Summary
Patients’ knowledge of coronary heart disease and prevention is insufficient. Thus, we sought to identify sources of patients’ knowledge about cardiovascular prevention. Patients perceive physicians as the most reliable and trusted source of knowledge regardless of sociodemographic and clinical factors. Patients with higher education more often obtain their knowledge from books and the internet, whereas patients with lower levels of education more often rely on their cardiologist for their knowledge.
Introduction
Cardiovascular disease (CVD) is the leading cause of death in Poland [1–3]. It is strongly related to several risk factors, most of which can be modified and controlled. The major risk factors of CVD that can be controlled (modifiable) are: high blood pressure; high blood cholesterol levels; smoking; diabetes; overweight or obesity; lack of physical activity; unhealthy diet and stress. Those that cannot be controlled (conventional) are: age (simply getting older increases risk); sex (men are generally at greater risk of coronary artery disease (CAD)); family history; and race [4]. It has been shown that the proper management of those risk factors leads to a significant reduction in cardiac morbidity and mortality. Several studies [5–7] have demonstrated that knowledge of risk factors for CVD is poor among cardiological patients [8, 9]. However, the majority of patients expressed the need and a desire for more information [10]. In most European countries, information about heart disease such as heart failure is obtained from a general practitioner and then from a medical specialist. However, in Poland, most patients tend to visit the medical specialist in the first place [11]. Even the standard education provided during hospitalization significantly improves patients’ awareness, and the result might be magnified by further educational programs [12–15]. Currently, in Poland, the Kordian National Healthcare Program is provided for the prevention and education of CVD [16]. Despite all efforts undertaken for prevention, there is a paucity of data on patient preferences regarding sources of knowledge and forms of patient education on CAD.
Aim
We sought to determine the most popular and the most attractive way of education for the prevention of CVD.
Material and methods
This study was designed to evaluate the sources of patients’ knowledge about cardiovascular prevention according to sociodemographic and clinical profiles, which might be a basis for further projects on the creation and improvement of personalized educational programs. The study group consisted of 486 respondents including 200 patients admitted to the 2nd Department of Cardiology and Cardiovascular Interventions University Hospital in Krakow, Poland between July 2016 and October 2018 and 286 participants at the First Cardiological Patients’ Congress during the New Frontiers in Interventional Cardiology workshop in 2018. Data were collected using a 24-item self-designed questionnaire in Polish language (Figure 1). It was composed of 6 questions about the sociodemographic profile, 7 questions about the clinical profile, 7 questions assessing sources of knowledge and patients’ expectations and 4 questions referring to the self- assessed level of knowledge and motivation for CAD prevention. In questions regarding actual and preferable knowledge sources, patients were allowed to select more than one answer (multiple dichotomy). The inclusion criteria were: consent for participation in the study and hospitalization in the 2nd Department of Cardiology and Cardiovascular Interventions University Hospital in Krakow, Poland between July 2016 and October 2018 or participation in the First Cardiological Patients’ Congress during the New Frontiers in Interventional Cardiology workshop in 2018. The only exclusion criterion was the lack of consent for participation in the study. All included patients provided signed informed consent to participate in the study and consent to the processing of personal data. The study protocol was approved by the local ethics committee. The study was conducted in accordance with the ethical principles of clinical research based on the Declaration of Helsinki with its later amendments.
Statistical analysis
The normality of the data was assessed with Shapiro-Wilk test where applicable. The categorical variables were presented as number (percentage) and compared with the χ2 test. Normal distribution was observed for none of the quantitative variables; therefore they were presented as median and interquartile range (IQR) and compared with the Mann-Whitney test. Spearman’s correlation coefficient was applied to assess possible connections between the quantitative variables. The level of statistical significance was set at p < 0.05. The analyses were performed with Statistica v13 software (StatSoft, Inc., Krakow, Poland).
Results
The baseline characteristics of included patients and comparison of the popularity of knowledge sources are presented in Tables I and II. Of 486 patients included in the study, 332 (68%) suffered from CAD; 168 (35%) had undergone PCI; 363 (75%) reported hypertension, 130 (27%) diabetes, 65 (13%) atrial fibrillation.
Table I
Knowledge sources used by patients in groups according to sociodemographic and clinical factors. Part 1. Data presented as number (percentage)
Table II
Knowledge sources used by patients in groups according to sociodemographic and clinical factors. Part 2. Data presented as number (percentage)
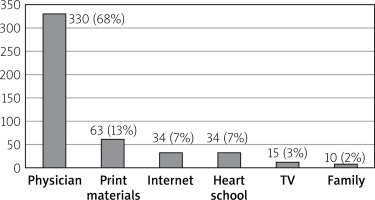
Cardiologists were reported as a source of knowledge more often by men than women (71% vs. 54%; p = 0.001) (Table I). Patients with CAD were more often educated by cardiologists (71% in CAD group vs. 42% in non-CAD group; p = 0.001). However, they used internet sources less often than patients with no CAD history (CAD vs. non-CAD: 25% vs. 41%; p = 0.002). Patients with higher education were more likely to use books (49% vs. 30%; p = 0.001) and internet sources (39% vs. 25%; p = 0.004) (Table II), but they were less prone to follow education provided by cardiologists, as compared to patients with lower levels of education (55% vs. 67%; p = 0.02) (Table I). Conversely, education provided by cardiologists and TV programs was more common in patients with a history of percutaneous coronary intervention (PCI) (for cardiologists and TV, respectively: 79% vs. 56%, p = 0.001; 30% vs. 16%; p = 0.001). Furthermore, a cardiologist as a source of knowledge was also more frequently reported in married patients (married vs. unmarried, widowed or divorced, respectively: 69% vs. 56%; p = 0.01) (Table I). Interestingly, 29% of respondents stated that they used help of the family to comply with medical recommendations. Moreover, almost a quarter of patients over 65 years old used internet sources (Table II). There was no difference in the popularity of individual online sources between those under 65, low and high educated, or rural and urban people in using online sources, except that more patients without a history of CAD seemed to use internet forums (p = 0.06). Detailed data are presented in Table III. The self-assessed level of knowledge correlated with the rate of provided education; however, the correlation was weak (Spearman’s rho: R = 0.26; p = 0.001). Patients indicated physicians as the most valuable source of knowledge (Figure 2). Healthcare professionals were indicated as the most preferable source of education regardless of the sociodemographic or clinical factors. A comparison of preferred forms of education is presented in Table IV.
Table III
Comparison of the popularity of particular internet sources of knowledge in groups according to sociodemographic and clinical factors
Table IV
Preferred forms of education in groups according to sociodemographic profile
Discussion
This study demonstrated that regardless of sociodemographic and clinical factors, patients perceive doctors as the most reliable and trusted source of knowledge. Thus, the crucial role of medical doctors in the education of patients should be emphasized. Our results are in line with previous studies [11, 17]. Patients preferred to visit cardiologists rather than general practitionera (GPs). Similar results were reported in the SHAPE study based on populations from Poland and Romania, whereas in the United Kingdom, Sweden, the Netherlands, France, and Germany, more respondents would go to their GP [11]. Furthermore, responders with CAD were educated more often by a cardiologist, but they used internet sources less often. A possible explanation for this observation could be that most patients are elderly, and they prefer personal contact with physicians than searching for information on the internet. Furthermore, older people are less familiar with computer and internet use. Nevertheless, the fact that people over 65 years old also use the internet cannot be ignored. In our study, it was 23%; thus this way of education should be more extensively used. Alarmingly, for many patients, the preferable form of internet knowledge sources is forums, which are considered as an unreliable source of knowledge. This highlights the crucial role of a doctor in educating the patients, which includes directing them to reliable websites. Clinicians should be aware of patients being misled by erroneous or commercially biased online content. Physicians should be able to redirect their patients to more robust, up-to-date sources [18, 19]. However, elderly people looking for information prefer printed material, verbal media, and physicians [19]. Interestingly, our study showed that patients with higher levels of education were more likely to use books and internet sources, but they relied less on education provided by cardiologists. It might suggest that they more often seek information on their own and consequently rely less on education provided by professionals. This might lead to incorrect conclusions if patients use sources incompatible with medical knowledge. Therefore, perhaps the solution is to recommend reliable books and websites by doctors. Patients with a history of previous PCI mainly used the care of a cardiologist, but they also preferred television programs. Generally, patients’ knowledge about cardiovascular prevention is insufficient and patients have poor knowledge and awareness of their CAD risk regardless of the history of revascularization [8, 9, 11, 19–21]. Most commonly older, male patients and people with risk factors of developing CAD, lower socioeconomic status, with lower education level, are more likely to have scarce knowledge about cardiovascular prevention [9, 22]. It is important to emphasize the fact that knowledge does not reduce risk factors of CAD by itself [23, 24]. It is only the first step to make people aware of the impact of adverse factors on the development and/or progression of CVD and the impact on both quality and life expectancy. In effect, patients should change their habits to improve health behaviors [9, 11, 21, 22, 25, 26]. To achieve this, it may be helpful to include spouses and other relatives in the educational process [27], as they can provide support in changing towards a more healthy lifestyle. In our study, 29% of respondents declared that they used the help of the family to comply with medical recommendations. Moreover, an interesting idea is participation in the Patient’s Club, which has shown significant benefits in terms of healthy lifestyle changes and more recommended management of cardiovascular risk factors [15]. More efficient education programs and educational materials should be provided to the population. Our study demonstrated experience from a large unselected cohort of Polish patients with CVD. Thus, it might reflect general trends in the level of knowledge about CVD prevention among the population in Poland. More comprehensive and personalized educational programs might improve the effectiveness of education and patients’ compliance [28]. It is important to underline the necessity of education provided by doctors as the most reliable and most preferred source of knowledge.
The study should be interpreted in light of several limitations. Our study is based on a single-center experience with a relatively small sample size. Furthermore, there is a potential selection bias. Participants of the First Cardiological Patients’ Congress were probably more interested in health issues, with more knowledge than other patients. A potential limitation is inclusion of patients without CAD. Despite diagnosis of other cardiovascular diseases, they might not receive knowledge about cardiovascular prevention. Furthermore, the questionnaire used in the assessment of patients’ knowledge and risk control levels was not validated. However, there is a lack of standardized tools for such assessment. The more studies are conducted, the better standardized questionnaires might be developed in the future.
Conclusions
Patients perceive physicians as the most reliable and trusted source of knowledge, regardless of sociodemographic and clinical factors. The principal findings were that patients with higher education more often obtain their knowledge from books and the internet, whereas patients with lower levels of education more often relied on their cardiologist for their knowledge. More comprehensive and personalized educational programs might improve the effectiveness of education and patients’ compliance.