Introduction
Heart valve surgery is associated with a risk of serious post-operative complications, including death [1]. Commonly used calculators for cardiac surgery risk assessment, such as EuroSCORE II and STS, have limitations due to limited discrimination and calibration [2–7]. It has been demonstrated that biomarkers such as troponin T, red cell distribution width or the number of erythrocytes determined before heart valve surgery are predictors of death in the early postoperative period [8–11].
N-terminal pro-B-type natriuretic peptide (NT-proBNP) is a prohormone secreted into the blood by cardiomyocytes (mainly the left ventricle) participating in the regulation of water-sodium management and maintenance of homeostasis of the cardiovascular system. The active form of the hormone (B-type natriuretic peptide) increases the glomerular filtration as well as the reduction of sodium resorption in the kidney and inhibits the secretion of renin and aldosterone. B-type natriuretic peptide (BNP) also inhibits the activity of the sympathetic system and directly affects the dilation of blood vessels; moreover, BNP is a hormone that counterbalances the neurohumoral mechanisms triggered in the process of developing heart failure. The process of secretion of NT-proBNP by cardiomyocytes occurs in response to increasing their voltage when the initial or subsequent load increases. The increase in the concentration of BNP and NT-proBNP in the blood indicates the activation of the compensation mechanism that occurs before the onset of symptoms of heart failure [12–14]. Information on the usefulness of NT-proBNP in patients with aortic stenosis undergoing aortic valve surgery is limited and needs to be supplemented with an evaluation of its usefulness as a predictive factor [15–17].
Aim
Because there is a need to supplement the risk assessment tools in patients undergoing aortic valve replacement, we decided to evaluate the suitability of NT-proBNP in patients with aortic stenosis.
Material and methods
This is a prospective study of consecutive patients with hemodynamically significant aortic stenosis (a mean pressure gradient ≥ 40 mm Hg and/or a valve area below 1 cm2) that were approved for cardiac surgery and subsequently underwent elective surgery replacement of the valve, with or without additional procedures at the Institute of Cardiology in Warsaw, Poland. The exclusion criteria were: active endocarditis, active neoplastic diseases, age under 18 years, a lack of consent to participate in the study, significant atherosclerotic changes in the coronary arteries. Once a patient gave his/her consent to participate the following data were collected: age, body mass index (BMI), gender, comorbidities, the results of echocardiography findings, the assessment of the coronary arteries, the risk of surgery using EuroSCORE II. One day before surgery a blood sample for the measurement of biomarker levels was collected from each patient. Complete blood count was performed with K2-EDTA samples, using a Cobas 6000 electronic counter (Roche, Mannheim, Germany). The plasma levels of NT-proBNP concentrations were measured by the electrochemiluminescent immunoassays Elecsys 2010 (Roche, Germany). In all patients procedures were performed through a midline sternotomy incision under general anaesthesia in normothermia. All patients were given cold blood cardioplegia at the initial dose of 15–20 ml/kg followed by booster doses of 5–10 ml/kg every 20 minutes. The primary composite end-point consisted of death from all causes as well as: postoperative myocardial infarction (defined as the development of new Q waves in two or more leads on an electrocardiogram or alterations of myocardial contractility that did not previously exist in echocardiography), stroke, hemodynamic instability (the need for supply of mechanical circulatory support – intraaortic balloon pump or extracorporeal membrane oxygenation despite the inclusion of catecholamines), postoperative renal failure requiring renal replacement therapy (the decision to start hemodiafiltration was made by the team of anesthesiologists responsible for the patient with the diagnosis of AKI and persisting high parameters of the kidneys and anuria despite intensive conservative treatment), prolonged mechanical ventilation (longer than 24 hours, or the need for reintubation) and the occurrence of multiple-organ failure (based on laboratory parameters and/or the need to use organ replacement therapy). The follow-up of patients was conducted through direct observation during hospitalization, telephone interviews, or clinic visits for 30 days after the surgery. The protocol was approved by the Institutional Ethics Committee, number 1705.
Statistical analysis
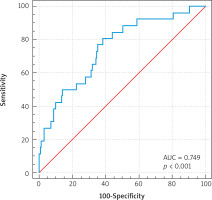
The statistical analysis was carried out using SAS version 9.2. Univariate and multivariate logistic regression was used to assess relationships between variables. The preoperative covariates – age, body mass index (BMI), stroke in history, atrial fibrillation, coronary artery disease, peripheral atherosclerosis, diabetes mellitus, hypertension, chronic obstructive airways disease, chronic kidney disease (GFR < 60 ml/min/1.73 m2), left ventricle ejection fraction, pulmonary blood pressure, NYHA classes, bilirubin, creatinine, high-sensitivity troponin T (hs-TnT) and NT-proBNP – were investigated for an association with the endpoint. Significant variates (p < 0.05) identified from univariate analysis were entered into multivariate models. The predictive value of NT-proBNP was assessed by comparison of the respective areas under the receiver operator characteristic curves. The Youden index was used to determine the cut-off point that meets the criterion of maximum sensitivity and specificity for the primary end-point.
Results
The study included 245 patients who underwent aortic valve replacement with or without concomitant procedures on the ascending aorta. The mean age in the study group was 66 ±11 and there were 149 (61%) men. In 160 patients a biological aortic valve prosthesis was implanted, and in 85 a mechanical valve. Fourteen (5.7%) patients had significantly impaired left ventricular systolic function (ejection fraction < 35%). The mean plasma preoperative NT-proBNP level was 1051 ±939 pg/ml. Baseline characteristics of the patients are presented in Table I. The primary end-point occurred in 74 patients: perioperative renal failure in 14 patients, prolonged mechanical ventilation in 29 patients, stroke in 7 patients and mechanical circulatory support in 6 patients. Multi-organ failure was observed in 23 patients. Myocardial infarction occurred in 5 patients. Eight patients died during the follow-up period as a result of gradually increasing multi-organ failure. In 15 patients more than one major complications occurred. The actual mortality was 3.2% vs the mortality 2.9% predicted by the EuroSCORE II model. Statistically significant predictors of combined end-point at univariate analysis are presented in Table II. In multivariate analysis NT-proBNP (OR = 1.208; 95% CI: 1.098–1.314; p = 0.01), age (OR = 1.037; 95% CI: 1.006–1.068; p = 0.02) and NYHA classes (OR = 2.132; 95% CI: 1.154–3.936; p = 0.01) remained independent predictors of the composite endpoint. A correlation was found between the level of NT-proBNP and hs-TnT (r = 0.27; p < 0.001), EF (r = –0.48; p < 0.001), NYHA class (r = 0.3; p < 0.001) and pulmonary blood pressure (r = 0.48; p < 0.001). The optimal cut-off point for the primary endpoint was calculated as 1254 pg/ml NT-proBNP. The area under the receiver operator characteristic curve for postoperative major complications including death for NT-proBNP is 0.749 (95% CI: 0.713–0.785) (Figure 1).
Table I
Baseline characteristics of the study population (n = 245)
| Preoperative characteristics of patients | Values |
|---|---|
| Age [years]* | 66 ±11 |
| Male: men, n (%) | 149 (61) |
| Body mass index [kg/m2]* | 27 ±5 |
| Atrial fibrillation, n (%) | 62 (25) |
| Stroke in history, n (%) | 15 (6) |
| Diabetes mellitus, n (%) | 47 (19) |
| Peripheral atherosclerosis, n (%) | 15 (6) |
| Hypertension, n (%) | 118 (48) |
| Current smoker, n (%) | 72 (29) |
| Chronic obstructive airways disease, n (%) | 29 (12) |
| Chronic kidney disease (GFR < 60 ml/min/1.73 m2), n (%) | 66 (27) |
| LV ejection fraction (%)* | 59 ±11 |
| Pulmonary blood pressure [mm Hg]* | 39 ±15 |
| NYHA I, n (%) | 2 (1) |
| NYHA II, n (%) | 138 (56) |
| NYHA III, n (%) | 101 (41) |
| NYHA IV, n (%) | 4 (2) |
| EuroSCORE II* | 2.9 ±2.5 |
| NT-proBNP [pg/ml]* | 1051 ±939 |
| Hs-TnT [ng/l] | 25 ±13 |
| Bilirubin [µmol/l]* | 13 ±9 |
| Creatinine [mmol/l]* | 90 ±2 |
| Ascending aortic aneurysm, n (%) | 24 (10) |
Table II
Univariate analysis of predictive factors for occurrence of the composite endpoint
Discussion
This is one of the few studies showing the prognostic significance of NT-proBNP in patients with valvular heart disease. In the present study, the parameter NT-proBNP was found to be an independent predictor of death and serious postoperative complications in a prospective study in patients undergoing aortic valve replacement surgery because of severe stenosis at the 30-day follow-up. The actual mortality in the present study was about 3% and was close to the risk assessed using the EuroSCORE II model. The main cause of death was gradually increasing multi-organ failure. In the presented group, in which the average age was about 66 years, in 34% of patients a mechanical aortic valve prosthesis was implanted. It is worth noting that as many as 25% of patients before cardiac surgery had indications for anti-clotting treatment due to the presence of atrial fibrillation. The present study showed a significant correlation between NT-proBNP values and left ventricular ejection fraction, NYHA class and pulmonary artery pressure.
In the available literature, the utility of NT-proBNP as a predictive factor in patients with heart failure, coronary heart disease, myocardial infarction or mitral and aortic regurgitation has been described [18–24]. Information on the utility of NT-proBNP in patients undergoing valve surgery is limited. Georges et al. found that changes in NT-proBNP concentrations in the early post-operative period in patients operated on due to mitral regurgitation or aortic stenosis did not significantly correlate with the severity of cardiac valve disease [25]. Filsoufi et al. in a prospective study in a group of 42 patients undergoing mitral valve surgery found that the pre-operative level of BNP was not a predictor of complications in the early postoperative period [26]. On the other hand, in a study of a group of 75 patients undergoing mitral valve surgery, the preoperative NT-proBNP was an independent predictor of serious complications in the 30-day observation [27]. Moreover Jiang et al. reported that the NT-proBNP level assessed on the first day after aortic valve surgery provided good discrimination of postoperative heart failure and identifies patients at particular risk of poor long-term survival [15].
It is worth noting that the level of NT-proBNP is taken into account when qualifying patients for surgery because of valvular heart disease. On the one hand, higher values are an indication for qualification for valvular heart disease surgery, especially in asymptomatic patients [28–30]. The results of the present study indicate at the same time that pre-operative decompensation of the circulatory system in the group of patients with aortic stenosis expressed by high values increase in NT-proBNP may be associated with an increase in serious post-operative complications, including death.
Conclusions
The results of this study indicate that NT-proBNP is a useful parameter for estimating the risk of postoperative complications including death in patients with aortic stenosis. Further studies are needed regarding the usefulness of NT-proBNP as a predictor of complications in patients with heart valve disease undergoing cardiac surgery. The results of our research may be helpful in the perioperative strategy in patients undergoing aortic valve surgery.