Summary
Iliofemoral vascular complications after transcatheter aortic valve implantation via transfemoral access (TF-TAVI) remain common despite technological improvement in the new-generation transcatheter systems. Detailed analysis of the access site facilitates risk stratification and prevents adverse events that may affect procedural outcomes, especially within the elderly population. Based on the results of the preoperative multi-slice computed tomography (MSCT) we present a systematic screening diagnostic tool that could be predictive of access-related complications after TAVI. We found that an external iliac artery (EIA) greater than 4.48 mm/m² effectively identifies patients at risk of periprocedural access requiring surgical intervention and bleeding complications. Among the diagnostic tools based on MSCT in TAVI patients, the EIA score distinguishes itself by its ability to predict vascular or bleeding complications using a clear cut-off value. The use of advanced preoperative imaging methods based on MSCT, and a multidisciplinary Heart Teams allow for optimization of the results and an increase in the survival rate of patients undergoing TAVI. Distinguished predictors of complications are not included in the commonly used models of cardiac surgery risk assessment (logistic EuroSCORE, STS score). Therefore, we describe a useful a tool that could be applied in risk stratification before TF-TAVI and prediction of periprocedural access site complications in preprocedural planning.
Introduction
Aortic stenosis (AS) is the most common valvular heart disease (VHD) and is associated with high mortality and morbidity when left untreated [1]. With an aging population, the number of patients undergoing valve interventions has significantly increased and is expected to rise further over the following years [2]. Transcatheter aortic valve implantation (TAVI) has been established as a standard of care in patients fulfilling the clinical and demographic criteria outlined in current ESC/EACTS guidelines [3], improving significantly outcomes and quality of life of patients with AS [4]. There is evidence that optimal vascular access selection, based on pre-procedural computed tomography (CT) imaging, shortened procedural time and accelerated recovery [5]. Transfemoral (TF) access is preferred over alternative access if the anatomy and size of iliofemoral arteries are appropriate for the TAVI delivery system. On the other hand, the technical improvements, including reduction of the dimensions of delivery systems, reduced the rate of vascular complications and improved procedural outcomes. However, in the elderly population presenting with comorbidities, including peripheral artery disease and frailty, the iliofemoral arteries are often borderline acceptable for TF access [6, 7]. The degree of vessel tortuosity, vascular calcification and atherosclerotic plaques increase with age and increase the risk of peri-procedural complications. Access site bleeding, pseudoaneurysms, hematoma, and vascular closure device-related failure are among the most prevalent of these [8]. The consequences include prolonged hospital stay, increased mortality, and higher treatment costs. Multi-slice CT (MSCT) is a gold standard for preprocedural planning and a key tool to estimate the risk of potentially life-threating complications and long-term procedural success. MSCT evaluation includes both the aortic root and aortoilio-femoral anatomy, determining the appropriate size of the valve prosthesis and the most feasible access route [9, 10].
Aim
The aim of the study was to evaluate whether the external iliac artery diameter indexed to body surface area (EIAD-BSA) predicts vascular access complications after TF-TAVI and to identify other potentially predictive indicators of unfavorable outcomes.
Material and methods
We retrospectively analyzed 193 patients with severe AS treated with TAVI between 2017 and 2019 at the Upper-Silesian Medical Center of the Medical University of Silesia in Katowice.
A multidisciplinary Heart Team determined the procedural approach. All patients underwent a diagnostic workup, including transthoracic echocardiography and MSCT of the aortic valve, complete aorta, and the femoro-iliac arteries. TAVI procedures were performed according to in-house standard operating procedures either under general anesthesia or conscious sedation with local anesthesia. The CFA was punctured under fluoroscopic guidance. A vascular closure device (ProGlide; Abbott or Manta; Teleflex) was used in all procedures. In case of any symptoms indicating access-related complications patients were referred for imaging testing, including Doppler ultrasound, MSCT, or angiography.
This retrospective study did not require approval of the bioethics committee. The diagnostic tests were carried out using contrast-enhanced CT (Toshiba Aquilion 64 and SOMATOM Force; Siemens Healthineers). Each patient received an average 70 ml of intravenous contrast (Iomeron 400 or Ultravist 370). The images were reconstructed with an average layer thickness of 0.6 mm (range: 0.5–1.5 mm).
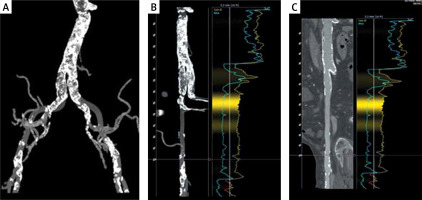
The evaluation of the femoral vessels included: the minimum lumen diameter (MLD) and cross-sectional area (CSA) of the common iliac, external iliac, and common femoral arteries; the presence of calcifications, their type, extent and location using a dedicated software package (3mensio, Pie Medical Imaging, Bilthoven, The Netherlands) (Figures 1, 2). The diameter of the ilio-femoral arteries was measured in the axial projection perpendicular to the longitudinal axis of the vessel. The diameter of the vessel was defined as the distance between the inner contours of the arterial wall. If calcifications protruding into the lumen were present, the diameter was defined as the vessel lumen minus the thickness of calcification. Measurements were indexed to body surface area (BSA) and body mass index (BMI). Periprocedural data – size of delivery system, type of hemostatic device (ProGlide/Manta) – were analyzed. The distribution of ilio-femoral vessel sizes in the study population were correlated with periprocedural and short-term results. TAVI access site complications were identified either in the implantation protocol or in the electronic patient files, according to Valve Academic Research Consortium 3 (VARC-3) [11]. Clinical data were retrieved from the hospital’s database. Data on 30-day and 1-year follow-up were obtained from the administrative database of the National Health Fund (NFZ). No patients were lost to follow-up. The data underlying this study will be available upon reasonable request.
Figure 1
Vessel assessment. Femoral and iliac arteries were reconstructed from MSCT data depicting the vascular anatomy from the aorta to the femoral bifurcation
Figure 2
Vessel assessment – calcifications. A – Overview; B, C – MSCT – reconstruction of the stretched iliofemoral arteries and contour analysis
Statistical analysis
Distribution of the variables was assessed with the Shapiro-Wilk test. Data are expressed as means and standard deviations (SD). Relative frequencies are used to present categorical variables. Continuous data are expressed as mean and standard deviation (SD) or median with interquartile range when appropriate. Student’s t-test and the Mann-Whitney U test were used. Categorical variables were compared using the χ2 test. Differences were considered significant at p < 0.05.
Results
Demographics
Our analysis included 193 consecutive patients who met the criteria of symptomatic AS and underwent TF TAVI. Clinically relevant baseline characteristics are summarized in Table I. The median age was 79 (75–83) years; 63% patients were female. The most prevalent concomitant diseases included coronary artery disease (64%), diabetes (41%), atrial fibrillation (37%) and PAD (26%). Mean glomerular filtration rate (GFR) (ml/min × 1.72 m²) was 58.97 ±16.5. Perioperative mortality risk was presented as the STS score and logistic EuroSCORE of 4.2% (2.5–7.9) and 14.2% (11.8–18.9) respectively. The distribution of TAVI systems was as follows: EvolutR (Medtronic) n = 97; Sapien 3 (Edwards Lifesciences) n = 48; Portico (Abbott Laboratories) n = 28, Accurate neo (Boston Scientific) n = 18; Lotus (Boston Scientific) n = 2.
Table I
Characteristics of the study population (n = 193)
[i] Results are presented as mean (± SD) and median (interquartile range) for normally and non-normally distributed data, respectively; categorical data as total number (percentage). BMI – body mass index, BSA – body surface area, PCI – percutaneous coronary intervention, CABG – coronary artery bypass grafting, TIA – transient ischemic attack, GFR – glomerular filtration rate, NYHA – New York Heart Association, LVEF – left ventricular ejection fraction, P2Y12 – oral inhibitors of platelets, DAPT – dual antiplatelet therapy, VKA – vitamin K antagonists, NOAC – non-VKA oral anticoagulants.
Access vessels
The mean external iliac artery diameter indexed to BSA ratio (EIAD-BSA) was 4.65 ±2.04. Based on this threshold, the patients were divided into two groups: high EIA ≥ 4.48 mm/m² (n = 86) and low EIA < 4.48 mm/m² (n = 107). Patients with larger EIAD-BSA presented: higher STS score, 15.6 (11.6–18.9) vs. 13.2 (11.0–17.1), p = 0.033; higher prevalence of coronary artery disease, n = 62 (72%) vs. n = 61 (57%), p = 0.031; and history of coronary angioplasty, n = 41 (48%) vs. n = 34 (32%), p = 0.019. The quantity and the location of calcifications did not show a statistically significant difference between the two study groups (Table II). No other significant difference in major risk factors or comorbidities evaluated prior to the procedure was detected.
Table II
Comparison of vascular closure device, vascular sheath measurements and calcifications between two groups
Access site complications
Vascular and access-related complications including bleeding occurred in 17.1% of patients (Table III). Major TAVI access site complications (VARC-3) were reported in 5.7% of patients, while minor complications (VARC-3) occurred in 2.6%. Type 2 bleeding according to VARC-3 was observed in 1 (1%) patient and more severe type 3 bleeding in 10 (5%) subjects. Tamponade alone was documented in 6 (5%) cases. 23% of the analyzed patients required a blood transfusion. Three (1.6%) patients died during the procedure, while 8 (4.2%) died during hospitalization.
Table III
Vascular complications during hospitalization
The analysis revealed that the external iliac artery diameter indexed to BSA ratio (EIAD-BSA) demonstrated a positive correlation with the composite primary endpoint of access site complications requiring surgical intervention or blood transfusion. Adverse events related to the access site observed during hospitalization are shown in Table IV. Patients with greater EIA had a significantly higher number of complications requiring surgical intervention or blood transfusion: n = 12 (5%) vs. n = 4 (4%), p = 0.011. No difference was observed regarding the length of hospital stay, 8 (7–10) vs. 7 (7–10), p = 0.21; mortality during the procedure, 1 (1.2%) vs. 2 (1.9%), p = 0.69; in-hospital death, 3 (3.5%) vs. 5 (4.7%), p = 0.68; 30-day mortality, 4 (4.7%) vs. 7 (6.5%), p = 0.57; or 1-year mortality, 6 (7%) vs. 6 (6%), p = 0.57. A higher EIAD-BSA did not correlate with the type of vascular closure device selected during the procedure, or with the vascular sheath diameter responsible for delivering the valve or the valve type.
Table IV
Complications near access site during hospitalization
Discussion
The development of transcatheter aortic valve replacement has constituted a landmark achievement in interventional cardiology within the last two decades. Growing clinical experience and continuous refinement of devices and procedural techniques have been associated with improved periprocedural outcomes. Transfemoral TAVI was associated with a significant reduction of mortality or disabling stroke compared to surgical aortic valve replacement, in patients with intermediate operative risk [12]. When compared to other more invasive vascular approaches, TF-TAVI has been consistently associated with improved survival, shortened hospitalization and improved quality of life [13–15]. One study compared the incidence of bleeding and cerebrovascular events after TF-TAVI vs. transapical access, and found that the TF approach reduced the mortality of patients after TAVI, due to the lower incidence of periprocedural bleeding and stroke [16]. On the other hand, we previously reported that despite higher baseline surgical risk and complicated anatomy, transcarotid access is safe and associated with similar results when compared to transfemoral access, and these findings were in line with studies from other high-volume centers [17, 18]. However, the totality of evidence has led transfemoral TAVI to become the recommended vascular approach.
According to multiple reports, the incidence of vascular complications in patients undergoing TAVI ranges from 5% to 50% [19–21]. This wide range is related to the initial lack of clear definitions for assessing the severity of vascular complications. Valve Academic Research Consortium-3 (VARC-3) defines the criteria for periprocedural complications in patients after TAVI, allowing for comparisons using independent studies [11, 22]. Our study revealed an overall prevalence of postprocedural vascular complications of 17.1%, which corresponds with the available scientific data.
Predictors of vascular complications in patients undergoing TAVI constitute a significant clinical problem and are the subject of analysis of many other researchers [23, 24]. The analysis of the ilio-femoral assessment using MSCT became an important goal in estimating the procedural risk. It was reported that the sheath to femoral artery ratio (SFAR) threshold of 1.0–1.05 was associated with a higher rate of vascular access site complications in transfemoral TAVI [25–27]. In contrast, some authors suggested that delivery sheath size above that value had no significant impact on vascular complications; therefore, the accurate impact of the vascular sheath measurements before TAVI does not seem to be clearly defined. To our knowledge, there is no standardized parameter for measuring the sheath to access site vessel ratio and there are insufficient published data on the effect of the real external ratio of the vascular sheath to the vessel diameter.
The further search for a perfect predictor of vascular events led to a series of studies describing potential candidates [28]. The iliofemoral tortuosity (IFT) score [((true vessel length/ideal vessel length) – 1) × 100] demonstrated a good positive correlation with access and bleeding complications [29]. Meanwhile, the iliac morphology score (IMS), composed of ipsilateral minimum iliac diameter and iliac calcification, proved to be a decent predictor of major vascular complications and mortality in patients undergoing transfemoral TAVI [29].
Our study demonstrated that external iliac artery diameter indexed to BSA (cut-off 4.48 mm/m²), with 75% sensitivity and 59% specificity, provides an independent and objective parameter that can facilitate the appropriate selection of the access vessel. Patients with EIAD-BSA ≥ 4.48 (mm/m²) had numerically higher risk for access site complications requiring surgical intervention or blood transfusion: n = 12 (5%) vs. n = 4 (4%), p = 0.011.
There is conflicting evidence regarding the relationship between access site calcification and vascular complications [30, 31]. Our analysis suggested no meaningful effect of the presence, type or extent of calcifications on the risk of access site complications. In contrast, Langouet et al. found that moderate and severe calcifications, the degree of tortuosity of the iliac-femoral vessels and the SFAR score are significant prognostic factors for the occurrence of vascular complications after TAVI [32].
We hypothesize that not only the degree of calcifications presented at the puncture site but also the operators’ experience and the use of different vascular closure devices (VCDs) all contributed to opposite outcomes. VCDs provide faster hemostasis, fewer complications and earlier mobilization in patients after TAVI. Multiple reports revealed that the use of both the Manta and Perclose ProGlide systems guarantees a fast and reliable procedure with a low complication rate [33, 34]. Our analysis demonstrated that the application of both Manta and ProGlide, regardless of the size of the vessel, does not directly correlate with the external iliac artery diameter indexed to BSA score; however, the direct relationship between the type of vascular closure device and vascular complications in both groups has not been analyzed due to the low number of outcome events.
Ultimately, the influence of vascular complications on early mortality is ambiguous and largely depends on the application of VARC criteria. While certain major access site complications are definitively linked with an increased early mortality rate, not every complication has shown a statistically significant difference [23, 25, 30, 35]. Accordingly, our analysis did not demonstrate the association of vascular complications and the mortality during hospitalization and the 30-day mortality.
Limitations
Several limitations must be considered when interpreting the results of this analysis. First, the study was retrospective, non-randomized, and limited to a single center. On the other hand, the use of objective quantitative data such as EIAD-BSA, vascular complications and short-term mortality as hard endpoints may mitigate the potential confusion resulting from the retrospective project. Second, patients with very small vessel diameters or severe calcifications may have been precluded from this study. The application of different devices with different sizes and catheter flexibility may be another limitation. The study population is represented by patients in advanced age, with numerous comorbidities and frailty, or during anticoagulation, which increase the risk of periprocedural complications. The clinical event rates were low, with limited power for evaluation of individual or composite vascular complication outcomes.
Conclusions
Vascular complications in patients undergoing transfemoral TAVI constitute a significant clinical problem. Detailed analysis of the access site facilitates risk stratification and prevents adverse events that may affect procedural outcomes, yet dedicated predictor models to simplify these steps are lacking. Our study demonstrated that EIA greater than 4.48 mm/m² effectively identifies patients at risk of vascular complications, and EIA diameter indexed to BSA (EIAD-BSA) could be useful in predicting access site complications in the preprocedural planning before TF-TAVI. However, due to the small number of participants, any conclusions derived from this study should be considered exploratory.








