The sinus of Valsalva aneurysm (SVA) is a rare congenital (muscular or elastic deficiency) or acquired (trauma, infection, atherosclerosis) pathological condition. The most common is isolated right sinus aneurism with an incidence of 94%; the non-coronary sinus is affected in 5% of cases, and rarest is an aneurysm of the left coronary sinus, about 1% [1]. Indications for treatment of unruptured SVA are aneurysm dimensions, rapidly increasing in size, prevention of complications (rupture or thrombus formation), symptoms and clinical presentation [2]. The literature describes different surgical strategies for the treatment of this pathology.
We performed surgical reconstruction of giant non-coronary sinus of Valsalva aneurysm using the valve-sparing procedure (David procedure).
The 55-year-old woman was admitted to the hospital due to palpitation, dyspnea and fatigue. The patient has no history of cardiovascular diseases. Transthoracic echocardiography examination revealed a huge aneurysm (45 × 40 mm) of the non-coronary sinus of Valsalva. An aneurysm sac compressed the right atrium and superior vena cava. The right-side filling pressure was elevated. The superior vena cava was dilated 28 mm, with an increased diastolic flow gradient of 9/5 mm Hg. The ascending aorta was 45 mm with moderate aortic valve regurgitation. The ejection fraction and dimensions of the heart were in the reference range. An additional computed tomography scan revealed a saccular aneurysm 45 × 40 mm of the non-coronary sinus of Valsalva and a smaller aneurysm of the right coronary sinus (Figures 1 A–C).
Figure 1
Computed tomography scan showed a huge non-coronary sinus Valsalva aneurysm. A, B – Volume rendering reconstruction. C – Contrast scan
Asterisk – aneurism of non-coronary sinus of Valsalva, Ao – ascending aorta, LV – left ventricle, RA – right atrium.

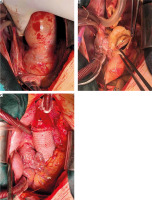
The surgical procedure was performed through median sternotomy. A giant aneurysm of the non-coronary sinus of Valsalva was detected. The right atrium was significantly compressed by an aneurysm sac (Figure 2 A). Cardiopulmonary bypass was established by ascending aorta and bicaval venous cannulation. Incision of the ascending aorta near the sinotubular junction was performed, and the aneurysm cavity and aortic valve were inspected (Figure 2 B). Due to the normal morphology of all three valve leaflets, we decided to perform the valve-sparing aortic root replacement procedure (David procedure). The preparation of the non-coronary sinus from the right atrium was challenging due to the frailty of the atrium tissue, and the damaged atrial wall was reconstructed with an autologous pericardial patch. Resection of the aneurysm and right and left coronary sinuses was performed, and preparation of the subannular plane was made. Coronary buttons were created, and an aortic valve was re-implanted into the Valsalva graft 28 mm (Figure 2 C) by the standard technique. Intraoperative transoesophageal echocardiography shows good coaptation of the aortic valve cusps without aortic regurgitation.
Figure 2
A – Surgical view on the ascending aorta and huge SVA. B – Surgical view on the resected Ao and SVA. C – Reconstructed aortic root and ascending aorta by David procedure
Ao – ascending aorta, RA – right atrium, RV – right ventricle, SVA – sinus Valsalva aneurysm, LCC – left coronary cusp.
The postoperative period was uneventful, and the patient was discharged from the hospital on the seventh postoperative day.
The incidence of SVA according to autopsy results is 0.09%. Males are four times more frequently affected than females. For patients with an aneurysm larger than 5 cm, with a growth rate of more than 5 mm per year, symptomatology and rupture are indications for surgical treatment [3]. Different surgical techniques are described in the literature. Direct closure has been used for a small aneurysm, while patch or isolated sinus repair is preferred in larger defects of the aortic wall to prevent suture line tension and disruption. Endovascular intervention was successful performed for an aneurysm smaller than 8 mm [4]. Mentioned techniques are not definitive solutions because the weakness of the aortic wall could be the main reason for postprocedural dilatation of the aortic root. Postoperative dilatation and rupture of the untreated parts of Valsalva sinuses are described and required urgent surgical treatment. Redo surgery in these cases was demanding, with higher risk [5]. This is the main reason why we decided to perform complete reconstruction of Valsalva sinuses and prevent late adverse events and reoperations. We think that aortic root replacement can be the method of choice for this pathological entity.
Surgical intervention is a gold standard for the treatment of sinus Valsalva aneurysm. Propensity to dilatation of unreconstructed parts of the aortic root required complete aortic root surgery. The valve-sparing aortic root replacement procedure (David procedure) is an excellent choice for these patients.






