Iatrogenic coronary artery dissection is a rare but possibly life-threatening complication of interventional procedures such as coronary angiography and angioplasty. It is mainly caused by the disruption of the intima of the coronary artery and it can proceed anterogradely leading to occlusion of the coronary artery lumen, or retrogradely into the aortic wall [1]. When it involves the latter one it is referred to as iatrogenic aorto-coronary dissection. The optimal treatment has not yet been established since it is often patient-dependent, and therefore no clear guidelines exist.
We present a case of a 62-year-old woman with unstable angina, hypertension, type 2 diabetes mellitus and obesity who underwent percutaneous coronary intervention (PCI) complicated by dissection of the right coronary artery (RCA) that progressed into the ascending aorta. Before the procedure she had been admitted to the local hospital with a retrosternal pain. She had a positive family history for coronary artery disease as her father died of myocardial infarction at the age of 42. Additionally, she had been an active smoker for many years. Importantly, she had no connective tissue disease diagnosed or family history of any aortic disorders. The coronary angiogram revealed 70–80% stenosis of the left ascending artery (LAD) and subtotal occlusion of the non-dominant RCA. During PCI of the RCA, after introducing the 5F guiding wire the dissection of the RCA and adjacent aorta occurred. In a rescue manner, three drug-eluting Xience Pro stents were implanted.
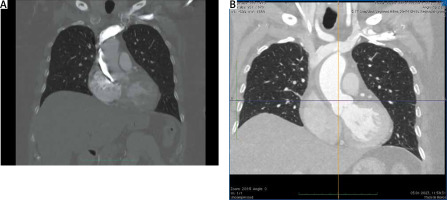
Despite these maneuvers, the no-reflow phenomenon was observed. The emergency computed tomography (CT) angiography revealed a dissection at the right-lateral side of the aorta propagating to the level of the brachiocephalic trunk (Figure 1 A). Of note, the ascending aorta was not dilated, with a maximal diameter of 34 mm.
Figure 1
A – Computed tomographic angiography (CTA) of the ascending aorta after iatrogenic injury; additional contrast in the right lateral side of the aorta fills a false lumen after coronary angiogram. B – CTA of the ascending aorta 3 days after the injury
The patient was immediately transferred to the cardiac surgery department. On admission she was responsive, in verbal contact and without chest pain. Blood pressure was 160/100 mm Hg and heart rate 73 beats per minute. The electrocardiogram (ECG) showed normal sinus rhythm and ST segment elevation in V1-V2 and rV3-rV6. The transthoracic echocardiogram showed no pericardial effusion and normal morphology and function of the tricuspid aortic valve. There was a visible flap of dissection in the right Valsalva sinus. Additionally, there were mild mitral and severe tricuspid insufficiencies. Left ventricular ejection fraction (LVEF) was 55% with hypokinesis of the basal segments of the intraventricular septum and left ventricular inferior wall. Moderately increased troponin I concentration and CK-MB activity were the only abnormalities found in the laboratory tests.
After stratified risk of early mortality (26.6% according to the EuroSCORE II calculator) was presented, the patient was not convinced of surgery as the only reasonable solution. Eventually, the heart team decided to proceed with conservative management as this high-risk patient presented stable hemodynamics and additionally was unfavorable for aorto-coronary bypass of the RCA (relatively narrow epicardial segments). Pharmacological oral and intravenous blood pressure control and double anti-platelet therapies (clopidogrel + acetylsalicylic acid) were continued. On the second day of hospitalization, the patient developed first degree AV block and needed temporary pacing. Eventually a permanent pacemaker was implanted. Moreover, one cycle of hemodialysis was performed due to acute kidney injury. Follow-up CT angiography performed a few days later showed a hypotensive area in the right lateral side of the aorta (7 mm in thickness) from the level of the aortic valve to the beginning of the brachiocephalic trunk, which might have corresponded to a thrombosed false lumen (Figure 1 B).
The patient was finally disqualified from cardiac surgery and was transferred in a stable clinical condition to the local cardiology ward for further treatment. The discharge transthoracic echocardiogram revealed not only improvement in the LV contractility (LVEF of 65%) but also less severe tricuspid valve insufficiency than previously. PCI of the LAD in a month’s time was recommended.
The incidence of catheter-induced iatrogenic aorto-coronary dissections is low; the exact range varies among studies, and it is estimated to be less than 0.6% of all procedures [2]. Dunning et al. [1] reported 9 patients with aortic dissection after more than 40 000 cardiac catheterizations. The IRAD (International Registry of Acute Aortic Dissection) included 28 cases of iatrogenic type A aortic dissections after interventional cardiological procedures and/or cardiac surgery, which constituted 5.3% of all aortic dissections [2].
Risk factors of this complication have not been well defined, but older age, hypertension and calcifications of the aortic root have been suggested to be predisposing conditions [3]. The incidence is higher in the setting of acute myocardial infarction [1]. Previous studies have indicated a higher risk of dissection at the ostium of the RCA, as this coronary artery has fewer smooth muscle cells and less dense matrix of type I collagen fibrils [4]. The entry point of the dissection can be caused by direct trauma from the catheter tip, forceful balloon inflation, dilation of calcified plaque, aggressive manipulations or contrast injections [3]. In our case probably manipulations with the guidewire led to damage of the RCA wall.
Management of iatrogenic aorto-coronary dissections depends on the patient’s hemodynamic status and the extent of aortic dissection. In some cases, dissection immediately proceeds to a life-threatening condition, including hemorrhage into the pericardium or occlusion of the coronary arteries with cariogenic shock, and high risk surgery is indicated. Dunning et al. proposed a classification of coronary dissection that extends towards the aorta to possibly guide strategies for treatment [1]. Class I is focal dissection restricted to the coronary cusp, class II involves the cusp and extends up the ascending aorta but less than 40 mm, and class III extends more than 40 mm. Class I and II should undergo conservative treatment (“wait and see” approach), whereas class III should be managed by surgical repair.
The initial goal of intervention should be to restore the patency of the coronary vessel. Immediate bailout stenting has been argued to be the best strategy for type I and II dissections [1, 5]. This maneuver will terminate progression of the dissection and the outcome for the aortic wall is more benign, with complete spontaneous healing over time [5]. Furthermore, in cases of severe dissection stenting does not interfere with chances of surgical repair. In fact, Nie et al. stated that surgery should only be considered when stenting failed to seal the dissection and the patient suffered from hemodynamic compromise [5].
The decision to decline surgical repair is a difficult one and should be taken by an experienced heart team. Recent studies and our case show that in a stable patient it is beneficial to proceed with bail-out stenting of the entry point of the dissection and continue with conservative management with diagnostic CT angiography even if more than 40 mm of the ascending aorta is involved (Dunning Class III).






