Primary cardiac tumors are rare, with benign myxomas representing the most frequently encountered subtype, predominantly localized in the left atrium [1]. Right atrial myxomas are comparatively uncommon, accounting for only 10–20% of all cardiac myxomas [2]. While these tumors may cause significant symptoms due to obstruction of blood flow through the tricuspid valve or embolic phenomena [3], certain patients, as highlighted in this case, may present with only mild clinical manifestations [4]. Early diagnosis and timely surgical intervention are critical to mitigate the risk of life-threatening complications [5]. This report describes the successful surgical management of a giant right atrial tumor, emphasizing the importance of prompt detection, even in minimally symptomatic individuals.
A 67-year-old male patient presented with mild, progressive exercise intolerance that had developed over the past year. The patient had no history of chronic illness, was not on any medications, and reported a long-standing history of smoking. He initially postponed seeking medical care, attributing his symptoms to lifestyle factors. After 8 months, he consulted a cardiology clinic, where transthoracic echocardiography revealed a large right atrial mass. Further evaluation at the cardiology unit confirmed the presence of a 6 × 5.5 cm pedunculated tumor attached to the interatrial septum, occupying nearly the entire right atrium and intermittently obstructing the tricuspid valve. Coronary angiography excluded significant coronary artery disease. The patient was subsequently referred to the cardiac surgery department for tumor resection.
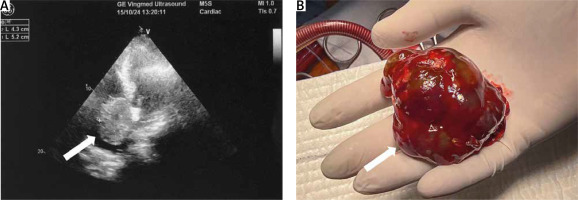
Under general anesthesia, a median sternotomy was performed, and cardiopulmonary bypass was initiated. Intraoperative findings revealed a tumor attached to the foramen ovale via a stalk. Complete excision of the tumor, along with a portion of the interatrial septum to ensure clear margins, was achieved (Figure 1). The resultant septal defect was closed with a patch, and the patient was successfully weaned from cardiopulmonary bypass without complications.
Figure 1
Echocardiographic images showing a right atrial tumor attached to the interatrial septum near the foramen ovale (A) and the fully excised myxoma with an intact stalk (B)
Histopathological examination confirmed the tumor’s benign nature. The postoperative course was uneventful, and the patient was discharged in stable condition to a cardiac rehabilitation center for further recovery.
This case underscores the atypical presentation of a giant right atrial tumor with minimal symptoms, which is unusual given the tumor’s substantial size and its potential to obstruct blood flow [6]. Myxomas predominantly arise in the left atrium, with right atrial myxomas being less commonly reported. These tumors are more likely to manifest with symptoms due to tricuspid valve obstruction or risks of pulmonary embolism [7]. In this patient, the pedunculated attachment of the tumor likely contributed to its intermittent obstruction of the tricuspid valve, resulting in only mild clinical manifestations [8].
Echocardiography remains the cornerstone diagnostic modality for evaluating cardiac masses, offering critical insights into tumor attachment, size, and mobility, which are integral to surgical planning [9]. Cardiopulmonary bypass plays an essential role in such cases by mitigating the risk of tumor embolization during resection. Current literature supports complete excision of the tumor, including its stalk, to minimize the risk of recurrence, consistent with best practices for managing cardiac myxomas [10].
Histologically, cardiac myxomas are benign but carry significant clinical implications due to their potential for embolic events or obstructive symptoms. While recurrence is rare, factors such as incomplete resection or genetic predisposition can contribute to recurrence [2]. Radical excision with clear surgical margins, as achieved in this case, is critical to reducing recurrence risk. Postoperative outcomes following complete excision are typically favorable, particularly when supported by structured rehabilitation programs aimed at enhancing recovery and functional capacity [5].
This case of a giant right atrial myxoma emphasizes the need for vigilance, even in patients with mild and nonspecific symptoms. As noted by Greberski et al. [11], delayed recognition of complications in cardiovascular surgery, even years after the initial intervention, can lead to life-threatening events. Similarly, our case highlights the importance of timely intervention to avert potentially fatal outcomes associated with obstructive cardiac tumors.
The challenges of perioperative management in cardiac surgery are well documented. For instance, Elikowski et al. [12] reported takotsubo syndrome as a rare yet significant complication following combined mitral valve replacement and coronary artery bypass grafting. In this patient, meticulous echocardiographic evaluation and precise surgical execution ensured complete tumor resection without perioperative complications, reinforcing the critical role of detailed preoperative planning in avoiding adverse outcomes.
Finally, the long-term success of cardiac surgical procedures relies heavily on surgical expertise and comprehensive follow-up programs. As demonstrated by Burysz et al. [13], even in medium-volume centers, complex cardiovascular procedures, such as thoracic endovascular aortic repairs, yield favorable outcomes when performed by specialized teams. These findings align with the importance of expert management in cases of cardiac myxomas, ensuring optimal patient recovery and minimizing the risk of recurrence.
This case highlights the critical importance of including cardiac tumors in the differential diagnosis of patients presenting with even mild and nonspecific symptoms. Echocardiographic evaluation and timely surgical resection were pivotal in achieving a successful outcome for this patient with a giant right atrial tumor. Early diagnosis and comprehensive surgical management remain essential in preventing potentially life-threatening complications associated with intracardiac masses.






