Venous thromboembolism (VTE), which encompasses deep vein thrombosis (DVT) and pulmonary embolism (PE), remains an important cause of worldwide morbidity and mortality. Acute venous thromboembolism affects about 1 to 2 per 1000 individuals each year in Europe and the United States, and venous thromboembolism is responsible for over 3 million deaths worldwide each year [1, 2]. The increase in incidence of VTE is seen with malignancy, immobilization, surgical interventions, and genetic predispositions [3]. Cancer-related VTE accounts for approximately 20% of the total burden, while recent hospitalization, including surgery and acute medical illness, account for 50% to 60% of the overall VTE burden [4]. Extensive thrombosis of the inferior vena cava (IVC) and bilateral iliac veins poses unique therapeutic challenges, particularly when complicated by PE, due to the high risk of both fatal PE and chronic venous insufficiency. Anticoagulation to prevent clot extension and recurrence has long been the traditional treatment of DVT and PE [5]. Nonetheless, in situations of significant thrombus burden or failed attempts to achieve therapeutic levels of anticoagulation, invasive options such as mechanical thrombectomy represent an attractive alternative. Here, we report the successful use of mechanical thrombectomy with the ClotTriever system (Inari Medical, Irvine, California) to remove these thrombi from large veins with regard to minimizing systemic lytic exposure and with a focus on safety and efficacy in patients with contraindications to thrombolysis. This was a challenging case of a 66-year-old female patient who presented acutely and was found to have extensive thrombosis in the IVC, bilateral iliac veins, and left renal vein, with an associated central right-sided PE. She was ineffectively managed with anticoagulation, necessitating mechanical intervention. An incidental finding of a right-sided breast mass, subsequently confirmed to be invasive ductal carcinoma, was discovered during evaluation. This a case demonstrates the utility of the ClotTriever thrombectomy in cases of extensive thrombosis, as well as the need for coordinated multidisciplinary care, particularly in the setting of suspected malignancy as an inciting etiology.
A 66-year-old woman with a medical history of asthma presented to a local hospital with acute back pain and dyspnea, which she had been experiencing over the previous week. The workup based on CT showed an extensive thrombus within the IVC, reaching the iliac veins bilaterally and the left renal vein, along with a centrally located right-sided PE (Figure 1). The patient had no prior history of malignancy, coagulopathies, or recent heparin exposure; however, her family history was positive for breast cancer, experienced by her mother. Although anticoagulation therapy with heparin was initiated, the patient’s condition continued to deteriorate, showing signs of venous congestion. Due to the degree of thrombosis and her refractory response to anticoagulation, she was referred to our tertiary care center for further management. On admission, there was bilateral lower extremity edema, as well as lower oxygen needs. Detailed radiological studies and a vascular assessment demonstrated significant thrombotic burden and an incidental right-sided breast mass, with an average size of 1.1 × 1.5 cm (Figure 2). Due to the severity of the thrombosis, mechanical thrombectomy was undertaken using the ClotTriever system (Figure 3). Bilateral femoral access was obtained, and four passes of the device were conducted on each side, resulting in the successful extraction of acute and subacute thrombus fragments (Figure 4). The total duration of the procedure was about 55 min, with no blood loss or need for thrombolytic therapy. Postoperatively, the patient showed significant clinical improvement and resolution of her lower extremity edema. Anticoagulation therapy was switched to apixaban on day 2 postoperatively, and Class II compression stockings were applied. Postoperative computed tomography (CT) follow-up showed only minimal residual thrombotic material adherent to the wall of the inferior vena cava and right renal vein, of no clinical significance (Figure 5). The patient also underwent a biopsy of the right breast, with the lesion being histologically diagnosed as an invasive ductal carcinoma. After discussion with the oncology team, a treatment plan was made to place a subcutaneous port for neoadjuvant chemotherapy in an attempt to shrink the neoplasm before surgical resection. She received 12 cycles of neoadjuvant chemotherapy and subsequently underwent surgical excision of the tumor. Pathological finding of the resected tissue suggested an invasive ductal carcinoma of no special type (NST), grade 2. Upon admission to the oncology ward, comprehensive hematological and hemostasiological workup was performed to clarify suspected underlying thrombophilia or other types of coagulopathies. All tests were normal, and there was no evidence of hereditary or acquired clotting disorders. Therefore, its extensive thrombosis was attributed to a paraneoplastic mechanism, presumably secondary to the newly diagnosed malignancy. After initiation of neoadjuvant therapy and surgical resection of her malignancy, this patient was transitioned to adjuvant care with continued anticoagulation and serial oncology follow-up for long-term management.
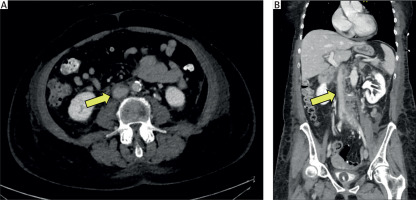
Figure 1
Preoperative CT scan images showing extensive thrombosis: A – Transverse section of the inferior vena cava with thrombus (arrow). B – Iliac veins with thrombus (arrows). C – Femoral veins with thrombus (arrows). D – Coronal section of the inferior vena cava with thrombus (arrow). E – Sagittal view of the inferior vena cava with thrombus (arrow). F – Pulmonary embolism in the left pulmonary artery on transverse view (arrow). G – Coronal view of the pulmonary embolism (arrow)
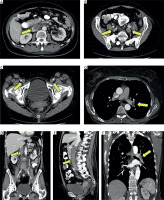
Figure 2
Imaging of the detected tumor in the right breast (arrow): A – CT scan, B – mammography, C –breast ultrasound
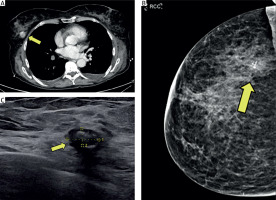
Figure 3
Intraoperative angiography images: A – thrombotic occlusion of the right iliac vein, B – thrombotic occlusion of the left iliac vein. C – thrombotic material in the inferior vena cava, D – result after thrombectomy
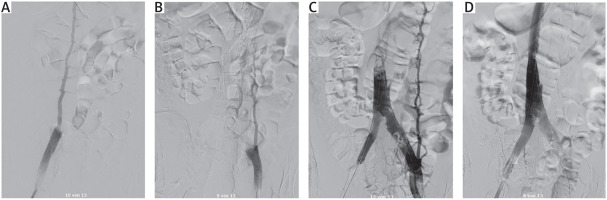
Figure 4
Intraoperative images demonstrating thrombectomy using the ClotTriever system: A, B – ClotTriever device in use, C – bifemoral approach for interventional thrombectomy, D – total thrombotic material removed, corresponding to the mass occluding the inferior vena cava
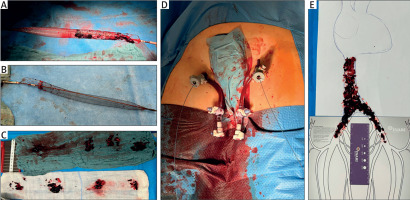
Figure 5
Postoperative CT scan showing the reopened inferior vena cava with minimal residual thrombotic material adhering to the vessel wall
IVC thrombosis, especially when it extends to the renal veins and into the iliac veins, is a challenging clinical condition. Its presence not only increases the risk of recurrent embolic events and chronic venous insufficiency but can also lead to significant risk of sudden cardiac or respiratory compromise from thrombus dislodgement [6, 7]. In this patient, the ARDS-like acute symptoms of back pain and dyspnea, along with imaging abnormality of extensive IVC thrombus and PE, led to the need for prompt and aggressive management. Due to her large thrombotic burden and inadequate therapeutic response to anticoagulation treatment efforts, the decision was made to proceed with endovascular mechanical thrombectomy using the ClotTriever device.
The ClotTriever system enables mechanical retrieval of thrombus in the larger venous structures affected by such disease, such as the IVC and iliac veins [8]. The patient was at high risk for thrombi during surgery and had a heavy thrombus load, rendering catheter thrombolysis ineffective; thus, this approach was chosen. Additionally, thrombolytic therapy is frequently associated with increased risk for bleeding complications. Here we present the use of the ClotTriever, illustrating the versatility of the device in the management of extensive venous thrombi where other therapies are contraindicated or otherwise would provide suboptimal results. The ClotTriever system was chosen for thrombectomy due to its unique advantages in managing large venous thrombi. Unlike catheter-directed thrombolysis (CDT), which requires prolonged infusion of thrombolytic agents and carries a high risk of bleeding complications, the ClotTriever device enables mechanical clot extraction in a single session without the need for thrombolysis. This aspect is particularly crucial in patients with malignancy, who often have an increased risk of bleeding due to underlying coagulopathies or chemotherapy-related thrombocytopenia. The device is specifically designed for large-bore mechanical thrombectomy, featuring a self-expanding nitinol coring element that effectively engages, disrupts, and retrieves organized thrombus material while minimizing endothelial trauma. Additionally, ClotTriever allows for rapid blood reinfusion, reducing procedural blood loss and eliminating the need for extracorporeal circulation [9–11].
Thrombolytic therapy is even riskier, and its application not only increases bleeding risk, but also places a heavy burden on intensive care units, which are extremely expensive and, in many hospitals, limited [12]. Bilateral femoral access was obtained, and thrombectomy was performed via four passes of the device on each side for the successful extraction of acute and subacute thrombus material. The procedure took about 55 min, resulted in substantial thrombus load reduction, and was without significant complications, including blood loss or transfusion of blood products. Postoperative imaging demonstrated marked reduction in the extent of thrombus, and the patient showed significant clinical improvement, with resolution of lower extremity edema. Considering the extensive thrombotic involvement and the recent diagnosis of malignancy, a comprehensive hematological and hemostasiological investigation was performed to exclude differential diagnoses for the thrombotic predisposition. Testing, including a complete panel for inherited and acquired thrombophilias, was performed and returned within normal limits, excluding common coagulopathic contributors. Hence, the thrombosis was attributed to a paraneoplastic origin, instigated by the newly diagnosed breast cancer-induced pro-thrombotic milieu. Paraneoplastic thrombosis or cancer-associated thrombosis, mediated by malignancy-associated procoagulant factors, is a well-recognized phenomenon that may specifically be seen more frequently with newly diagnosed or aggressive cancers, with VTE appearing as the presenting sign of cancer, and can even be witnessed up to 6 years prior to a diagnosis of cancer [2]. The 6.1% of undiagnosed cancer prevalence at VTE diagnosis increases to 10% within 12 months [13]. This highlights the need for comprehensive diagnostic workup, as in our case, imaging obtained during the initial VTE workup unmasked a malignancy – aggressive and invasive – enabling appropriate surgical and chemotherapeutic intervention in a timely manner. In the patient’s care, a multidisciplinary approach by vascular surgery, oncology, hematology, and interventional radiology teams was necessary. The earlier mechanical thrombectomy provided symptomatic relief and reduced the immediate threat of PE and further embolic events. Meanwhile, the oncology team organized the workup for the incidental breast lesion, which was confirmed to be invasive ductal carcinoma that would require neoadjuvant chemotherapy. The tumor was surgically resected following chemotherapy. The entire treatment course was supported by ongoing anticoagulation and preventive measures to manage her thrombotic risk. This case demonstrates the benefit of a comprehensive, multidisciplinary approach to the care of patients with extensive VTE and concomitant malignancy. Application of the ClotTriever offered a valuable therapeutic option that allowed for rapid thrombus clearance. Concurrent oncologic management was instituted for the underlying malignancy, likely contributing to reducing the patient’s continued thrombotic risk. The eventual successful management of the patient’s acute thrombotic events and the establishment of long-term management for her underlying malignancy serve to highlight the potential advantages offered by coordinated multidisciplinary management in the context of complex clinical problems.
Other large-bore mechanical thrombectomy systems, such as the AngioVac device, have also been employed in cases of extensive venous thrombosis. The AngioVac system (AngioDynamics, Latham, NY) is designed for veno-venous extracorporeal thrombectomy and employs an aspiration cannula connected to an external bypass circuit with a centrifugal pump and filter. While the AngioVac is highly effective for retrieving large thrombi, it requires systemic anticoagulation, a controlled surgical setting, and potentially longer procedural times due to the need for extracorporeal circulation. These factors can limit its use in cases where anticoagulation poses a significant risk, as in patients with malignancy or active bleeding concerns. Additionally, the AngioVac is primarily indicated for floating thrombi rather than wall-adherent thrombi, making it less optimal in cases involving extensive chronic venous thrombi or mixed acute-subacute clot burdens, such as in this patient [14, 15].
Several other large-bore mechanical thrombectomy devices are available for managing extensive venous thrombi. The FlowTriever system (Inari Medical), primarily designed for pulmonary embolism, provides effective clot extraction without thrombolytics but necessitates large-bore access [16]. The AngioJet system (Boston Scientific) combines mechanical fragmentation with pharmacologic thrombolysis but carries a risk of endothelial injury and post-thrombotic complications [17]. Lastly, the Aspirex system (Straub Medical) uses rotational thrombectomy for acute and subacute thrombi but is less effective for chronic cases [18]. The ClotTriever was chosen in this case due to its ability to remove large, organized thrombi in a single session without thrombolysis, anticoagulation, or extracorporeal circulation, making it particularly advantageous in a patient with malignancy-associated thrombosis. Compared to other devices, the ClotTriever offers a distinct advantage by enabling direct mechanical thrombectomy without systemic anticoagulation or thrombolysis, making it particularly useful in patients with contraindications to anticoagulants. Furthermore, the absence of extracorporeal circulation with the ClotTriever simplifies the procedural setup, reduces the risk of hemodynamic instability, and shortens the overall intervention time. Given these benefits, the ClotTriever system was the preferred choice in this case, allowing for a rapid, effective, and safe thrombectomy in a patient with a high thrombotic burden and an underlying malignancy-associated hypercoagulable state.
This case stresses the advantages of mechanical thrombectomy for use in cases of extensive thrombosis of the IVC and iliac veins, especially where conventional anticoagulation therapy fails to work or is contraindicated. The ClotTriever maneuver resulted in significant thrombus reduction with immediate symptom relief. The multidisciplinary approach involving vascular intervention, hemostasiological study, and oncologic management was instrumental in achieving a successful outcome. A diagnosis of cancer-associated thrombosis associated with incidental invasive breast carcinoma was made based on negative hemostasiological results. Having different fields of expertise work together within an intensive care plan and share the responsibilities of careful drug use along with routine laboratory work for screening and substitution are the key elements which allowed us to manage the extensive thrombotic process in this patient, as well as the underlying malignancy, paving the way for her successful recovery and long-term management as an outpatient.






