Introduction
Tetralogy of Fallot (TOF) corrective surgery, especially using a transannular patch, carries a high risk of reintervention [1]. Surgical pulmonary valve replacement with a bioprosthetic valve (BPV) is a well-established method of treating postoperative right outflow tract dysfunction [2]. Since BPV function deteriorates and patient-prosthesis mismatch increases with growth, reintervention is necessary. To avoid the reoperation risk, valve-in-valve (ViV) transcatheter pulmonary valve replacement (TPVR) has become an attractive alternative [3]. The BPV true inner diameter (ID) is shorter than the nominal BPV size by 2 mm or more, which limits the ViV therapy [4]. The valve implanted within the BPV makes the effective lumen even narrower. Since the first report by Tanase et al. [5], intentional fracture of the BPV frame using ultra-high-pressure balloons has become a valuable option to optimize the hemodynamic outcomes of ViV in the BPV in a pulmonic position [6].
Case report
The case concerns a 17-year-old, 69 kg, asymptomatic boy after a TOF complete repair with a transannular patch. The patient was re-operated at the age of 10 with a stentless valve and only 1 year later with a 23 mm Carpentier-Edwards Perimount Magna bioprosthetic valve (Edwards Lifesciences Inc., Irvine, USA). Pulmonary stenosis (PS) with maximum/mean gradient of 100/55 mm Hg, moderate pulmonary regurgitation, and dilated right ventricle were established during transthoracic echocardiography. Computed tomography (CT) revealed a 12 mm supravalvular PS and proximal narrowing of pulmonary arteries: right (RPA) to 9 and left (LPA) to 6 mm (Figure 1 A).
Figure 1
A – Computed tomography of a 17-year-old tetralogy of Fallot patient after bioprosthetic Edwards Magna valve (BPV) surgical replacement. Supravalvular pulmonary (PS) and bifurcation stenosis. B – Three-dimensional computed tomography-derived silicone model of the right ventricle outflow tract with supravalvular (PS) and bifurcation stenosis: 48 mm AndraStent XXL implanted into PS and LPA and through this stent’s cells a 21 mm AndraStent XXL was implanted in the RPA. C – 48 mm AndraStent XXL implanted into both PS and LPA and 21 mm AndraStent XXL implanted into RPA. Lower frame of 23 mm Magna valve cracked at 18 atm with 24 mm Atlas balloon, arrow – frame separation. D – 23 mm Edwards Sapien XT valve implanted in the upper part of a 23 mm Magna valve
RPA – right pulmonary artery, LPA – left pulmonary artery.
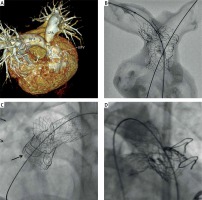
In order to test transcatheter treatment options, a 3D CT-derived silicone model of the aforementioned region with an embedded valve was prepared. Subsequently, the Y-stenting technique for bifurcation stenosis was selected. This includes implantation of a long hybrid-cell designed stent into the supravalvular PS and LPA and another stent into the RPA through the struts of the first stent (Figure 1 B). Moreover, an experimental bench test with cracking of the 23 mm Magna BPV using a 24 mm Atlas balloon (Bard Peripheral Vascular Inc., Tempe, USA) was performed. The lower restrictive frame of the valve cracked at 14 atm. A preprocedural CT scan excluded risk of coronary artery compression in the intended valve landing zone. Finally, the patient was qualified for ViV TPVR and informed consent was obtained.
A PS gradient of 51 mm Hg, right-to-left ventricle pressure ratio (RV/LV) of 0.73, and a BPV ID of 19 mm were confirmed by catheterization. A 48 mm AndraStent XXL (AndraMed GmbH, Reutlingen, Germany) was implanted into the LPA, pulmonary trunk, and Magna valve on a 22 mm BIB balloon (NuMED Inc., NY, USA). The supravalvular diameter increased to 18.3 and the LPA origin increased to 16 mm. The next step was postponed for a month to enable partial stent ingrowth. After pre-dilatation with a 12 mm Atlas Gold balloon, a 21 mm AndraStent XXL on a 16 mm MaxiLD (Cordis, Florida, USA) balloon was implanted into the RPA through a semi-opened first stent scaffold. The RPA expanded to 11.4 mm. Magna valve fracture was performed 3 months later with a 24 mm Atlas balloon. The lower BPV frame cracked at 18 atm and ID increased to 22 mm (Figure 1 C). A 23 mm Edwards Sapien XT valve was subsequently implanted slightly above the Magna valve (balloon overfilled with 3 ml) (Figure 1 D). The XT valve overdilation allowed the BPV ID to be expanded to 24, the XT valve ID to 22, and supravalvular stenosis to 21 mm. The residual gradient decreased to 30 mm Hg with an RV/LV ratio of 0.39 and persisted at the supravalvular stenosis (top of the XT valve). There were no procedure-related complications during any stage. Life-long aspirin, 6 months of clopidogrel, and continuous infective endocarditis prophylaxis were administered. In a 10-month follow-up, the patient is asymptomatic with a mean PS gradient < 25 mm Hg and no PR in routine control echocardiography.
Discussion
BPV has a four-component structure: tissue valve, supporting frame, sewing ring, and polymer cloth covering. ViV tactics in BPVs cause an unacceptable limitation of the eventual lumen. Furthermore, a high residual gradient after TPVR brings a greater risk for valve failure, death [7], and infective endocarditis [8].
Depending on the frame material, BPVs can be either fractured or stretched. The ultra-high-pressure Kevlar balloons are non-compliant and resistant to overdilation with a nominal burst pressure of 18 atm; however, successful inflation up to 26 atm was reported [6]. According to the literature, the balloon should be minimally 1–2 mm larger than the true ID of the BPV [6]. BPV fracture proved to be safe in both in vitro and in vivo studies due to the surrounding Dacron sewing ring, which prevents vessel damage [5, 6, 9].
The complex bifurcation anatomy in our patient forced the non-standard procedure. A Y-stenting technique was selected in order to dilate the PS and pulmonary arteries. The long hybrid-cell stent was implanted into the PS and the LPA to enable efficient RPA dilation. However, staged rehabilitation of the obstructed right ventricle-to-pulmonary artery conduit with implantation of a stent on two balloons has also been described [10]. As cracking was performed with a 24 mm balloon, selection of a 23 mm Edwards XT valve seemed to be safe. The XT valve was implanted just below the bifurcation to dilate the narrowest part of the stent at a safe distance from coronary arteries. On the basis of the distance between coronary arteries and the pulmonic valve landing zone, the compression test was abandoned. The whole procedure was divided into stages to ensure proper stent stabilisation and to prevent displacement during the cracking of the BPV. In summary, supravalvular PS and bifurcation were significantly dilated and the gradient decreased to 30 mm Hg.
The Y-stenting technique for bifurcation stenosis and intentional fracture of the BPV frame with ultra-high-pressure balloon prior to ViV TPVR is possible in selected patients in order to prevent a hazardous reoperation.








