Introduction
Uterine fibroids present a common cause of gynecological complaints among women of reproductive age. In addition to symptoms such as heavy bleeding, pelvic pain, and compression of adjacent organs, fibroids often negatively affect fertility, leading to difficulties with conceiving and maintaining successful pregnancy [1, 2].
Traditional treatment approaches include surgery such as hysterectomy and myomectomy, which provide lasting symptom relief but also either eliminate the possibility of conception or are associated with surgical risks [3, 4]. Uterine artery embolization (UAE) offers an alternative by providing effective symptom control through fibroid node ischemia, preserving uterine integrity. This procedure is very suitable especially in women who want to avoid surgery or are not fit for surgery due to extreme obesity.
Despite its promising results, UAE raises questions about its impact on future fertility and obstetric outcomes, including the risk of miscarriage, placenta previa, and preterm delivery [5, 6]. This case report examines the possibility of successful conception and delivery after two successive UAE procedures.
Case report
Patient history
A 31-year-old female patient presented with complaints of heavy menstrual bleeding (menorrhagia), dysmenorrhea, and a heaviness in the pelvic region that had persisted for more than two years. The symptoms significantly reduced her quality of life, also resulting in mild iron deficiency anemia.
Transvaginal ultrasound revealed a 7 × 6 cm intramural fibroid node that deformed the uterine cavity. The patient was admitted to the University Hospital “Medica Rousse” on 2016-01-08 with consecutive intermenstrual bleeding. Laboratory tests on admission revealed mild anemia (Hb 114g/l). The rest of the hematological parameters were in the normal ranges.
The patient expressed a strong desire to preserve her uterus and childbearing functions as she had no prior birth. After discussing suitable alternatives including myomectomy, she opted for UAE. After 14 months, the patient spontaneously became pregnant. At the 38th gestational week, she delivered via cesarean section.
On November 25, 2019, the patient, now 35 years old, returned to the hospital with similar symptoms and was diagnosed with a recurrent intramural fibroid node, with a size of 6 × 6 cm. Symptoms included heavy vaginal bleeding, dysmenorrhea, and longer periods, resulting in significant discomfort and a lower quality of life. Laboratory tests showed a Hb level of 123 g/l. After discussing therapeutic options, the patient again opted for UAE as a method for managing the symptoms and expressed her desire for a second pregnancy. In the 10th month after UAE, she became spontaneously pregnant. At the 38th gestational week, she delivered via cesarean section.
Diagnosis and treatment
Uterine artery embolization procedures
Both UAE procedures were performed under local anesthesia and sedation by a specialized interventional radiology team (Fig. 1). The left brachial artery was catheterized up to the uterine artery. A 2.8 Fr microcatheter was used. Target vessels supplying the fibroid node were identified by intravenous injection of contrast medium. Super-selective embolization was applied to the arterial branch feeding the fibroid. Polyvinyl alcohol particles with a size of 700 µm were used for the first UAE.
Fig. 1
A) Uterine artery embolization (UAE) of right uterine artery. B) UAE of the left uterine artery
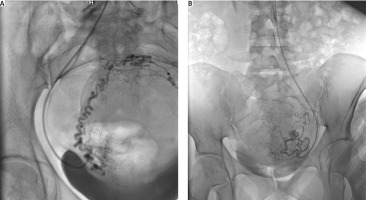
For the second UAE procedure, the uterine artery was accessed again through the left brachial artery with a 2.8 Fr microcatheter. The polyvinyl particles used were 900 µm in size.
Postprocedural angiographic images confirmed complete occlusion of blood flow without significant collateral circulation to the fibroid. The same procedure was performed on the right uterine artery.
Post-procedure recovery
In both cases of UAE the patient experienced mild to moderate post-embolization syndrome including:
moderate pelvic pain managed with non-steroidal anti-inflammatory drugs,
mild fever of up to 38°C (100.4°F), which subsided within 48 hours,
nausea and discomfort resolving within 3–5 days.
After both procedures, the patient was discharged after 48 hours of observation with recommendations for regular follow-up.
Follow-up and conception
Following the first uterine artery embolization procedure
The patient reported feeling significantly better within three months following the procedure:
the heavy menstrual bleeding was significantly reduced,
pelvic discomfort was eliminated,
ultrasound examination showed a size reduction of the fibroid by about 50%. At the third month following the first UAE, Hb was 134 g/l.
Fourteen months after the procedure, the patient spontaneously became pregnant, whereas the recommendation was to avoid pregnancy for at least 18 months after the UAE. Regular follow-ups included ultrasound examinations to assess fetal growth rate and placental localization.
Following the second uterine artery embolization procedure
Similar improvements were observed after the second procedure. Fibroid size reduction and Hb – 142 g/l were observed at the third month follow-up appointment.
Again, despite the recommendations to avoid pregnancy for at least 18 months, the patient became spontaneously pregnant 10 months after the procedure.
Course of pregnancy
Both pregnancies were fairly uneventful and developed without significant complications to the third trimester. Highlights include:
Follow-up examinations: The patient underwent regular ultrasound examinations, including three detailed fetal morphology check-ups at a specialized fetal medicine center during both pregnancies;
First parturition: An elective cesarean section at 38 weeks was performed. The newborn was a healthy girl, with a weight of 2930 g, height of 48 cm, and an Apgar score of 9 out of 10;
Second parturition: The second pregnancy also ended in a live birth via an elective caesarean section at 38 weeks – another healthy girl was born, weighing 2850 g, with a height of 50 cm, and an Apgar score of 9 out of 10.
Discussion
Uterine artery embolization was performed for the first time in 1995 by Ravina et al. to treat uterine myoma [7]. So far, substantial evidence has accumulated in the literature about the safety and effectiveness of this procedure as a non-surgical option for treatment of uterine fibroids [8]. Uterine artery embolization is increasingly used in medical practice and has numerous indications that can be systematized as gynecological indications (strong and less strong) and childbirth-related causes (Table 1).
Table 1
Indications for uterine artery embolization
The pain and pressure-related symptoms include bloating, increased frequency of urination, constipation and nocturnal urination. Despite its widespread use, the procedure has some relative and absolute contraindications (Table 2).
Table 2
Contraindications for uterine artery embolization
All types of fibroids are classified according Munro et al.’s classification [9].
There are a lot of studies reporting that UAE is safe for patients who desire to preserve their fertility. Firouznia et al. highlighted successful pregnancies after UAE despite an increased risk of complications such as placenta previa [10]. Homer and Sarıdoğan reported similar results, noting the importance of regular follow-up [11]. Similar results have been reported by other authors [12–14].
In a direct comparison of myomectomy with UAE, both methods improved quality of life but myomectomy shows greater benefit to women [15]. However, UAE has some advantages which cannot to be ignored [11, 16, 17]:
UAE does not carry risks of adhesions and complications for future pregnancies that are common for conservative myomectomy;
UAE is a minimally invasive procedure with a shorter recovery period;
UAE offers a wide range of options for performing the procedure itself, e.g., access via the brachial artery when femoral artery catheterization poses challenges; selectively occluding a specific branch of the uterine artery or blocking blood supply to the artery as a whole.
Ludwig et al. analyzed and synthesized data from 12 clinical studies and quantified the possible complications and pathologies related to pregnancy and parturition after UAE [18]. They presented the following data:
ratio between the number of successful and desired pregnancies,
miscarriage rate among confirmed pregnancies,
the percentage of preterm deliveries,
the ratio of cesarean compared to vaginal births.
The data set was also compared against the previously mentioned complications in the general population to assess the contribution of UAE to their occurrence. The total number of women, under the age of 40, who underwent UAE procedures and desired pregnancy was 672. Of them, 268 women conceived. Thus, the percentage of pregnancies achieved averaged 39.9% across all 12 studies, with successful conception rates in the general population ranging 75–95%. Given that the studies also tracked and reported subsequent pregnancies among the participants, the total number of successful pregnancies among the 268 women was 320.
Of these 320 pregnancies after UAE, the average miscarriage rate was 33.1% (106 miscarriages). The average miscarriage rate among the general population is in the range of 15–25%.
Preterm delivery occurred in 28 of 171 pregnancies for which data regarding this criterion are available in the study. Thus, the average rate of preterm deliveries following UAE was 16.4%, whereas the average rate among the general population is around 12.6%.
According to the data provided, out of the total 187 that reached full term, 115 were cesarean deliveries. The cesarean delivery rate following UAE was 61.5%, compared to 31.9% in the general population. In contrast, the proportion of cesarean vs. vaginal deliveries among the general population is only 31.9%.
The visualization of the quantitative relationship of pregnancy- and parturition-related complications, which we have calculated based on the data set provided by Ludwig et al. [18], between women treated for symptomatic leiomyomas via UAE procedures and the general female population is given in Table 3.
Table 3
Comparison of pregnancy and childbirth complications between post-uterine artery embolization women and the general population [18]
It is notable that UAE is associated with a higher risk of pregnancy and birth complications. Some of them are admittedly also due to anatomical and physiological uterine changes due to the fibroids themselves. The lower chances of conception are due to both the anatomical changes caused by the leiomyomas and the varying uterine atrophy following an UAE procedure.
The risk of miscarriage and preterm birth is also higher compared to the general population, but the ratio of these complications is significantly closer in incidence to the general population when compared to the chances of conceiving. This correlation indicates that for women who are able to conceive after UAE, the functionality of the uterus (its ability to carry a full-term pregnancy) is not significantly compromised, compared to that of the general population.
Although myomectomy was discussed with the patient as a conservative method for treatment with preserving reproductive functions, she chose a UAE procedure.
The present case is unique because it demonstrates:
Successful consecutive conception following each of the two separate UAE procedures;
Lack of serious complications (placenta previa, placental abruption, abnormal sites of placental attachment, uterine atony) despite the shorter than recommended time interval between both UAE procedures and conceptions;
To our knowledge, there have been no other cases worldwide, where two consecutive pregnancies following two consecutive UAE procedures were carried to term and resulted in two live births, without pathological abnormalities during either gestation or parturition.
This case highlights the need for an individualized approach to patient care, with interdisciplinary collaboration between obstetricians, interventional radiologists, and maternal-fetal medicine specialists playing a key role.
Conclusions
Uterine artery embolization is a promising minimally invasive alternative to myomectomy for women with fibroids who want to preserve their fertility. The present case demonstrates that successful conception and childbirth are possible when patients undergo close follow-up and individualized management.











