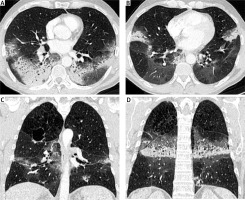
A 56-year-old man with stage IV non-small cell lung cancer (NSCLC) presented to the emergency department with progressive dyspnea and hypoxia. He had been diagnosed with adenocarcinoma of the right upper lobe 16 months earlier. PD-L1 expression in the tumor was 2%, and no other gene driver mutations were detected. The patient initially received treatment with a combination of platinum-based chemotherapy and immunotherapy (pembrolizumab). After the initial partial response to treatment, the patient remained in consolidation therapy treated only with pembrolizumab (Keytruda) for the last 12 months. At the time of the investigation of the progressive dyspnea, a chest radiograph and a computed tomography (CT) scan were performed. The chest radiograph showed bilateral airspace opacities consistent with either pneumonia or pneumonitis (Figure 1). The CT scan showed symmetrical bronchocentric consolidation with distribution suggestive of organizing pneumonia induced by pembrolizumab treatment (Figure 2). Bronchoalveolar lavage (BAL) was performed confirming the radiological diagnosis and excluding infection. The patient was treated with steroid therapy with clinical improvement and resolution of the symmetrical consolidation. Pembrolizumab (Keytruda) is a programmed cell death protein 1 inhibitor that is used as frontline treatment for NSCLC, with significant improvement of the survival rate [1]. Despite pembrolizumab’s clinical benefits, some patients develop associated immune-related adverse events (IRAE) including pneumonitis [2]. Immunotherapy-associated pneumonitis is a rare (3–6%) [3, 4] but severe complication characterized by focal or diffuse parenchymal inflammation. The time of onset of pneumonitis after administration of immunotherapy is variable [5]. Symptoms are often nonspecific, including dyspnea, cough, malaise and low-grade fever, requiring a high index of suspicion, whilst some patients may be asymptomatic [4]. As a result, diagnosis of immunotherapy-induced pneumonitis is usually achieved by excluding other potential causes. Clinically it is graded using the Common Terminology Criteria for Adverse Events (CTCAE) severity scale, which ranges from grade 1, asymptomatic, through to grade 5, where death occurs [6]. Diagnosis is based on appropriate history and suggestive radiological findings on CT scanning. The most common radiological features include ground glass opacities, interstitial reticulation, or bronchocentric consolidation suggestive of patterns of organizing pneumonia (OP), non-specific interstitial pneumonia (NSIP), diffuse alveolar damage (DAD) or hypersensitivity pneumonitis (HP) and reflecting the histological patterns of interstitial pneumonia [7–9]. Definitive diagnosis may require a combination of BAL and/or a biopsy. Treatment options include supportive therapy alone, oral or intravenous corticosteroids and cessation of immunotherapy [9].