Introduction
One of the most important risk factors for cancer is age; cancer incidence is > 50% and cancer causes approximately 70% of mortality among those aged 65 and above [1, 2]. As the average age of the world population increases, the number of cancer patients in the geriatric age range increases concomitantly. Cancer in geriatric patients deserves special attention at every stage as major changes in body organ systems occur with advanced age. Age-related physiological changes are particularly a problem when facing stressors, such as cancer and therapeutic agents for cancer treatment. Older age may lead to changes in the course of the disease as well as causing a substantial change in the effects and side effects of treatment modalities. Older patients are underrepresented in current cancer practices and in randomized clinical studies; much remains to be elucidated within geriatric oncology research and effective medical practice [3–5].
Bibliometric techniques can be used to identify current trends in a particular area of research. As in other fields of medical science, many bibliometric analyses have been conducted within oncology [6–9]. However, to our knowledge, no bibliometric analysis has previously been performed in geriatric oncology.
In this study, we identified and analyzed the top 100 most-cited papers published between 1983 and 2018. The main objective of this analysis was to identify the authors leading this field, the journals chosen by geriatric oncologists, and the institutions and countries that have focused on this subject. We also aimed to classify articles according to their level of evidence and to identify geriatric age limits, as well as to determine the cancer types most frequently studied and the preferred assessment methods for geriatric evaluation. We aimed to create an easily accessible resource for practicing physicians in this important area of oncology by comprehensively analyzing the most notable articles in the field of geriatric oncology.
Materials and methods
On December 23, 2020, we searched Web of Science (WoS) papers published between 1975 and 2020 using six keywords: “geriat*” OR “older patient*” OR “older adult*” OR “elderly” and “*cancer” OR “oncolog*”. The search was conducted by topic. Initially, we encountered 41,866 studies that were relevant to this subject. We analyzed the studies one by one, starting with the first study that received the highest number of citations. We excluded those not related to geriatric oncology. The 100th most-cited article was the 682nd article in the list; therefore, we excluded 582/682 articles that were unrelated to this subject. We identified the top 100 most-cited articles (termed the T100) and ranked them from 1 to 100 according to citation numbers. Two authors independently identified the T100 with a discussion on any areas of disagreement to reach a consensus.
Citation numbers were provided as an adjusted citation index (ACI; in addition to the total number of citations); articles published earlier could have received more citations, thereby causing bias. The ACI was obtained by dividing the number of citations by the number of years since the publication of the article, such that the ACI indicates the yearly average number of citations.
All studies were analyzed in detail using WoS and PubMed databases. The evidence levels of the articles in the T100 were determined according to the Scottish Intercollegiate Guidelines Network-SIGN 50. Descriptive methods were frequently used in statistical analyses of the studies. Continuous variables were expressed as medians ± interquartile ranges (IQR); categorical variables were expressed as frequencies and percentages. SPSS software for Windows (version: 23.0) was used for all statistical analyses (SPSS Inc., Chicago, IL, US).
All authors declare that the study was conducted according to the principles of the World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. This study did not require approval from an ethics committee as it was designed as a bibliometric analysis of existing published studies.
Results
In the current study of peer-reviewed articles published within the field of geriatric oncology, the T100 median ± IQR citation count was 253 ± 130 (range: 181–1,511) and the median ± IQR of the ACI was 19 ± 8 (range: 7–86). As expected, all identified articles were published in English. The T100 was sequenced according to the total number of citations, and the ACI value of each study was specified (Table 1). One paper received more than 1,000 citations and 14 papers received at least 500 citations.
Table 1
The top 100 cited articles in geriatric oncology
The most-cited article was titled “Underrepresentation of patients 65 years of age or older in cancer-treatment trials”. This article was written by Hutchins et al. and was published in the New England Journal of Medicine (NEJM) in 1999. The paper received 1,511 citations, with an ACI of 68.6. Other papers with high ACIs include manuscripts titled “International Society of Geriatric Oncology Consensus on Geriatric Assessment in Older Patients with Cancer” (written by Wildiers et al.; ACI: 85.71), and “Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study” (written by Hurria et al.; ACI: 83.3). Differences between the rankings made according to the ACI and the total number of citations are presented in Table 1.
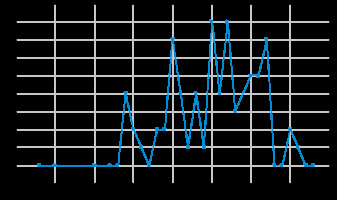
The T100 consisted of studies published between 1983 and 2018. The earliest study – “Clinical trials and drug toxicity in the elderly – the experience of the Eastern Cooperative Oncology Group” – was conducted by Begg et al. and published in the journal Cancer. The most recent study is Mohile et al.’s “Practical assessment and management of vulnerabilities in older patients receiving chemotherapy: ASCO guideline for geriatric oncology”, which was published in the Journal of Clinical Oncology (JCO). Most studies were published in 2005 and 2007 (nine studies were published in each year, and with a sum of 5,500 citations) (Fig. 1).
Evidence levels were analyzed individually following the Scottish Intercollegiate Guidelines Network-SIGN 50. Seventeen studies were prospective cohort studies, 13 studies were retrospective cohort studies, and 12 studies were both randomized control studies and reviews. Ten studies were reports of expert committees. Thirty-seven studies were identified as having Level 1 evidence. A detailed list of study evidence levels is presented in Table 2.
Table 2
Top 100 most-cited articles according to their study designs and levels of evidence
We also analyzed studies using geriatric assessment scales. The two most-studied scales were the Geriatric 8 (G8) and Vulnerable Elders Survey (VES-13) scales; both were analyzed in four studies. A triage risk screening tool was evaluated in two studies.
Fifty papers in the T100 focused on a particular type of cancer. Lung (15), breast (14), and colorectal (13) cancers were the three most studied cancer types. Prostate cancer, glioblastoma multiforme, and hepatocellular cancer were evaluated in two studies each.
Seventy-seven studies in the T100 list defined an age threshold for oncogeriatric patients. While 33 (42%) of these studies accepted 70 as the age threshold for oncogeriatric patients, 29 (37%) accepted 65 as the age threshold. Four studies defined the limit as age 75 and three studies defined it as 80 years.
We summarized information on the countries in which these studies were conducted in the current assessment. The total number of countries represented in the T100 was 25; the United States of America (USA) was the leading country, with 62 studies. Italy ranked second with 19 studies, France ranked third with 18 studies, and England ranked fourth with 16 studies. Apart from the US and European countries, Canada, Australia, and Japan were among the top 15 countries represented in these studies (Table 3).
Table 3
Top 100 most-cited articles according to their geographic origins (with three or more geographic origins)
| Rank | Country | Number* |
|---|---|---|
| 1 | The United States of America | 62 |
| 2 | Italy | 19 |
| 3 | France | 18 |
| 4 | England | 16 |
| 5 | The Netherlands | 10 |
| 6 | Canada | 9 |
| 7 | Switzerland | 9 |
| 8 | Belgium | 7 |
| 9 | Germany | 5 |
| 11 | Australia | 3 |
| 12 | Japan | 3 |
| 13 | Norway | 3 |
| 14 | Scotland | 3 |
| 15 | Spain | 3 |
The Journal of Clinical Oncology was the journal with the highest number of published papers, with 35 papers among the most-cited publications. The Journal of the National Cancer Institute ranked second with 11 studies, and Cancer ranked third with seven studies. A total of 28 journals published all 100 studies.
The author with the greatest contribution to these studies was Hurria, who contributed to a total of nine studies in the T100 list. She was the first author of five of these studies. She was followed by Extermann, who contributed to eight studies, and Monfardini, who contributed to six studies. Authors with contributions to four or more studies in the top 100 most-cited articles are presented in Table 4.
Table 4
Authors with contributions to four or more studies in the top 100 most-cited articles
| Author | Number of top 100 articles | ||
|---|---|---|---|
| Author | First author | Co-author | |
| Hurria A | 9 | 4 | 5 |
| Extermann M | 8 | 5 | 3 |
| Monfardini S | 6 | – | 6 |
| Audisio RA | 5 | 1 | 4 |
| Cohen HJ | 5 | – | 5 |
| Wildiers H | 5 | 2 | 3 |
| Aapro M | 4 | – | 4 |
| Repetto L | 4 | 1 | 3 |
| Tew WP | 4 | – | 4 |
| Yancık R | 4 | 4 | – |
We examined impact factors (IF) as a quality criterion for journals in the T100. The IF of JCO (with the most published papers) was 32.95. The IF of the Journal of the National Cancer Institute, which ranked second among top-cited papers in this analysis, was 11.57. Finally, the IF of Cancer, which ranked third in the current study, was 5.74. The number of articles published, total citations received and the IF of journals that published four or more studies are listed in Table 5.
Table 5
List of journals that published four or more of the reviewed articles
Among the institutes where studies in the T100 were carried out, the most frequently contributing centers were Harvard University (n = 18), the National Institutes of Health (n = 14), Dana Farber Cancer Institute (n = 12), Memorial Sloan Kettering Cancer Center (n = 12), and Unicancer (n = 12). Institutions of origin with 5 or more of the top 100 cited articles are presented in Table 6.
Table 6
Institutions of origin with 5 or more of the top 100 cited articles
Besides medical oncology studies in the T100, four studies were conducted in the field of surgical oncology, and five studies were conducted in the field of radiation oncology.
Discussion
Approximately 70% of patients with cancer are aged 65 years and older [10]. As the world population ages, the number of older patients with cancer will increase concomitantly. However, there is insufficient evidence informing the management of geriatric cancer patients, mainly due to the underrepresentation of this population in clinical studies [11–13]. In the T100 list, Hutchins et al.’s study (the most-cited article of the T100) specifically elucidated this issue. Besides, studies with high levels of evidence are of great importance in geriatric oncology, as in any other oncology sub-field. In this context, we examined articles in the T100 in terms of study type and level of evidence. Thirty-seven studies provided Level 1 evidence. In other bibliometric studies examining the level of evidence, the proportion of papers with Level 1 evidence was lower [6, 14]. This suggests that physicians’ attention in the field of geriatric oncology is directed toward studies of relatively high quality.
Due to developments in healthcare systems, life expectancy is increasing globally. However, it is not clear what the geriatric age limit should be in oncology practice. The International Society of Geriatric Oncology (SIOG) suggests screening with a comprehensive geriatric assessment (CGA) after 70 years of age, based on the fact that geriatric problems increase sharply after that age. On the other hand, the National Comprehensive Cancer Network and ASCO accept 65 years and over when defining older adults. Considering that the most cited physicians (Arti Hurria and Martine Extermann), institutes, and journals in the T100 list are from the USA, this may affect the results. In the T100 list, 65 and 70 years of age were the most preferred age limits, proportionally to each other. As a result, in our opinion, when evaluating the geriatric patient in oncology, it would be better to decide by evaluating the biological age and performance status of the patient instead of only the chronological age.
The author leading the T100 list (in every sense) is Arti Hurria. To shed light on our current practice, we took a closer look at prominent authors within the last decade (≥ 2010). We abstracted information on their countries, clinics, and accomplishments in this field – as a result, three authors stood out: Hurria, Mohile, and Wildiers. Arti Hurria, MD, was a leader in geriatric oncology, embracing the age-associated nuances of the elderly and leading initiatives and research that advanced this specialty field. Supriya Gupta Mohile is working at the University of Rochester. She directs the Specialized Oncology Care & Research in the Elderly (SOCARE) geriatric oncology clinic at the University of Rochester and Highland Hospital. Dr. Mohile is an expert in geriatric oncology, with over 148 publications in this area. She is the editor-in-chief of the Journal of Geriatric Oncology. Hans Wildiers’s career has been dedicated to breast cancer research and geriatric oncology. He previously worked at the University of Leuven. Since 2008, he has chaired the task force for cancer in the elderly within the European Organization of Research and Treatment of Cancer (EORTC). Between 2018 and 2020, Wildiers served as the president of SIOG.
While examining the top 100 studies according to number of citations, we determined the most influential studies based on their ACI. A ranking based on ACI criteria allowed us to overlook time biases. The study with the highest ACI value among the T100 was titled “International Society of Geriatric Oncology Consensus on Geriatric Assessment in Older Patients with Cancer”. This study was conducted by Wildiers et al. (ACI: 85.71) and was published in JCO in 2014. When the first ten most-cited studies were examined according to their ACI (excluding the article that ranked 1st, published in 1999), 9/10 articles were published in 2011 or later, with a median publication year of 2015. The fact that articles with a higher ACI were mostly published recently demonstrates that recent studies are impactful and generating interest, in reflection of the changing tendencies in this field.
A comprehensive assessment is an essential part of geriatric patient management in oncology practice. CGA provides valuable information on different topics. However, in daily practice, the problem of limited time has led to the development of effective but shorter questionnaires. The G8 scale emerged as the most studied scale and was examined in four studies. In one of those studies, Bellera et al. developed and evaluated the G8 screening tool against various reference tests. The G8 consists of seven items from the Mini Nutritional Assessment questionnaire, with an item related to patient age. The primary reference test was based on a set of CGA scales. When considering the primary reference test, G8 tool provided a good sensitivity estimate (85%) without excessive deterioration of specificity (65%) [15]. We also examined trends regarding preferred geriatric assessment scales. A total of 16 studies among the T100 included geriatric assessment scales, 15 of which were published in 2005 or later. In addition, studies using the CGA were published in 2012 or earlier, while studies examining G8, VES13, and/or TRST scales (i.e., more commonly used shorter scales) were more recent (2012 or later).
The most studied cancer types in the T100 were lung, breast, and colorectal cancers. According to global cancer statistics published by Globocan in 2018, these three cancer types are among the top three in terms of incidence; however, their incidence in the population over 65 years is slightly different. While lung and colorectal cancers are the most frequent cancers in this age group, the incidence of breast cancer is lower. Oncologists together with other primary care and specialized physicians have achieved longer survival rates due to screening programs as well as success in the treatment of breast cancer. Therefore, although breast cancer incidence is low in the geriatric age group, its overall prevalence is still high. The high rate of breast cancer studies included within the T100 may be related to this finding.
We also examined the centers generating the most work within the T100. We expected that the pioneering centers would be comprehensive and highly experienced cancer centers. The National Institutes of Health (NIH) is the primary agency of the US government for biomedical and public health research. The National Cancer Institute (NCI) is the oldest institute of the NIH, established in 1937. Dana-Farber is one of the world’s leading cancer centers, a principal teaching affiliate of Harvard Medical School, and is one of the cancer centers designated by the NCI, with over 70 years of experience in cancer treatment. The Memorial Sloan Kettering Cancer Center (MSKCC), founded in 1884 as the New York Cancer Hospital, is a cancer treatment and research institution in New York City. It is another of the 51 NCI-designated Comprehensive Cancer Centers. The geriatric service at MSKCC takes special care of patients aged 65 years and over. In addition to medical management, it also provides services in social work, rehabilitation, emotional support for older patients and their caregivers, and nutrition. Unicancer brings together the French Comprehensive Cancer Centers, promoting their cancer research organizations with 16 oncogeriatric centers. The Unicancer Oncogeriatrics Group brings together oncologists, geriatricians, radiotherapists, surgeons, biostatisticians, and pharmacologists, all working towards promoting clinical research and innovation in oncogeriatrics and tailoring clinical trials for the elderly population by adapting methodological approaches and rationalizing diagnostics and treatments.
Older articles may have been included in the T100 through an increasing number of citations over time, or we may have overlooked some highly cited papers that could not be included in the list because of their publication dates. On the other hand, the fact that a significant part of the most cited studies came from high-income countries, especially from the USA, is a point that should be emphasized. The fact that there are more scientists working in the country and more access to funding are the factors that increase the quality of the studies. Besides, in order to cite a study, it should not be forgotten that the possibilities of access (e.g. open access journals) may differ according to the development level of the country. Because of these limitations, we have avoided making generalizations. Finally, conducting bibliometric analyses based on citations, though quantitative, is a subjective method of evaluating research quality and scientific efficiency, and qualitative assessments and systematic reviews are necessary to better understand this topic.
Conclusions
Our study is the first to analyze the top 100 most-cited studies in geriatric oncology. According to the results, Western high-income countries, especially the USA, were the leading countries, and JCO was the leading journal in geriatric oncologic studies. In the centers where most studies were carried out, the USA was the leader. Also, the fact that the most influential articles were published in the last ten years reflects the increasing interest in geriatric oncology in recent years. As a result, it will be beneficial for clinicians to conduct large-scale, multi-center studies in the field of geriatric oncology, especially involving different geographic regions of the world.