Introduction
Hydatid disease is parasitic infection caused by the larval form of Echinococcus granulosus. It is endemic in many parts of the world: South America, Australia, New Zealand, the Middle East, and the Mediterranean region, including Morocco. In adults the liver is the first site (50–60%) followed by the lung (10–30%). The association of pulmonary and hepatic hydatid cysts may occur in 4–25% of patients [1–4].
Surgical management for concomitant pulmonary (right lung) and liver hydatid disease can be managed separately by two-stage surgery (TSS) or by a one-stage approach (OSS) via thoracophrenotomy,
Aim
The aim of this study is to evaluate our results in the treatment of concomitant pulmonary and hepatic hydatidosis by the two procedures and compare them.
To our knowledge, there is no similar work published in the French and English literature.
Material and methods
All data were from consecutive patients who were diagnosed with concomitant pulmonary and hepatic hydatid cysts following surgical resection in the Department of Thoracic Surgery, Mohammed V Military Teaching Hospital, Rabat, Morocco, between January 2008 and December 2019.
Data included age, clinical history, symptoms at presentation of pulmonary and hepatic hydatid cysts (Table I), preoperative radiological examination (Table II), surgical approach, postoperative complications, duration of hospitalization, interruption of activities and work, mortality and the follow-up.
Table I
Findings of the patients with lung and liver hydatid cyst
Table II
. Radiological data of the patients with lung and liver hydatid cyst
| Variables | TSS patients (n = 33) | OSS patients (n = 14) |
|---|---|---|
| Diameter of the lung cysts | 5–17 (8.6 cm) | 3–7 (4.7 cm) |
| Diameter of the liver cysts | 4–16 (9.7 cm) | 2–6 (3.8 cm) |
| Location: | ||
| Right lung: | 29 | 14 |
| Upper lobe | 1 | 1 |
| Middle lobe | 4 | 1* |
| Lower lobe | 24 | 12 |
| Left lung: | 4 | 0 |
| Upper lobe | 1 | |
| Lower lobe | 3 | |
| Liver: | 33 | 14 |
| Right lobe | 27 | 13 |
| Left lobe | 6 | 1 |
| Liver cysts’ site: | ||
| Bulging dome | 15 | 14 |
| Inferior segments | 12 | 0 |
| Anterior segments | 5 | 0 |
| Lung computed tomography: | ||
| Homogeneous masses | 15 (45.5%) | 7 (50%) |
| Floating membrane | 6 (18.2%) | 4 (28.6%) |
| Retention of membrane | 5 (15.6%) | 2 (14.3%) |
| Pseudo-tumor mass | 4 (12.1%) | 1 (7.1%) |
| Cavity | 3 (9.1%) | 1 (7.1%) |
| Liver: | ||
| Unilocular simple cyst | 18 (55.5%) | 7 (50%) |
| Multivesicular septated cyst | 12 (36.4%) | 5 (35.7%) |
| Heterogenous contents | 2 (6.1%) | 1 (7.1%) |
| Calcified wall | 1 (3.1%) | 1 (7.1%) |
The patients were divided into two groups: patients operated on by separate two-stage surgery through thoracotomy and later laparotomy (TSS patients, n = 33) and patients operated by one-stage surgery through thoracophrenotomy (OSS patients, n = 14).
Statistical analysis
All values in the text and tables were expressed as mean ± SD. The data were analyzed using the software IBM SPSS Statistics, version 21, IBM Corp.. Unpaired t-test, χ2 test, and Fisher exact test were used for group differences. A p-value less than 0.05 was considered statistically significant.
Operation duration, hospital stay and interruption of activities and/or work for patients managed by TSS are the sum of times at the first and second surgery.
Results
A total of 47 patients aged 18 to 76 years were included. There were 33 operated on by TSS (19 men and 14 women) and 14 by OSS (9 men and 5 women).
All the patients were symptomatic and the most of the symptoms were chest pain, abdominal pain in the right upper quadrant and cough (Table I).
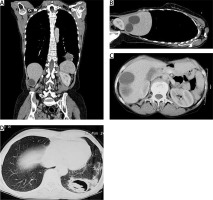
The diagnosis was established by chest radiography, abdominal ultrasonography, chest and abdominal computed tomography (CT) (Figures 1 and 2) in all patients.
Figure 1
Chest and abdominal computed tomography showing a large cystic lesion with floating membrane in the right lower lung lobe and a liver hydatid cyst (hepatic dome)
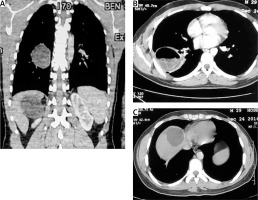
Figure 2
Chest and abdominal computed tomography showing a large ruptured cystic lesion with floating membrane in the left lower lung lobe and two cysts in the right lobe of the liver
Different radiological features found in the chest and abdominal CT scan are summarized in Table II.
All patient underwent serological tests by ELISA and were positive in 54.45% (18/33) in the TSS group and 57.14% (8/14) in the OSS group.
The primary surgical approach was open thoracotomy-phrenotomy for single-stage surgery (n = 14 patients), and thoracotomy followed by laparotomy (n = 33 patients) 3 to 20 weeks later (mean: 6.4 weeks).
For the one-stage surgery, a posterolateral thoracotomy is performed through the 6th, rarely through the 7th or 8th intercostal space. First the operating field is protected and isolated with sponges soaked in scolicidal solution (H2O2) in order to reduce the risk of spillage and dissemination of the scolices and daughter vesicles into the thoracic cavity and the pulmonary hydatid cysts are treated (cystotomy, pericystectomy exceptionally pulmonary resection).
Via a radial 4-5 cm phrenotomy, careful puncture of the liver hydatid cyst and aspiration of its content ensuring color examination (yellow or purulent) allowed a large cyst opening followed by extraction of the proligerous membrane and closure of the biliary fistulas (resection of the bulging dome).
Two Redon drains through the abdomen were inserted, one in the residual cavity and the second in the sub-diaphragmatic space. The diaphragm was closed in two layers with non-absorbable suture. One to two chest drains (24F to 32F) were inserted into the thoracic cavity.
The surgical procedures were as follows: cystotomy and pericystectomy with residual cavity capitonnage for most patients (n = 45; 95.74%) and lung resection for 2 patients (2 lobectomies) for destroyed pulmonary lobe by the cysts (Table III).
Table III
Operative and post-operative results of the patients
| Variables | Patients (n = 33) | Patients (n = 14) | P-value |
|---|---|---|---|
| Lung operation: | |||
| Cystotomy | 24 (72.7%) | 10 (66.7%) | 0.190 |
| Pericystectomy | 8 (24.2%) | 4* (26.7%) | 0.250 |
| Lobectomy | 1 (3.1%) | 1 (6.7%) | – |
| Capitonnage | 31 (93.9%) | 13 (86.7%) | 0.330 |
| Liver operation: | |||
| Resection of bulging dome | 29 (87.9%) | 12 (85.7%) | 0.350 |
| Partial pericystectomy | 4 (12.1%) | 2 (14.3%) | 0.460 |
| Pleural and diaphragmatic adhesion: | |||
| Partial | 19 (57.6%) | 7 (50%) | 0.056 |
| Total | 4 (12.1%) | 2 (14.3%) | |
| None | 10 (30.3%) | 5 (35.7%) | |
| Operation duration [min] | 154 (163–260) | 122 (95–210) | 0.047 |
| Post-operative complication: | 8 (24.3%) | 2 (14.3%) | 0.036 |
| Atelectasis | 2 (6.1%) | 1 (7.15%) | |
| Persistent air leakage | 1 (3%) | 1** | |
| Persistent biliary leakage | 2 (6.1%) | 1** (7.15%) | |
| Wound infection | 2 (6.1%) | ||
| Empyema | 1 (3%) | ||
| Hospital stay [days] | 13.8 (11–19) | 8.7 (6–15) | 0.022 |
| Mortality | 1 (3.1%) | 0 (0%) | – |
| Interruption of work and activities [days] | 56 (45–75) | 31 (25–45) | 0.045 |
| Follow-up period [months] | 28 (15–58) | 26 (8–54) | 0.412 |
For hepatic cysts resection of the bulging dome was performed in 41 (87.23%) patients and partial pericystectomy in 6 patients.
Postoperative complications (n = 10, 21.3%) were recorded essentially in the TSS group (8/33 = 24.3%). The postoperative complications are detailed in Table III.
There were significantly more complications in the TSS group (n = 8, 24.3%) than in the OSS group (n = 2, 14.3%) (p = 0.03).
The postoperative length of stay was significantly longer in the TSS group (13.8 days vs. 8.7 days, p = 0.022).
The interruption of activities and/or work for the TSS group was the sum of the 2 periods of convalescence after each intervention and there was significantly more interruption in the TSS group (56) than in the OSS group (31) (p = 0.045).
Discussion
Hydatid cyst disease is still a serious health problem in many countries worldwide. In adult the liver and lungs are the most common organs of involvement, the synchronic association of lung and liver hydatid cysts is not uncommon, and the incidence varied between 4% and 25% in the published series [5–7].
Hydatid cysts in the lungs are revealed by nonspecific symptoms – cough, chest pain, dyspnea and hemoptysis – but sometimes the presence of a pathognomonic sign of the diagnosis such as hydatidemesis (expectoration of the contents of the hydatid cyst (membrane or white liquid) [8].
Hepatic cysts are asymptomatic for a long time, but when they become giant or complicated (obstruction, rupture, infection, etc.), they may cause abdominal pain and the discovery of a palpable mass.
Radiological imaging including chest X-ray, abdominal ultrasound, thoracic and abdominal CT scan, and rarely MRI, allows one to make the diagnosis, to detect complicated forms, to differentiate the cystic nature of a mass, to search for the obstruction in the bile ducts and to plan the surgical approach, techniques and operative difficulties [9–11].
The classic surgical approaches to these two sites are sequential laparotomy and thoracotomy in a single or multi-stage procedure one to several weeks later.
Therefore, thoracotomy followed by laparotomy [7, 12, 13] or simultaneous surgical treatment of both locations by phrenotomy after thoracotomy is an approach widely used by several authors [1, 2, 7, 14, 15].
Rami-Porta et al. [7] reported before 1986 that only 13.3% to 57.6% of concomitant hepatic and right pulmonary hydatid cysts were treated by a simultaneous approach by thoracophrenotomy; currently this percentage is 83.5% for Kurul et al. [12].
In the drainage of the liver cavity, we do not use these drains through the pleura and leave the diaphragm open like some authors [16] who sutured the edges of the diaphragmatic incision to the edges of the residual cavity and drained with a catheter through the 9th intercostal space (pleural cavity) in order to isolate the peritoneal cavity and protect it from the flow of hydatid contents. In our practice, we do not use this method to avoid persistent communication between the liver and the pleural space.
Erdogan et al. [6] preferred obliteration of the residual cavity without placement of a drain because they found that external drainage causes prolonged drainage in non-suppurative cysts with appearance of a new biliary opening.
Kanojia et al. [17] presented a new approach to the treatment of a hepatic hydatid cyst through the diaphragm when associated with an ipsilateral pulmonary hydatid cyst by thoracoscopy. Patients underwent cystotomy of the pulmonary hydatid and resection of the bulging hepatic hydatid cyst by thoracoscopy. This approach has some limitations especially in non-bulging liver lesions through the diaphragm, cysts located in the anterior segments of the diaphragm and small or deeper liver lesions.
The size of the cyst is very important, because a large cyst can lead to enormous contamination of the peritoneal cavity, and in addition the management of the large residual cavity is difficult. The type according to the classification described by Gharbi et al. [18] and the complicated or uncomplicated nature of the pulmonary and/or hepatic cysts may require two-stage surgery rather than a single stage.
Moreover, the patient operated on by single-stage surgery avoids a second general anesthesia, additional postoperative pain and a second hospital stay. This allows a quick return to physical and professional activities and reduces the costs of treatment.
Based on our experience and data from the current study, we recommend performing two approaches (thoracotomy and laparotomy) in one or more steps with an interval of one to several weeks when the cyst is larger than 10 cm or in complicated forms, especially biliary complications or obstruction of the main bile duct [8].
Most authors managed pulmonary hydatid cysts by conservative techniques (cystotomy or pericystectomy with capitonnage), sometimes by sub-lobar resection or wedge and rarely by major resections such as lobectomy or exceptionally pneumonectomy [3, 6, 12, 19, 20]. For hepatic hydatid cysts they used different conservative procedures such as resection of the bulging dome, cystotomy and capitonnage [3, 6], sometimes segmentectomy or exceptionally right or left hepatectomy.
The rate of postoperative complications is low in the published literature, including in the hepatic compartment: minor or major biliary leakage [1, 5, 12, 21–23], bronchobiliary fistula [1, 12] or biliary-cutaneous fistula [2, 12], subphrenic abscess [7] and in the thoracic compartment: atelectasis; persistent air leakage; empyema, postoperative hemoptysis, suppuration of wound (Table IV) [14, 21–23].
Table IV
Post-operative complications and mortality in literature
Some authors report a high rate of complications (often minor): 56% for Lone et al. [23], 30% for Aghajanzadeh et al. [1] and 26.08% for Kir et al. [22]; Aribas et al. [21] report a 16% complication rate but they do not specify the percentage for each surgical strategy (Table IV).
However, in the majority of series using one-stage surgery, this complication rate is less than 5% [2, 5, 12].
In the literature, the mortality rate after surgical treatment of pulmonary and hepatic hydatidosis, especially with a one-stage approach, is zero regardless of the tactic used [1, 2, 5, 12, 21–23]. Athanassiadi et al. [16] report a very low rate between 0 and 4.2%.
Medical therapies have been used in the treatment of hydatid cysts; these drugs are indicated for inoperable patients with hepatic or pulmonary cysts, patients with multiple cysts in two or more organs, or peritoneal cysts [24], but the results have been variable.
The authors routinely prescribe benzimidazoles (albendazole or others) at a dose of 10 mg/kg/day preoperatively and postoperatively for 3 to 6 months, especially for patients with multiple hydatid cysts. The protocol is continuous or with a break interval of 1 week per month and monitoring of liver function [3].
Some authors believe that drugs are not necessary in the preoperative period, as they are responsible for complications, such as expectoration of membranes or even anaphylactic shock [2, 6, 25].
Medical therapy is mainly used in the postoperative period to prevent secondary recurrences.






