Summary
The most effective therapy for ST-segment elevation myocardial infarction (STEMI) is immediate primary percutaneous coronary intervention. It is known that one of the most important factors affecting mortality in STEMI patients is the door-to-balloon time. In our study, we divided the door-to-balloon time into two and investigated the effect of emergency department delay time on mortality. We observed that loss of time in the emergency department may have significant effects on mortality.
Introduction
An unstable plaque within the coronary artery thrombus, which results in acute myocardial ischemia and necrosis, is the main trigger of ST segment elevation myocardial infarction (STEMI). Persistent chest pain, dyspnea, and sweating cold are the most common clinical symptoms [1]. Since the development of healthcare systems, the early clinical mortality rate of STEMI has decreased significantly from 13% to 4%, mainly due to early opening of the culprit artery [2]. Therefore, the most effective therapy for STEMI is immediate primary percutaneous coronary intervention (pPCI). Myocardial perfusion and blood supply can be restored after the recanalization of the infarct-related artery (IRA) [3]. Any delays from onset of symptoms to recanalization of IRA are associated with increased microvascular obstruction (MVO), infarct size (IS), and mortality [4]. Treatment recommendations from several randomized controlled studies highlight the significance of resuming blood flow to the infarct-related artery in STEMI patients as soon as feasible [5].
Reducing door-to-balloon time (DTB) has attracted the most research attention among recent STEMI treatment strategies. European and US guidelines for clinical practice advocate providing the patient with DTB time within 60 min of STEMI diagnosis. The effects of all time intervals, especially DTB and total ischemic time [6], for patients diagnosed with STEMI have been investigated in many studies. Total ischemia time (TIT) and DTB time are associated with mortality and worse cardiac outcomes [6–8].
However, the impact of emergency department delay time (EDDT) (time from arrival at a PCI-capable center to sheath insertion) on all-cause mortality and adverse cardiac events in STEMI patients remains unclear.
Aim
The primary aim of this study was to test the hypothesis that EDDT reduces in-hospital and 1-year mortality in STEMI patients undergoing pPCI, and the secondary aim was to investigate the effect of EDDT on treatment outcomes.
Material and methods
Study populations
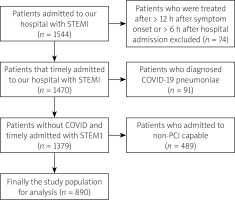
This was a retrospective analysis of 890 consecutive STEMI patients who had previously undergone pPCI at the Health Sciences University of Gazi Yaşargil Training and Research between October 2016 and May 2021. Of the 1544 patients diagnosed with STEMI and who underwent pPCI, 74 were treated more than 12 h after the onset of symptoms or more than 6 h after hospitalization. Ninety-one patients were diagnosed with COVID-19 pneumonia, while data could not be accessed for 89 patients. 400 patients who applied to centers where PCI could not be performed were excluded from the study. Finally, patients with “nonsystemic delays”, such as patients with suspected aortic dissection who required CT angiography before going to the catheter laboratory, were excluded. Finally, 890 patients diagnosed with STEMI were included in the current analysis. Figure 1 displays the patient flow chart according to the inclusion and exclusion criteria. The patients were divided into two groups: survivors and non-survivors. The survivor group consisted of 805 patients and the non-survivor group consisted of 85 patients.
Definitions
STEMI patients were diagnosed based on the recommendations of the ESC guidelines [9].
Diabetes mellitus (DM): 126 mg/dl (7.0 mmol/l) or higher fasting blood sugar; an glycated hemoglobin (HbA1c) of greater than 7; or use of antidiabetic drugs.
Hypertension (HT): Arterial blood pressure of more than 140 mm Hg or the use of antihypertensive agents.
Dyslipidemia: The use of anti-lipid medications or a reading of fasting total cholesterol of over 200 mg/dl.
On-hour admission: Admission between 8.00 and 17.00.
Off-hour admission: Admission between 17.00 and 8.00.
Procedural success: Achievement of less than 20% residual stenosis and TIMI-3 flow in the IRA.
Patient delay: Time between the onset of symptoms and the first medical contact.
Prehospital system delay: Period between first medical contact (FMC) and arrival at a PCI-capable center.
Door-to-balloon time (DTB) or in-hospital delay time: Period from arrival at a PCI-capable center to first blood supply (by balloon or wire).
Total ischemia time (TIT): Period from the onset of symptoms to recanalization IRA flow. It includes all time intervals, such as patient delay, prehospital system delay, and DTB time.
Total procedure time: Period from sheath insertion to final imaging.
We divided the DTB time into two: (1) the emergency department delay time (EDDT) is the time from a patient’s arrival at a PCI-capable center to sheath insertion; and (2) the sheath-to-balloon time (STB) is the time from sheath insertion to recanalization of the IRA (by balloon inflation or wire crossing).
Transthoracic echocardiography
Transthoracic echocardiographic (TTE) images were acquired according to a standard protocol using a GE Vivid 5 (5–1 MHz multifrequency probe, GE Medical Systems, Milwaukee, USA) device in accordance with current European and American guidelines by experienced cardiologists [10]. M-mode, two-dimensional, and color Doppler images were obtained in parasternal, suprasternal, substernal, and apical views with patient position adjustment. The first TTE was performed within 24 h of the primary PCI. The follow-up echocardiography records in the study were obtained from our hospital registries at least 6–8 weeks after pPCI.
PCI procedure
The Judkins technique was used to perform selective coronary angiography. Two experienced invasive cardiologists, unaware of the patients’ clinical conditions, evaluated the coronary angiography records. When performing primary PCI on STEMI patients in our clinic, we used a diagnostic catheter for the left system for right coronary artery (RCA) lesions and a guide catheter for the RCA. A right diagnostic and left system guidance catheter was used for left anterior descending (LAD) and circumflex coronary artery (CX) lesions. One diagnostic catheter and one guide catheter were used instead of the standard two diagnostic catheters.
To further shorten DTB, our center established a cardiac catheterization laboratory that will remain open 24 h a day, 7 days a week, staffed by an in-hospital interventional cardiologist, nurse, and technologist.
Clinical end-point and follow-up
Our study’s clinical endpoint was all-cause in-hospital and 1-year mortality. We obtained 24-month follow-up data of all examined patients from hospital records. The median follow-up time was 48 months.
Statistical analysis
IBM SPSS Statistics version 24 was used to analyze the data. According to whether they were normally distributed, the continuous variables were shown as the median and interquartile range (IQR) (25–75%) or mean ± SD. The Shapiro-Wilks test and histogram were used to confirm that the data had a normal distribution. Percentages were used to express categorical variables, and a χ2 test was performed to compare categorical variables between groups. For continuous variables, the Mann-Whitney U test or Student’s t-test was used for comparison. To identify the determinants of in-hospital mortality, univariate and multivariate logistic regression analyses were carried out. To find determinants of 1-year all-cause mortality, univariate and multivariate Cox regression analyses were carried out. In the multivariate analysis, variables with p < 0.05 were added to the model. Based on prior research and established or conceivable connections with mortality, the predicted candidate factors were chosen. Receiver operating characteristic (ROC) curve analysis was used to assess the association between EDDT and 1-year all-cause mortality. AUC, specificity, sensitivity, confidence interval, and p values were collected and reported. Two separate groups were created according to the cutoff value obtained by ROC analysis. The mortality relationship between the groups was evaluated using Kaplan-Meier analysis. The p-value was used to determine the statistical significance level of the data collected. Statistics were deemed to be significant at p < 0.05.
Results
The cohort belonged mostly to the male gender (690 [77.5]) with a mean age of 60.73 ±13.53 years. The median EDDT was 23 (15–35) min, STB was 10 (7–13) min, and DTB time was 34 (25–48) min. The median total procedure time was 18 (12–26) min. Out of the total group of patients, 418 (47%) were active or past smokers, 356 (40.0%) were hypertensives, 291 (32.7%) were diabetic, and 360 (40.4%) were dyslipidemic. The study cohort demographics and initial clinical characteristics are displayed in Table I.
Table I
Baseline characteristics of the study population
[i] EF – ejection fraction, DM – diabetes mellitus, HT – hypertension, EDDT – emergency department delay time, STB – sheath-to-balloon time, DTB – door-to-balloon time, IRA – infarct-related artery, LAD – left anterior descending artery, CX – circumflex artery, RCA – right coronary artery, PCI – percutaneous coronary intervention, MVI – multivessel intervention, GRAFT – Graft vessels, CCB – calcium channel blockers, OAC – oral anticoagulants, D2B – door to balloon time, ASA – acetyl salicylic acid, ACEI – angiotensin converting enzyme inhibitor, ARB – aldosterone receptor blockers, BB – β-blockers.
Logistic regression analyses for in-hospital mortality
In univariable logistic regression analysis for in-hospital mortality, EDDT (OR = 1.021, CI = 1.01–1.04, p = 0.005), age (OR = 1.106, CI = 1.07–1.14, p < 0.001), female gender (OR = 3.171, CI = 1.52–6.62, p = 0.002), glomerular filtration rate (GFR) (OR = 0.944, CI = 0.93–0.96, p < 0.001), HT (OR = 2.681, CI = 1.26–5.70, p = 0.01) and smoking (OR = 1.332, CI = 1.141–1.783, p = 0.012) were significant. In multivariable logistic regression analysis, age (OR = 1.074, CI = 1.032–1.123, p = 0.04) and GFR (OR = 0.975, CI = 0.938–0.976, p < 0.001) were independent predictors among all causes of in-hospital mortality. The latter did not appear to be correlated with EDDT (OR = 0.994, CI = 0.972–1.017, p = 0.611) (Table II).
Table II
Univariate and multivariate logistic regression analysis for in-hospital mortality
[i] LVEF – ejection fraction, DM – diabetes mellitus, EDDT – emergency department delay time, STB – sheath-to-balloon time, LAD – left anterior descending artery, PCI – percutaneous coronary intervention, MVI – multivessel intervention, GFR – glomerular filtration rate, HT – hypertenstion, DTB – door-to-balloon time.
Cox regression analyses for 1-year mortality
In univariable Cox regression analysis, EDDT (HR = 1.024, CI = 1.016–1.031, p < 0.001), STB time (HR = 1.022, CI = 1.007–1.038, p = 0.004), age (HR = 1.079, CI = 1.061–1.098, p < 0.001), female gender (HR = 2.31, CI = 1.494–3.575, p < 0.001), left ventricle ejection fraction (LVEF) (HR = 0.941, CI = 0.918–0.965, p < 0.001), GFR (HR = 0.959, CI = 0.951–0.967, p < 0.001), DM (HR = 1.618, CI = 1.054–2.485, p = 0.028), and HT (HR = 1.914, CI = 1.248–2.935, p = 0.003) were significantly associated with 1-year all-cause mortality. In the multivariable logistic regression analysis, EDDT (HR = 1.011, CI = 1.002–1.021, p = 0.022), age (HR = 1.044, CI = 1.019–1.068, p = –0.001), LVEF (HR = 0.957, CI = 0.931–0.988, p = 0.003), and GFR (HR = 0.982, CI = 0.966–0.997, p = 0.016) were independent predictors among all causes for 1-year mortality (Table III).
Table III
Univariate Cox and multivariate Cox regression analysis for 1-year all-cause mortality
[i] LVEF – ejection fraction, DM – diabetes mellitus, HT – hypertension, EDDT – emergency department delay time, STB – sheath to balloon time, LAD – left anterior descending artery, PCI – percutaneous coronary intervention, MVI – multivessel intervention, GFR – glomerular filtration rate, DTB – door-to-balloon time.
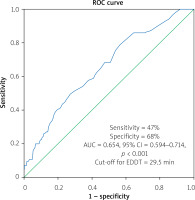
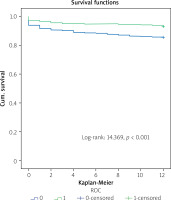
The relationship between EDDT and 1-year all-cause mortality was also examined using ROC analysis. According to ROC analysis, mortality was associated with EDDT with 47% sensitivity and 68% specificity (AUC = 0.654, 95% CI = 0.594–0.714, p < 0.001) (Figure 2). The cutoff EDDT was 29.5 min. According to the Kaplan-Meier analysis, mortality was significantly higher in the group with EDDT of more than 29.5 min (Figure 3).
Discussion
The association between EDDT and 1-year all-cause mortality and in-hospital mortality in STEMI patients who underwent pPCI was investigated in this single-center retrospective analysis. EDDT did not significantly affect in-hospital mortality in the multivariable logistic regression analysis; however, age and GFR did. According to a multivariable Cox regression analysis, EDDT, EF, age, and GFR independently predicted 1-year all-cause mortality.
Studies on time intervals in STEMI patients have generally focused on DTB and TIT. Several studies on the components of total ischemia time are available in the literature [11–14]. In terms of myocardial damage, death, and heart failure in STEMI patients, it is well established that the interval between the onset of symptoms and balloon inflation or wire crossing is crucial [11–14]. Therefore, many studies have been conducted to understand the effects of changes in time intervals in STEMI patients and the reasons for the delays in these time intervals.
Recently, some studies have shown that TIT is a better mortality predictor and quality marker than DTB [11, 15, 16]. Prehospital delay is a significant proportion of total ischemic time. In a cohort, 54.76% of total ischemic time occurred before patients called for help, suggesting that awareness programs can play a role in reducing delay times. Prehospital delays could not be assessed because the retrospective data were equivocal.
The type of FMC significantly impacts the total ischemic time; it was significantly shorter in patients who arrived via ambulance than in those who arrived by self-transport [17]. In a real-world registry, more than 70% of STEMI patients experienced prehospital delays of more than 2 h. Older age, female gender, rural health insurance, hypertension, early morning onset of symptoms, and lack of ambulance facilities have been associated with prolonged prehospital delay [18]. The majority of patients (49.5%) in the nationwide TURKMI registry arrived using self-transport, 11.8% using an emergency medical services (EMS ambulance, and 38.6% were transferred from different EMS without PCI capability centers) [19].
Wang et al. found that a longer first medical contact to balloon (FMCTB) time was associated with larger IS, MVO, and worse recovery of the LVEF. FMCTB time of more than 90-minute duration was an independent prognostic factor of short-term adverse LV remodeling in STEMI patients. A longer FMCTB time is associated with increased mortality [20]. In addition, several previous studies have emphasized that IS predicts adverse remodeling and major cardiac adverse events (MACE) after STEMI [21, 22].
Furthermore, a number of studies have been carried out to assess the impact of DTB on STEMI patients. A recent study by Yamada et al. showed that in-hospital mortality was correlated with DTB time. A DTB time of less than 30 min and cardiogenic shock upon admission were shown to be significantly associated with in-hospital mortality in the multivariable analysis. Compared to those treated with a DTB time of more than 30 min, STEMI patients treated with a DTB time of less than 30-minute duration had considerably superior clinical results [23].
In Korea, Park et al. reported the effects of prompt reperfusion. They observed that a 1-hour delay in DTB time increased 1-year mortality by 55% and a 1-hour delay in symptom onset-to-door time (OTD) time increased 1-year mortality by 4%. Older age, chronic kidney disease, LVEF, DTB time, Killip class, heart rate, cardiogenic shock, and anterior location were independent predictors among all causes of 1-year mortality [8]. Similar to their study, our study showed that older age, GFR, EF, and EDDT were independent predictors among all causes for 1-year mortality; however, instead of DTB, we evaluated EDDT, which is a part of DTB.
Debates continue about the effect of the time of admission on STEMI patient mortality. In a study, Glaser et al. found that STEMI patients undergoing pPCI during off-hours were at a significantly higher risk for in-hospital mortality, myocardial infarcts, and target vessel recanalization [24]. However, Özbek et al. reported that the clinical condition of STEMI patients who were admitted off-hours was worse, and similar results were observed between groups in terms of clinical outcomes [25]. Similarly, in our study, no significant relationship was observed between on-hour admission and mortality in the univariable logistic regression analysis.
STEMI treatment time was reduced by 57%, and the mean DTB time was reduced by 71 min with the in-house interventional team (IHIT) [26]. Our center has a team of in-hospital interventional cardiologists, nurses, and technologists, and a cardiac catheterization laboratory open 24 h a day, 7 days a week, to further shorten the DTB. We attribute our EDDT and DTB to the HAART program being lower than expected.
Previous revascularization history, HT, and DM were not independent predictors among all causes of in-hospital and 1-year all-cause mortality. These comorbidities are likely to affect the prognosis of STEMI patients. The limited number of patients in our study population may have caused this result. The use of antihypertensive, anti-ischemic, and antidiabetic drugs also reduces the mortality of STEMI patients. Perhaps controlled diabetic and hypertensive patients affected our analysis results.
EDDT is the time interval between the patient’s arrival time and the time the angiography procedure begins, and it is a more reliable time interval because it is not subjective as in cases such as out-of-hospital delay and procedure time. Reducing in-hospital delays may contribute to reducing mortality.
No difference in STB time was found between the two groups in the multivariable logistic regression analysis for 1-year all-cause mortality in our study. We believe that the relationship between DTB time and mortality in STEMI patients is actually due to EDDT. Randomized, controlled, and large-scale studies are needed on this subject.
Limitations. Our study has several limitations. First, this was a single-center, retrospective investigation. There were only a few patients in the research population. We were unable to reach patients who first called/activated the EMS time. Therefore, it was not possible to individually assess patient delays and prehospital system delays to determine prehospital delays or total ischemic time. Second, we could not trace how patients arrived at the emergency department (EMS or self-conveyed). Third, we could not evaluate the Killip classification due to a lack of data.