method among the input criteria when making decisions, which will increase selectivity in the given group and may reduce mortality rates and improve patient survival prognosis.