The number of elective total knee arthroplasty (TKA) and total hip arthroplasty (THA) procedures performed in Poland has been growing in recent years. The National Health Fund (NFZ) data from 2005-2021 demonstrated that in Poland the number of TKAs increased from 4072 to 29614 annually, and the number of THAs increased from 26091 to 55337 annually [1]. In light of ongoing demogra-phic changes, it is likely that the increasing trend will continue.
Following exploratory interviews in the Polish community of orthopaedists and anaesthesio-logists, the authors noted a wide variety of peri-operative methods and procedures depending on the health care institution and medical practitioners’ own experience. To gain further insight into this area, a survey-based study was conducted to identify perioperative management practices used in this group of patients in Polish hospitals. The findings of the study, in combination with already exi-sting recommendations and international guidelines, may serve as a foundation for implementing a standardised perioperative care system in Poland. Since the study was multifaceted, the data pool was divided into issues related to preoperative and perioperative management separately and the results will be published in three independent publications. The financial aspects could not be ignored – multiplication of procedures and tests increase financial burden and extend redundant time of hospitalisation. One of main problems in that context seems to be excessive ordering of specialist consultations and using pre-defined sets of laboratory tests as ‘routine panels’, without taking into consideration individual clinical characteristic of each patient separately.
METHODS
The study was approved by the Bioethics Committee at the Jagiellonian University in Cracow (Decision No. 1072.6120.259.2020 of 24 September 2020). The study aimed to determine the contemporary clinical practice in terms of orthopaedic and anaesthetic preparation of patients for elective TKA and THA procedures in Polish hospitals. The questionnaire was compiled following a literature review. In this way, it was possible to determine the elements of therapy that are associated with clear benefits according to available scientific evidence, such as thromboprophylaxis, multimodal analgesia, regional nerve blocks, and early upright positioning. In addition, a number of elements for which there is no clear scientific basis were also identified, including preoperative antibiotic therapy in patients with asymptomatic bacteriuria, and selection of dose of tranexamic acid. The research survey was conducted in order to establish whether clinical practice in Poland is cohesive among local healthcare professionals and consistent with worldwide standards and guidelines.
Survey development
The survey’s questions were divided into two groups: survey 1 – for orthopaedists (30 questions) [Survey S1], survey 2 – for anaesthesiologists (24 questions) [Survey S2]. The analysis included responses both from medical specialists and physicians during their specialty training. The survey consisted of both single and multiple-choice questions, which was taken into account during statistical data analysis. The questions were drawn up in collaboration with the national consultants for Orthopaedics and Traumatology and Anaesthesio-logy and Intensive Care. In order to reach as many health care institutions and medical practitioners in Poland as possible, the LimeSurvey application (version 3.26.1+210427) [2] was used to generate an electronic questionnaire which was then shared online with survey participants. Any number of participants from each centre could take part in the survey. Participation in the study was anonymous and completely voluntary.
Survey validation
The survey was designed and executed by the study investigators. After creation of initial version of the survey it was spread among investigator’s close local collaborators in the area of anaesthesio-logy and orthopaedics with enquiry to complete the survey and share their opinion and feedback regarding survey itself. After taking into conside-ration their comments the survey was adjusted accordingly.
Data collection
The survey was sent to all health care institutions in Poland performing elective TKA and THA procedures in adult patients. A list of health care institutions was obtained from the National Health Fund (NFZ) data thanks to collaboration with the National Centre for Quality Assessment in Healthcare. The study was promoted through websites, in social media channels, and via personal contacts. It was carried out in two rounds: 17 May – 30 July 2021 and 3 August – 24 August 2021. One person was responsible for contact with all health care institutions (all centres were phone called twice in each round, two weeks apart). All gathered data will be kept in secure files for 10 years.
Statistical analysis
Analysis encompass responses regarding ordered laboratory tests, additional tests, specialist consultations, providing prehabilitation, setting of preanaesthetic evaluation in matter of place and time before surgery, applying perioperative protocol, possibility of providing fast-track approach to TKA and THA procedure. Analysis covered also comparison of approach between anaesthesiologists and orthopaedists as well as possible influence of responder. The results obtained in the study were analysed statistically with the R and Python programming languages using appropriate data analysis libraries. Since the survey responses were binary, Yates’s χ2 test was applied for the purpose of comparison. For multivariate modelling, logistic regression was used. Only complete responses were included in the analysis, so the denominator varied slightly between questions depending on the number of missing responses. To determine the measure of concordance across the medical centres, an intraclass correlation coefficient was used.
RESULTS
A total of 162 health care institutions took part in the study. Survey responses were submitted by 93 (57%) orthopaedics teams and 112 (69%) anaes-thesiology teams. A total of 187 responses from orthopaedists and 299 responses from anaesthesio-logists were obtained. In 41 medical centres, survey responses were provided by both groups of medical practitioners. In 63 (39%) centres, responses were submitted by at least two physicians of a given specialty. More than half of the respondents were from small hospitals (< 600 beds), and the highest number of responses came from medical practitioners with over 20 years professional experience. Fewer laboratory tests were found to be ordered in larger hospitals. Table 1 lists data on the medical practitioners’ length of work experience. Table 2 summarises the responses of orthopaedists and anaesthesiologists to the question regarding routine ordering of laboratory tests prior to elective TKA and THA procedures.
TABLE 1
Comparison of survey responses submitted by medical practitioners (by medical specialty and length of work experience)
| Work experience | Anaesthesiology (n = 239) | Orthopaedics (n = 131) |
|---|---|---|
| < 5 years | 45 (19%) | 13 (10%) |
| 6–10 years | 67 (28%) | 21 (16%) |
| 11–15 years | 40 (17%) | 12 (9%) |
| 16–20 years | 18 (8%) | 16 (12%) |
| > 20 years | 69 (29%) | 69 (53%) |
Values are presented as number (percentage).
TABLE 2
Laboratory tests ordered by medical specialty
[i] Values are presented as number (percentage). A detailed table including responses distribution of all questions concerning laboratory tests is placed in the Supplement Table 1 APTT – activated partial thromboplastin time, INR – international normalized ratio, CRP – C-reactive protein, ESR – erythrocyte sedimentation rate, BNP – B-type natriuretic peptide, NT-proBNP – N-terminal pro-brain natriuretic peptide
The survey findings show that mean (standard deviation) 7.2 (SD 3.5) laboratory tests are routinely ordered preoperatively. Figure 1 shows relationship between the length of work experience and the number of ordered laboratory tests by medical practitioners. 75% of orthopaedists and 92% of anaesthesiologists routinely order an ECG test, while 36% of orthopaedists and 32% of anaesthesiologists refer patients for an X-ray. Table S2 lists the number of routinely performed additional examinations, and Table S3 – imaging evaluations of the surgical site. Data on specialist consultations are summarised in Table 3. Overall, 18% of anaesthesiologists and 79% of orthopaedists refer patients for at least one specialist consultation on a routine basis.
FIGURE 1
Relationship between length of work experience and number of ordered laboratory tests: ESR, CRP, urinalysis, dental consultation, and no preoperative consultations
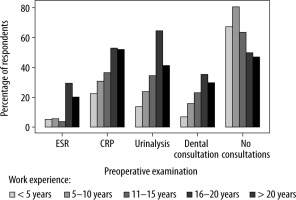
TABLE 3
Specialist consultations ordered by medical specialty
Six medical centres participating in the study submitted more than 10 responses to the survey questions in both study groups. The intraclass correlation coefficient (ICC) was calculated as 0.6-0.8. On that basis, the correlation of responses was confirmed.
A statistically significant difference was noted between the groups as regards the frequency of ordering CRP and ESR tests, urinalysis, and consultations with a cardiologist, gynaecologist, laryngologist, and internal medicine/family physician (Figure 2).
The findings of the study regarding patient edu-cation, preoperative rehabilitation, management of asymptomatic bacteriuria, place and time of preanesthetic evaluation are summarised in Table 4. A comparison of responses by medical specialty, work experience or hospital size showed no significant differences between these groups.
FIGURE 2
Comparison of frequencies of preoperative examinations ordered by ortho paedists and anaesthesiologists
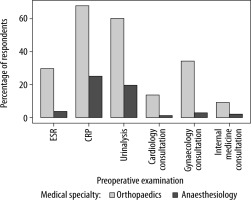
TABLE 4
Intervention of patient’s education, preoperative rehabilitation, management of asymptomatic bacteriuria, place, and time of pre-anaesthetic evaluation
The survey also addressed the application of a standardised perioperative procedure. A total of 87 (29%) anaesthesiologists confirmed application of such regarding both surgery types, four (1.3%) only for TKA, and one (0.3%) only for THA. In contrast, in the group of orthopaedists, there were 126 (67%) confirmative responses for TKA and THA, four (2.1%) for THA only and one (0.5%) answer for TKA only. Standardised perioperative procedures were implemented more commonly in small medical centres compared to large hospitals. More laboratory tests and consultations were ordered in the health care institutions using perioperative procedures.
Figure S3 presents a comparison of incidence of laboratory tests and consultations ordered by medical practitioners (expressed as percentage), in reference to perioperative procedure application and hospital size.
Same-day TKA and THA procedures are performed in just four hospitals in Poland.
Discussion
Appropriate preoperative preparation for TKA and THA procedures is of fundamental importance, as it has a direct impact on the risk of perioperative complications [3]. The survey showed that physicians performing patient eligibility assessment for surgery and preanaesthesia evaluation order a wide panel of laboratory tests (e.g. CRP, ESR, glucose, urinalysis), imaging assessments, and specialist consultations. Most orthopaedists order a urinalysis before surgery, even in patients not presenting symptoms of urinary tract infection. Patient education is provided primarily during the assessment of eligibility for TKA/THA or upon hospital admission. However, more than half of orthopaedists do not routinely prescribe preoperative rehabilitation. More examinations and consultations are carried out in hospitals, where a perioperative protocol is followed.
Guidelines of the Canadian Anaesthesiology Society (CAS) [4] and practice advisory issued by the American Society of Anaesthesiologists (ASA) [3] highlight that preoperative evaluations should not be performed on a routine basis [3, 4], but selectively, to guide or optimise preoperative management [4]. The ASA has additionally defined clinical characteristics of patients to be used by anaesthesiologists, as an aid in decision-making process. A slightly different approach has been taken by the authors of the UK’s National Institute for Health and Care Excellence (NICE) guidelines, who advise that the panel of tests should be selected depending on the extent of surgery, taking into conside-ration the ASA system, with TKA and THA classified as major procedures [5]. The European Society of Anaesthesiology and Intensive Care (ESAIC) supports the NICE guidelines without any modifications [6]. Tables 5 and 6 list the NICE, ASA and CAS guidelines content together with specific types of laboratory tests and additional examinations recommended.
TABLE 5
Detailed NICE, ASA, and CAS guidelines for different types of laboratory tests
TABLE 6
Detailed NICE, ASA, and CAS guidelines for different types of additional examinations
In 2016, the Polish Agency for Health Technolo-gy Assessment and Tariff System prepared a report [7] presenting an expert statement based on global guidelines published before 2016. The report lists a set of tests and examinations, which are required before surgery (ECG with interpretation, urinalysis, CRP, CBC with differential, electrolytes, and glucose) and a panel of recommended tests (urea, creatinine, and coagulation profile). The guidance was drawn up based on a review of a total of 24 clinical practice guidelines. However, it is worth noting, that only New Zealand’s 2014 guidelines mention routine performance of laboratory tests, urinalysis, and ECG. Other recommendations supports an individualised approach, taking into account chronic diseases and perioperative risk [7]. The high number of tests ordered in Poland may thus be linked to the findings presented in that report.
Laboratory tests, additional examinations, specialist consultations
Haemoglobin, haematocrit (complete blood count)
There is a consensus among scientific societies that a haemoglobin test should be performed preoperatively on a routine basis (major surgery, risk of intraoperative bleeding) in order to prepare the patient better for complications, if any should occur, or pursue further diagnostic workup [8]. Untreated preoperative anaemia is known to prolong hospitalisation and elevate perioperative mortality rates. According to ESAIC guidelines in case of revealing an anaemia, serum iron level should be assessed and treatment of known iron deficiency initiated with intravenous iron supplementation before elective procedures [6].
Patient blood management (PBM) is wider topic than only screening and treating anaemia. Nowadays experts all over the world emphasize need and importance of implementing cohesive blood management programs in health care systems. The concept involves also i.a. minimizing blood loss, mana-ging coagulopathic bleeding, focusing on preserving a patient’s own blood [9]. The crucial issue is shared decision-making, involving patient’s perspective [10]. Implementing a PBM program creates opportunity to achieve additional benefits for patients (such as lower morbidity, mortality and reduced LOS in hospital and the ICU, fewer complications) and optimise transfusion related costs of hospitalisation [11]. PBM was not covered in the survey and should be investigated in a dedicated research.
Coagulation system (APTT, INR)
According to the NICE guidelines coagulation tests are not deemed essential in patients classified as ASA 1-2, regardless of the extent of surgical procedures. In the ASA 3 and 4 groups, coagulation tests should be considered only in patients with concomitant liver diseases. Based on the ASA and CAS guidelines, the performance of these tests should be made conditionally, basing on factors including the type of surgery and its invasiveness. It needs to be highlighted, that anaesthesiologists often need coagulation parameters to determine the optimal type of anaesthesia (central block, regional block).
Biochemical tests
According to the available guidelines, biochemical testing should be considered and specific tests selected depending on the patient profile [4]. The NICE guidelines, which are usually restrictive, prescribe that eGFR, creatinine, urea, and electrolyte tests should be carried out in all ASA 2-4 patients, but in the ASA 1 group only in patients who are at risk of developing AKI [5]. ASA 2 patients are those with chronic conditions, that are well controlled pharmacologically, but their medications may affect electrolyte levels or impair renal function. The analysis of study findings shows that Polish medical practitioners have a very liberal approach to routine biochemical testing. The vast majority order biochemical tests regardless of whether patients have any comorbidities or not. In addition to generating high costs, this practice may cause undue delay in TKA and THA procedures. Particularly noteworthy observations include high rates of inflammatory marker tests (CRP and ESR) performed in patients without signs of infection. The NICE, ASA and CAS guidelines do not mention these tests, probably because they are regarded as unwarranted in patients showing no clinical signs of infection (elective procedures). The position of orthopaedists is presented in the expert consensus statement [12] ‘Implantation of joint prosthesis in patients with active inflammation should be deferred until complete healing confirmed by laboratory tests’. Consequently, negative history of active inflammation is not an indication for routine CRP or ESR tests.
Troponin and NT-proBNP tests
In Poland, these tests are not performed on a routine basis. According to the CAS guidelines, they should be considered in patients aged over 65 years or presenting with major cardiac diseases. ESC 2022 guidelines change the recommendation class to I for high-sensitivity troponin testing before intermediate or high-risk surgical procedures and 24 hours and 48 hours after surgery in patients with cardiovascular disease [8].
Urinalysis
The NICE and ASA guidelines clearly identify patients presenting with symptoms of urinary tract infection, as the only group benefiting from the urine test. Screening for asymptomatic bacteriuria causes an unwarranted delay in performing surgery, and leads to further tests (microbiology, CRP, procalcitonin) and unnecessary antibiotic therapy, which has a direct impact on the development of antibiotic-resistant bacteria and increases the costs. According to the available evidence, in the population of women over 80 years of age, one in 10 has asymptomatic bacteriuria [13]. Orthopaedists agree that urinalysis should not be performed on an obligatory basis, but be reserved for patients with active or history of urinary tract infection [12].
Additional examinations
Similarly to the 2022 ESC guidance, anaesthe-siology guidelines unequivocally endorse ECG screening in patients with cardiac diseases or cardio-vascular risk factors. In ASA 1 patients, NICE and ESC experts additionally recommend ECG in patients over 65 years of age. With respect to chest X-ray, the guidelines do not advise routine imaging examinations, restricting them to patients with respiratory or cardiovascular conditions.
Specialist consultations
Experts agree, that specialist consultations should only be carried out if the benefits outweigh the risks associated with delaying the procedure and additional costs. In fact, there are two situations to be considered in this context: diagnosis of a new disease or inadequate control of an existing medical condition. In Poland, specialist consultations are ordered far too often, particularly by orthopaedists (only 21% do not refer patients for any consultations on a routine basis).
Prehabilitation
Prehabilitation refers to all interventions performed prior to surgery in order to improve patients’ health status and physical performance, reduce perioperative mortality and accelerate recovery. In 2021 findings of a systematic review and meta-analysis were published in BMJ, which identified four interventions reducing the length of stay (LOS) and the rate of postoperative complications: immunomodulatory nutrition, breathing exercises, gene-ral fitness exercises, and multimodal prehabilitation. The authors of the review highlighted that prehabilitation was safe, and no adverse effects of these interventions were reported in any study [14]. It should be noted that worldwide, in several health care systems prehabilitation is a permanent element of perioperative care, whereas in Polish health care system it is not centrally provided- patients have no access to any structured education and rehabilitation program other than local initiatives.
Asymptomatic bacteriuria
There is scientific evidence both for [15, 16] and against a correlation between asymptomatic bacteriuria and implant infection [17, 18]. A 2018 metaanalysis found no such association [15]. To date, antibiotic therapy has not been proven to be of value in reducing implant infections following treatment of asymptomatic bacteriuria [14]. On the other hand, according to orthopaedic practice guidelines, patients with asymptomatic bacteriuria can be operated on safely, provided that they receive perioperative antibiotic prophylaxis, which is routine in all cases [12].
Protocols
The application of standardised perioperative intervention protocols aims to reduce patients’ LOS and the rate of complications, including postoperative mortality [19-21]. At present, the most widely used care protocol is ERAS (Enhanced Recovery After Surgery). In 2020 took place a publication of the findings from a multicentre, prospective observational study assessing the relationship between the use of the ERAS care protocol and postoperative complications after elective TKA and THA procedures. The application of the protocol was shown to reduce the rate of postoperative complications. Moreover, specific interventions of the greatest importance were identified, including the use of regional or local anaesthesia, appropriate mana-gement of anaemia and bleeding, and early mobilisation of patients. The study also found that not all the principles of the protocol were properly adhered to, even in units that recognise themselves as ERAS-compliant [22]. In addition, achieving the benefits of the protocol requires cooperation between medical team members and the patient [21]. In Poland, paradoxically, more examinations and consultations are ordered by medical practitioners following the procedures. Therefore, a question arises as to what standardised protocols are in place and whether they are being implemented adequately.
Fast-track TKA and THA procedures
Increasing social expectations to reduce the LOS while maintaining the safety and quality of patient care open up new directions for changes. Prospective scientific studies provide evidence for the safety and efficacy of fast-track programs [23, 24]. In 2020 Drosos et al. published a retrospective analysis of data collected prospectively for 434 patients undergoing TKA and THA procedures. The paper outlined a three-step process of modification of perioperative procedures, including step I – physiotherapy, step II – blood transfusion program, step III – multimodal pain management [25]. Each stage lasted nine months, with new regimens successively implemented and further components added. The literature data demonstrated clear medical, social and financial benefits, indicating the need to reorganise work [23, 24, 26].
Same-day TKA and THA procedures are performed in only four hospitals in Poland. Effective and safe modernisation of the Polish perioperative care system requires careful planning and training of medical professionals, followed by stepwise implementation, while allocating an appropriate amount of time for adaptation.
Preanaesthetic evaluation before TKA and THA
Studies available in the literature show the benefits of early assessment of patients in anaesthesia clinics. Preoperative anaesthesiology assessment should be multidisciplinary and planned in advance adequately prior to scheduled surgery, in order to optimise chronic conditions e.g. iron deficiency [8]. Research has demonstrated a decreased number of cases of patient’s ineligibility for procedure on the scheduled surgery date [27], reduced LOS and lower costs of care [28]. Blitz et al. [29] reported lower perioperative mortality in the group of patients assessed for eligibility for surgery in an anaesthesia outpatient clinic. Research findings are incorporated into guidelines issued by scientific societies (as summarised in Table S4).
In Poland, according to the Regulation of the Mi-nister of Health, which has been in force since 2016, preanaesthesia evaluation should be carried out at least 24 hours before scheduled anesthesia [30].
LIMITATIONS
As we approach the responders in several possible ways to increase the response rate, we do not know the exact denominator of studied group. It should be noted, that the response rate in the orthopaedic group was lower than in anaesthesiologists group. There was also no prior sample size calculation performed as we planned the study to have exploratory character. Concerning the questionnaire, PMB was not covered in the survey. In authors’ opinion it was impossible to fulfil complex PBM aspects in a comprehensive way in this questionnaire and keep it concise at the same time.
CONCLUSIONS
The survey helped to identify elements of preoperative care which should be modified to improve the safety and quality of TKA and THA procedures. The following conclusions were reached:
– laboratory tests should be individualised depending on the patient’s disease profile;
– tests including urinalysis, CRP, ESR and glucose should not be ordered on a routine basis;
– PBM is prominent part of preoperative preparation. This area requires further investigation in Poland and should assume growing importance;
– ECG and chest X-ray should be individualised depending on the patient’s disease profile;
– patients should not be referred for specialist consultations if their chronic disease is stable;
– preoperative rehabilitation and education should be provided to patients in a standardised and systematic manner;
– standardised surgical protocols should be applied with due diligence. In case of difficulties with their full implementation, the implementation of their major components should be pursued;
– fast-track TKA and THA procedures are both safe and effective;
– the number of patients undergoing preanesthetic evaluation before elective procedures in an anaesthesia outpatient clinic should be increased;
– cooperation between anaesthetic and surgical teams is fundamental to the quality and safety of patient hospitalisation.
The conclusion arising from the study results’ analysis is that perioperative care in Poland needs standardisation, in a form of formally binding guidelines or recommendations.




