Introduction
As life expectancy increases, so aging-related diseases increases [1]. The distorted body image associated with pelvic organ prolapse (POP) can harm women’s quality of life (QoL) and their wellbeing [2].
The World Health Organization (WHO) defines QoL as “individuals’ perceptions of their position in life in relation to the culture and values in which they live, and in relation to their goals, expectations, standards, and concerns” [3]. It is a broad concept including the person’s physical and psychological status, level of independence, social relationships, and relationships with their environment [3].
POP can cause serious complaints because of hampered hygiene and limited mobility [2]. The most common symptoms of POP are a feeling of pressure or protrusion from the vagina, urinary incontinence (UI) or retention, voiding difficulties, and low backache. The symptoms associated with POP can cause significant disability affecting the QoL [4].
Various surgical procedures have been suggested for POP treatment, including colporrhaphy (with or without mesh placement), sacrospinous fixation (SSF), sacrocolpopexy, and colpocleisis. These surgical procedures differ in both success and complication rates. SSF is a technically challenging approach because the surgical site is deep and narrow. Although, several studies concluded that SSF is a safe and effective treatment in cases of uterine or vaginal vault prolapse [5, 6], it carries risk of complications including, haemorrhage, infection, and nerve damage.
Surgical treatment options of POP can be classified to either reconstructive or obliterative procedures. The reconstructive procedure, usually done after hysterectomy, can restore the vaginal depth and function, while the obliterative procedure is done as an effective alternative for correction of apical prolapse in old women who do not seek coital function [7].
An increasing number of old and healthy women are choosing the obliterative procedure due to its high success rate and quick recovery [8]. Le Fort colpocleisis (LFC) is the preferred obliterative surgical procedure for POP [9, 10]. Although LFC is an effective procedure for POP, its drawbacks include future evaluation of the cervix, vaginal discharge, and an uncomfortable feeling of fullness in the vagina [11].
Recent reports on LFC are mostly case series with poorly defined post-operative outcomes and follow-ups [12, 13]. There is only scarce literature about QoL after correction of POP in older women. This study was designed to evaluate the surgical outcome and QoL 12 months after LFC and SSF in older postmenopausal women.
Material and methods
This prospective comparative study was conducted from January 2015 to May 2019, after approval by the ethical committee of the Obstetrics and Gynaecology department.
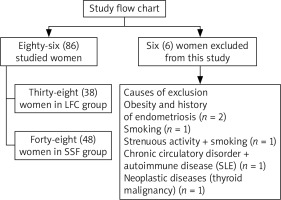
Eighty-six (86) post-menopausal women ≥ 65 years old with ≥ stage II vault prolapse were included in this study after informed consent in accordance with the Declaration of Helsinki.
Exclusion criteria included smoking, obesity (body mass index – BMI > 35), history of strenuous activity in the form of frequent heavy lifting > 50 kg as per job requirement [14], previous abdominal/pelvic surgery other than hysterectomy, and previous history of endometriosis and/or pelvic inflammatory disease.
Women with chronic circulatory disorders, autoimmune and/or neoplastic disease other than endometrial carcinoma, urinary incontinence, cognitive impairment, and unreliable women for post-operative follow-up were also excluded from this study. Six (6) women were excluded at the beginning of this study, and the causes of exclusion are summarized in the study flow-chart (Fig. 1).
Participants were subjected to thorough history to record their age, BMI, parity, medical co-morbidities (diabetes mellitus, thyroid disorders, cardiovascular, liver, renal diseases), neurological diseases (stroke, cerebrovascular attacks), neuropsychiatric disorders, and non-gynaecological malignancies.
Participants underwent standard physical examination and evaluation of their prolapse using the POP quantification (POP-Q) suggested by the International Continence Society (ICS), American Urogynecologic Society (AUGS), and Society of Gynecologic Surgeons [8]. The POP-Q was used for the objective measurement of POP according to 6 distinct locations (Aa, Ba, C, D, Ap, Bp) and 3 anatomical markers (gh, pb, tvl) [8].
Participants were examined in a supine position, and the maximum prolapse was evaluated by asking participants to cough or to perform a Valsalva manoeuvre. POP was evaluated using POP-Q, and the stage of POP in relation to hymen was recorded.
Stage 0: No prolapse is observed (all Aa, Ba, C, D, Ap, and Bp points are ≤ –3 cm).
Stage 1: The prolapse is > 1 cm above the hymen (all Aa, Ba, C, D, Ap, and Bp points are < –1 cm).
Stage 2: The prolapse is 1 cm above or below the hymen (points Aa, Ba, C, D, Ap, and Bp points are –1 or + 1 cm).
Stage 3: The prolapse > 1 cm below the hymen but < 2 cm of tvl (points Aa, Ba, C, D, Ap, and Bp are ≥ + 2 cm and < tvl – 3 cm).
Stage 4: Vaginal eversion with 2 cm of tvl (Aa, Ba, C, D, Ap, and Bp points are ≥ tvl –2 cm).
Eligible women were assigned to either the LFC group or the SSF group, after giving informed written consent (based on their choice after counselling). Surgeries were performed by an experienced gynaecologist (≥ 12 years’ experience after MD degree and ≥ 80 LFC and SSF procedures).
LFC procedure: Rectangular shapes on the anterior and posterior vaginal walls were demarcated with sterile marker; then, the anterior and posterior vaginal epithelial tissue were stripped with sharp dissection and the edges of each distal quadrangle were sutured together. The denuded areas were sutured together front-to-back in progressive rows using (Vicryl 2–0, Ethicon, NJ, USA) interrupted sutures. The prolapsed parts were inserted into the vaginal cavity, leaving lateral tunnel on each side followed by levator ani plication and posterior perineorrhaphy.
SSF procedure: SSF procedures were performed unilaterally to the right sacrospinous ligament. The rectovaginal space was dissected to separate it from the rectum following posterior vaginal wall incision. The pararectal space was entered to access the sacrospinous ligament (SSL). The SSL was made visible via blunt dissection following palpation of the ischial spine. One permanent suture (Prolene 1.0, Ethicon, NJ, USA) and one delayed absorbable suture (Vicryl 1.0, Ethicon, NJ, USA) were placed through the right SSL (at least 2 cm from the ischial spine) to the vaginal apex. The sacrospinous sutures were tied to elevate the vaginal apex towards the SSL after closure of the upper 2/3 of the posterior vaginal wall incision with absorbable (Vicryl 2) sutures. Then the lower 1/3 of the posterior vaginal wall incision was sutured, followed by anterior and/or posterior colporrhaphies.
The Arabic version of the WHOQoL-BREF Inventory [15] was used to evaluate the participants’ QoL preoperatively and post-operatively. The total WHOQoL score based on 26-items (minimum score 26, while maximum score 130 – higher scores indicating better QoL). The WHOQoL includes 4 domains (physical, psychological, social, and environment health domains) in addition to general quality of life and general health satisfaction [15, 16]. Because of reading and visual difficulties among the elderly studied women, their QoL was assessed during direct interview by 2 investigators who were blinded to the pre-operative stage of POP and the surgical procedures done (to avoid potential bias affecting the study results).
Post-operative (PO) follow-up of the participants was done at 6 weeks and 3, 6, and 12 months PO. The surgical outcome and QoL 12 months after LFC and SSF were analysed to evaluate the surgical outcome (primary outcome), and QoL (secondary outcome) 12 months after LFC and SSF.
Statistical analysis
Statistical analysis was done using STATA version 14 (software for statistics and data science, STATA Corp., Texas, USA). Numerical variables were presented as mean and standard deviation (± SD), while categorical variables were presented as number (n) and percentage (%). The χ2 test was used to compare qualitative variables, and Student’s t-test was used to compare numerical variables. Primary outcome measures, the surgical outcome 12 months after LFC and SSF, while the secondary outcome measures, the QoL 12-months after LFC and SSF. P-value < 0.05 was considered significant.
Results
Eighty-six (86) post-menopausal women were included in this study (38 in the LFC group and 48 in the SSF group) after approval of the study and informed consent in accordance with the Declaration of Helsinki.
There was no significant difference between the 2 studied groups regarding mean age, parity, BMI, indications of hysterectomy [17–19], medical comorbidities, and per-operative prolapse stage (Table 1).
Table 1
Characteristics of the studied groups, operative time, estimated blood loss, post-operative complications, and hospital stay
[i] AUB – abnormal uterine bleeding, BMI – body mass index, CI – confidence interval, χ2-test – used for statistical analysis when data presented as number and percentage (%), COPD – chronic obstructive pulmonary disease. Data presented as mean ± standard deviation (SD) and number and percentage (%), EBL – estimated blood loss. Student’s t-test used for statistical analysis when the data presented as mean ± SD
The surgical procedures, either LFS or SSF, were done under general anaesthesia in 6.98% (6/86), and under epidural anaesthesia in 93.02% (80/86) of the studied cases. There was no significant difference between the 2 studied groups regarding the operative time (59.5 ± 11.2 min in the LFC group vs. 65 ± 16.2 min in the SSF group (p = 0.9 [95% CI: –11.4, –5.5, 0.4]), intra-operative estimated blood loss (EBL) (442.5 ± 45.8 mL in the LFC group vs. 539 ± 68.7 mL in the SSF group (p = 0.9 [95% CI: 121.2, –96.5, –71.8]), and post-operative hospital stay (2.8 ± 1.7 days in the LFC group vs. 3.2 ± 2.9 days in the SSF group (p = 0.9 [95% CI: –1.4, –0.4, 0.61]). One woman (1/48 [2.08%]) in the SSF group had intra-operative bleeding due to injury of the inferior gluteal vein, controlled by compression. Two women (2/48 [4.16%]) in the SSF group had PO urinary retention managed by Foley`s catheter insertion and bladder training. No intra-operative or PO complications were recorded in the LFC group. There was no significant difference between the 2 studied groups regarding the intra-operative (p = 0.2) or PO complications (p = 0.1) (Table 1).
There was no significant difference between the 2 studied group regarding the pre-operative Aa, Ba, C, D, Ap, Bp, gh, pb, and tvl values of the POP-Q. The pre-operative Aa, Ba, D, Ap, and Bp values of the POP-Q significantly improved 12 months PO in the LFC group (p1 = 0.004, 0.0006, 0.02, 0.004, and 0.0001, respectively) and in the SSF group (p1 = 0.003, 0.0003, 0.003, 0.0005, and 0.01, respectively). In addition, there was no significant difference between the 2 studied groups regarding the 12-month PO Aa, Ba, C, D, Ap, Bp, gh, pb, and tvl values of the POP-Q (Table 2).
Table 2
Preoperative and 12-month post-operative pelvic organ prolapse quantification in the two studied groups
* – significant difference, CI – confidence interval. Data presented as mean ± standard deviation (SD), p1 value used when the pre-operative and postoperative variables compared within the same group, p2 value used when the pre-operative or postoperative variables compared between the two studied groups, Student’s t-test – used for statistical analysis, POP-Q –pelvic organ prolapse quantification, Aa – refers to midline of anterior vaginal wall, 3 cm up from the hymen when there is no prolapse, Ba – refers to anterior vaginal wall mid-way between Aa and anterior fornix when there is no prolapse, C – cervix (lowest edge or vaginal cuff following hysterectomy), D – Douglas pouch, Ap – refers to the midline of posterior vaginal wall 3 cm proximal to hymen, Bp – refers to posterior vaginal wall mid-way between Ap and posterior fornix when there is no prolapse, gh – genital hiatus, refers to the length from the urethral opening to the posterior vaginal opening, pb – perineal body, refers to length from the posterior aspect of hymen to the mid-anal opening, tvl – total vaginal length, measured from hymen to the most distal point to assess of the depth of prolapse before, and after surgical correction
Eighty (93.02%) of the studied women had no prolapse at 12-month PO follow-up, while 6 (6.98%) of them had asymptomatic stage I prolapse (3 after SSF and 3 after LFC), and none of them required additional surgery.
There was no significant difference between the two studied groups regarding the pre-operative physical, psychological, social, and environmental health domains, general QoL, general health satisfaction, and total QoL score (Table 3).
Table 3
Preoperative and 12-month post-operative quality of life in the two studied groups
* – significant difference, CI – confidence interval. Data presented as mean ± standard deviation (SD), p1-value used when the pre-operative and postoperative variables compared within the same group, p2-value used when the pre-operative or postoperative variables are compared between the two studied groups, QoL – quality of life. Student’s t-test used for statistical analysis
The pre-operative physical, psychological, and social health domains of the WHOQoL score significantly improved 12 months PO in LFC group (p1 = 0.04, 0.02, and 0.02, respectively) and in the SSF group (p1 = 0.02, 0.0002, and 0.0001, respectively). In addition, the preoperative general health satisfaction and total QoL score significantly improved 12 months PO in the LFC group (p1 = 0.04 and 0.01, respectively) and in the SSF group (p1 = 0.003 and 0.0001, respectively) (Table 3).
The 12-month PO psychological and social health domains were significantly higher in the SSF group compared to the LFC group (p2 = 0.04 [95% CI: –8.8, –4.1, 0.6], and 0.02 [95% CI: –5.6, –1.2, 3.2], respectively). In addition, the 12-month PO general health satisfaction and total QoL scores were significantly higher in the SSF group compared to the LFC group (p2 = 0.03 [95% CI: –1.8, –0.2, 1.4], and 0.01 [95% CI: –9.7, –3.7, 2.3], respectively) (Table 3).
Discussion
POP is a major concern among older women. A small number of women who suffer from POP will be operated; most of them just receive conservative treatment and never present to physician [11, 12].
POP symptoms can cause significant disability, affecting the QoL [4]. LFC is the least invasive and most durable surgical procedure available for the treatment of POP in older women [20].
Therefore, 86 post-menopausal women were included in this study (38 in the LFC group and 48 in the SSF group) to evaluate the surgical outcome and QoL 12 months after LFC and SSF in older postmenopausal women.
There was no significant difference between the 2 studied groups regarding mean age, parity, BMI, indications of hysterectomy, medical comorbidities, and per-operative prolapse stage. In addition, there was no significant difference between the 2 studied groups regarding the operative time (p = 0.9) and intra-operative EBL (p = 0.9). Medical co-morbidities were recorded in 34/38 (89.47%) women of the LFC group and in 42/48 (87.5%) women of the SSF group.
Ng et al. reported at least one medical comorbidity in 20/22 (90.9%), and > 2 comorbidities in 13/22 (59.1%) women > 70 years old with POP [21]. Ghezzi et al. found that 95.7% had > 1 comorbidity, and only 4.3% had 1 medical comorbidity during treatment of pelvic floor dysfunction in advanced-age women [22].
In general, medical disorders and comorbidities increase with age. Age alone should not be the main reason for rejecting any surgical procedure in an older woman. Furthermore, it is important to take the QoL into consideration. The decision to perform surgery should be extensively discussed with the patient and her relatives [23].
In the SSF studied group, 1 woman (1/48 [2.08%]) had intra-operative bleeding due to injury of the inferior gluteal vein (controlled by compression), and two women (2/48 [4.16%]) had PO urinary retention (managed by Foley's catheter insertion and bladder training). No intra-operative or PO complications were recorded in the studied LFC group.
Sung et al. reported that women with extreme old age who underwent obliterative procedures had a lower risk of complication than those who underwent reconstructive procedures for POP (17 vs. 24.7%, p < 0.01) [24]. Krissi et al. reported no intra-operative complications and 2 lower tract infections among women > 80 years old who underwent LFC, with a subjective cure rate of 86.7% (20/23) [25].
Leijonhufvud et al. concluded that LFC is the least invasive and most durable surgical procedure available for treatment of POP in older women [20].
The pre-operative Aa, Ba, D, Ap, and Bp values of POP-Q significantly improved 12 months PO in the 2 studied groups. Eighty (93.02%) of the studied women had no prolapse at 12-month PO follow-up, while 6 (6.98%) of them had asymptomatic stage I prolapse (none of them required surgery).
The largest colpocleisis study, by Zebede et al., reported an anatomical success rate of 98.1% after colpocleisis [26].
De-novo urinary incontinence may develop after POP surgery, which is referred to as occult stress urinary incontinence [27, 28]. The bladder nerve damage during LFC are usually minimal, and most urinary symptoms after LFC are transient and self-resolving [28]. In addition, anti-incontinence surgery at the time of POP surgery is under debate [29].
Von Pechmann et al. reported 2 cases of rectal prolapse (2.2%) in 92 women who underwent total colpocleisis [30]. They suggested that the plication of the levator ani during colpocleisis and correction of the anterior pelvic floor weakness may result in posterior pelvic floor weakness and subsequent anorectal prolapse with increased intrabdominal pressure [30].
In this study, the pre-operative physical, psychological, and social health domains, general health satisfaction, and total QoL score were significantly improved PO in the 2 studied groups. In addition, the psychological and social health domains, general health satisfaction, and total QoL scores were significantly higher in the SSF group compared to the LFC group 12 months PO (p2 = 0.04, 0.02; 0.03, and 0.01, respectively).
Zebede et al. reported a 92.9% subjective satisfaction rate after colpocleisis [26]. Ng et al. reported a 93.8% satisfaction rate in women > 70 years old with POP treated with obliterative LFC [21]. Song et al. reported a 94.3% satisfaction rate 5 years after LFC, and only 2 women were “neither satisfied nor dissatisfied” [31].
This study concluded that LFC can be considered a good surgical procedure with minimal or neglectable complications for POP in older women with multiple co-morbidities who do not seek coital function. Although the QoL significantly improved after both LFC and SSF, the psychological and social health domains, general health satisfaction, and total QoL scores were significantly higher in the SSF group compared to the LFC group 12 months PO.
Women refusing to give consent and/or participate, women with difficult communication, and being a single-centre study were the limitations of this study.
There is only scarce literature about QoL after surgical correction of POP in older women. This is the first study designed to evaluate the surgical outcome and QoL 12 months PO after LFC and SSF in older postmenopausal women using the Arabic version of the WHOQoL-BREF Inventory. Further future comparative studies using the WHOQoL-BREF Inventory are needed to confirm our findings.
Conclusions
Age alone should not be the main reason for rejecting any surgical procedure in an older woman, and it is important to take the QoL into consideration. LFC can be considered a good surgical procedure with minimal or neglectable complications for POP in older postmenopausal women with multiple co-morbidities who do not seek coital function. Although the QoL significantly improved in both LFC and SSF groups, the psychological and social health domains, general health satisfaction, and total QoL score were significantly higher in the SSF group compared to the LFC group 12 months PO.