Iatrogenic aortocoronary dissection (IACD) is a rare (estimated to occur in 0.039% of cases) but potentially fatal complication of percutaneous coronary intervention (PCI) [1]. The mortality rate is 6.4%, though this may be underestimated due to selective reporting bias [2]. Heavy calcifications are a potential predisposing factor for IACD [2]. In such scenarios, bailout rotational atherectomy (RA) may be the treatment of last resort, despite dissection being commonly cited as a contraindication for RA [3–5].
We present the case of an 83-year-old female patient with unstable angina who was referred for PCI of the left descending artery (LAD) following Heart Team consultation and patient preference. Her medical history included previous stroke, sustained atrial fibrillation, peripheral artery disease, arterial hypertension, and hypercholesterolemia. Echocardiography showed no significant abnormalities.
The procedure was performed via right radial access using a 6F Extra Back Up (EBU) 3.5 guiding catheter. Initial optical coherence tomography was unsuccessful due to probe inability to cross the proximal LAD lesion. Predilation with a 1.5 × 15 mm balloon at 14 atm resulted in retrograde dissection extending to the left main coronary artery (LMCA) and ascending aorta (Dunning Class II, involves the ascending aorta but extends less than 40 mm). Subsequently, no balloon could pass beyond the dissection. We elected to perform RA using a 1.25 mm burr, changing to a Rotawire Floppy via a Finecross microcatheter. Following successful bailout atherectomy, we completed the PCI with deployment of three drug-eluting stents. The final angiography demonstrated complete sealing of the dissection origin with no residual aortic contrast staining. Follow-up computed tomography angiography confirmed complete healing of the aortic root (restitutio ad integrum). The patient was discharged on post-procedure day 5 (Figure 1).
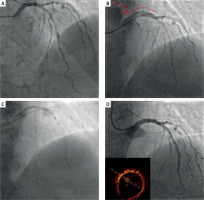
Figure 1
Angiographic sequence of iatrogenic aortocoronary dissection (IACD) management with rotational atherectomy. A – Baseline coronary angiography showing multiple lesions in the proximal and mid left anterior descending artery (LAD). B – Retrograde IACD extending from the proximal LAD to the left main coronary artery (red arrow), classified as Dunning Class II. Despite preserved distal LAD flow, no devices, including low-profile balloons, could cross the dissection plane. C – Bailout rotational atherectomy with a 1.25 mm burr using pecking-motion technique to minimize complications. D – Final angiographic result after deployment of three drug-eluting stents, with optimal stent apposition confirmed by optical coherence tomography
This case illustrates management of a rare PCI complication involving retrograde LMCA dissection with aortic extension. While conservative management may be considered for IACD, progressive dissection and symptom development necessitated immediate intervention. Given that unsuccessful stent delivery in this scenario carries significant mortality risk, bailout RA was essential for procedure completion. We selected the smallest available burr to minimize the risk of intimal flap enlargement. The RA proceeded without complications and enabled adequate stent expansion, as confirmed by optical coherence tomography. In cases where dissection sealing fails or PCI is unsuccessful with concurrent hemodynamic instability or persistent symptoms, surgical intervention should be strongly considered.








