A 57-year-old female patient with a history of chronic obstructive pulmonary disease (COPD) and anxiety was referred to our clinic for evaluation of a pericardial cyst that had been incidentally diagnosed two decades prior. On radiographic imaging, the cyst had doubled in size from 2 to 4 cm. She stated that approximately 3–4 years ago she began having hypertension and shortness of breath with activity. She had been recently evaluated for carotid artery disease, which was found to be negative. She reported chest pain on the left side of her chest which could occur at any time. She also reported fatigue as well as progressive shortness of breath. She denied having lower extremity edema, orthopnea, paroxysmal nocturnal dyspnea, dizziness, or palpitations.
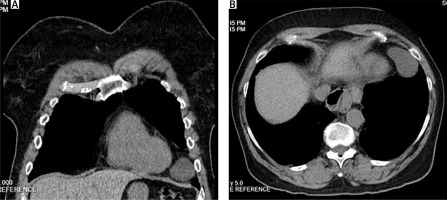
On imaging, computed tomography (CT) revealed a large pericardial cyst measuring 5 cm in diameter (Figure 1). The cyst was confined to the left cardiophrenic angle and was adjacent to the fifth rib along the inner chest wall. Transthoracic echocardiogram was normal with slightly elevated B-type natriuretic peptide.
Figure 1
Computed tomography of the pericardial cyst in the left cardiophrenic angle, coronal (A) and transverse (B) views
Operative planning was discussed with the patient. Sternotomy was advised due to proximity of the pericardial cyst to the left phrenic nerve.
On the day of the procedure, the patient was brought to the operating room and a median sternotomy was performed. The left pleural space was opened close to the sternum, as for a mammary artery takedown. The pericardial cyst was then visualized. It was localized at the left cardiophrenic angle, anterior to the phrenic nerve. There were numerous adhesions between the lung and the chest wall as well as between the lung and the mediastinal pleura. These were meticulously divided, staying close to the lung as to avoid injury to the phrenic nerve. The cyst was dissected away from the pericardium and pleura using a combination of blunt dissection and low-power electrocautery. The pericardium was not opened at any point. We stayed 1 cm anteromedial to the phrenic nerve, which was visualized at all times. The cyst was removed intact and sent for pathology (Figure 2).
The results of pathological examination revealed a thin-walled unilocular cyst filled with yellow-tinged fluid. Immunohistochemical staining was positive for calretinin and CK5/6, highlighting the mesothelial lining of the cyst wall. The morphology and immunophenotype were found to be compatible with a congenital mesothelial cyst.
The patient’s postoperative recovery was uneventful. She was discharged on the 10th postoperative day with plans for follow-up in the clinic. On follow-up, the patient denied recurrence of symptoms and no cyst was visualized on transesophageal echocardiography.
Congenital pericardial cysts are fluid-filled, unilocular sacs lined with mesothelial cells. They typically form due to incomplete fusion of the pericardial sac during embryonic development [1]. Acquired pericardial cysts may result from trauma or inflammation of the pericardial sac. Pericardial cysts occur in 1 in 100,000 patients and comprise 7% of all mediastinal masses [2]. They are most often found in the right cardiophrenic angle (70%) [1].
Approximately 25% of patients experience nonspecific symptoms such as chest pain, cough, dyspnea, and palpitations. These symptoms are sporadic, resulting from the compression of structures adjacent to the pericardium.
In general, when a pericardial cyst is detected, either computed tomography (CT) or Cardiac magnetic resonance (CMR) is recommended to confirm the diagnosis [3, 4]. Additionally, both offer better tissue characterization of the mass and detection of metastasis if malignancy is suspected [4].
Treatment recommendations for pericardial cysts are largely based on observational data [4]. Serial echocardiography every 1–2 years may be recommended to asymptomatic patients [5]. However, surgical resection is indicated in patients presenting with symptoms, large cysts, and/or radiologic features of compression or potential for malignancy [4, 5]. Video-assisted thoracic surgery is associated with less blood loss, minimal incision, better wound healing, and decreased length of stay [4]. Other approaches include mediastinoscopy, sternotomy, and thoracotomy. If conservative measures are desired, image-guided aspiration is also a possibility, with a 33% risk of recurrence [3].
In conclusion, it is desirable to perform surgical removal specific to the location of the pericardial cyst and schedule follow-up in 6 months with echocardiography.







