Introduction
The first reports on treating lung metastases from cancer appeared in the second half of the 19th century. Initially, randomized and then selective screening of patients was used. The first publications appeared in Germany (Weinlechner) in 1882. According to the available data, it was he who performed the first metastasectomy of two pulmonary lesions detected accidentally during the removal of a tumor of the chest wall. In turn, the first planned resection of pulmonary metastases was performed by Divis in Europe in 1927, and then in 1930 by Torek in the United States. In 1934 Edwards from Brompton Hospital performed a lobectomy for metastatic sarcoma, and in 1939 Barney and Churchill removed the metastasis of kidney cancer. The patient survived the procedure for 23 years. In 1947, Alexander and Haight from Michigan described 24 cases of secondary neoplastic lesions treated with surgery in the lungs. Their work brought new rules of conduct. For the first time, they proposed to systematize the eligibility criteria for surgery. At the same time, they recommended the necessity of aggressive control of changes in the lungs with the possibility of performing subsequent resections on the same patient. They also suggested introducing new criteria for the treatment of pulmonary metastases. Firstly, the primary lesion had to be monitored, secondly, the condition of surgical treatment was the absence of extrapulmonary metastases, and thirdly, the patient had to have respiratory reserves to perform the previously assumed range of resection. These criteria, confirmed in later years by Ehrenhaft (1958) and Thornford (1965), with some additional modifications, are still valid today. The 1950s were a period of evolution of this type of surgery due to the introduction of routine chest images in oncological patients (which allowed for earlier detection of changes in the lungs). Moreover, the qualification criteria introduced by Alexander and Haight became rational guidelines accepted by most doctors. Initially, anatomical resections of the pulmonary parenchyma accounted for the vast majority of procedures. It resulted from the conviction that such a scope of surgery was necessary, which would allow for radical removal of the disease. And so, in 1957, Gleidman reported 29 metastasectomies, 17% of which were pneumonectomies. In 1965, a study was published involving a group of 205 patients who underwent 222 resections of the pulmonary parenchyma. In this group, pneumonectomies accounted for as many as 15%. The 1970s turned out to be a key decade in the treatment of metastases [1, 2]. The introduction of chemotherapy resulted in long-term remissions. In combination with surgical treatment, the hope for increasing the effectiveness of the treatment of secondary neoplastic lesions increased. In 1970, the results of a study from the Memorial Sloan-Kettering Cancer Center were published. They concerned many years of studies of patients with sarcomas who underwent surgical treatment of lung metastases. Ultimately, 5-year survival was found in 32% of cases. The International Registry of Lung Metastases continued to be the largest registry. This database contains data of patients treated at multiple centers all over the world. In 1997, Pastorino, based on these data, published a paper describing 5,206 cases of lung metastases. To this day, it is quoted in all published works in this field. However, there are still many unanswered questions. Does metastasectomy really prolong life, does it inhibit the disease progression, what is the significance of lymph node removal and are the obtained data on the status of the lymph nodes useful in further management, is chemotherapy needed for surgical resection and how timely should it be coordinated, what surgical access should be used in a planned metastasectomy and, therefore, is manual palpation of the lung parenchyma absolutely necessary in the era of imaging examinations (CT, PET-CT)? Finally, what are the possibilities of monitoring the secondary proliferative process based on the assessment of tumor markers? The main problem that makes it difficult to draw certain statistically confirmed conclusions is the inability to conduct prospective research. It is difficult to compare patients treated surgically with the group of patients who, being at a similar stage of the proliferation process, would undergo alternative treatment. There are many variables that influence prognosis and therefore survival. Over the years, based on the experience gained and the multicenter analyses carried out, it was determined which elements of the surgical treatment affect the prognosis. Factors such as the radicalism of the operation, disease-free interval (DFI) time, single metastasis in the lung parenchyma, small lesion size, and the histological type of the primary tumor differentiating the prognosis do not raise doubts in general. Some doubts are raised by the issue of the progression of secondary proliferative disease, which results in a greater number of metastasectomies. The results published in the literature differ, but in general the authors tend to believe that survival is longer in patients operated on more than once. However, this thesis is already wrong in its initial assumption. It consists in the fact that the patient who undergoes another operation must meet the oncological and systemic conditions that allow such treatment. Therefore, this group must have a better prognosis if it is possible to perform another operation. Moreover, we cannot compare these patients to others who would not receive such treatment. Here, too, often erroneous results of publications dealing with this problem are produced. In our previous studies, after creating two comparable groups of patients, we found longer survival in patients without relapse after metastasectomy (median survival 71 months without relapse versus 36 months with relapse) [3, 4]. Subsequent metastasectomies are directly related to disease progression. It should be remembered that they worsen the quality of life. They increase pain and organ dysfunction, and cause perioperative stress. That is why it is so important to find out what factors may influence the relapse/progression of the disease and to have knowledge about the chances of extending the life span already in the planning phase of the next treatment. Given the above, factors influencing progression-free survival (PFS) were investigated. This parameter is directly related to overall survival (OS) and is sometimes used as an alternative. According to various authors, in some neoplasms both times are related, while in others they are not. 5-year survival after pulmonary metastasectomy, depending on the histological type of the primary tumor, ranges from 35.5% to 47% in renal cell carcinoma, 39.1% to 67.8% in colorectal cancer, 29% to 52% in soft tissue sarcoma, 38% to 49.7% for osteosarcoma and 79% to 94% for non-seminomatous embryonic tumors [5, 6]. The PFS parameter, occurring earlier than death, allows for a faster and more accurate assessment of the effectiveness of current treatment.
Aim
The factors influencing PFS after the first metastasectomy and thus their impact on OS were investigated. In addition, an attempt was made to determine the strength of the influence of individual factors considered prognostically significant on the relapse of the disease and its consequences.
Material and methods
A group of 577 patients treated surgically at the Institute of Tuberculosis and Lung Diseases in Warsaw in 2002–2019 was analyzed. For the purposes of the present analysis, PFS was defined as the time from the first metastasectomy to the next operation or to the date of death from any cause. Alternatively, it was defined as the time from the first metastasectomy to the end of the study, assuming the patient was alive at that date. The influence of various factors influencing PFS was investigated. Gender, age, unilateral or bilateral surgery, radicality of the procedure, DFI time, and lymph node status were taken into account. The histological type of the tumor was associated with the location of the primary tumor. Thus, adenocarcinomas originating from the large intestine, renal carcinomas (mostly clear cell carcinoma), sarcomas originating jointly from soft tissues and the osteoarticular system, and testicular germinal tumors were distinguished.
Statistical analysis
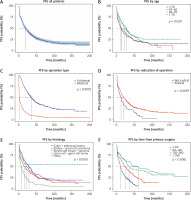
The tabular results present one-dimensional analyses of PFS and a multivariate analysis of this issue. Descriptive statistics were presented as 1, 3, and 5 years of survival using the Kaplan-Meier estimator. One-dimensional comparisons were performed using the log-rank test and multi-dimensional comparisons were performed using multivariate Cox regression. The research was carried out using the statistical software R version 4.0.2 (R Core Team 2020. R: Statistical computing language and environment. R. Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/) [7].
Results
The factors influencing PFS were investigated. It was established that the probability of 1-year and 5-year relapse-free survival (PFS) in the whole group was 60.7% and 24.4%, respectively. One-way analyses showed that statistically significantly longer PFS was observed in older patients. The 1-year PFS, respectively, was 69.5% and 68.7% in the over 60 and over 70 age groups compared with 51% and 55.6% in the under 50 and 50–60 age groups, respectively. Patients undergoing unilateral metastasectomy have a significantly longer PFS compared to those undergoing bilateral surgery (1-year PFS 82.7% vs. 25.3%, respectively). Another element analyzed was the radicalism of the metastasectomy performed. A higher probability of longer PFS was found in completely operated patients. 1-year PFS in this group was 61%, 3-year PFS 35% and 5-year PFS 26%. Patients with no surgical margin, respectively, achieved 1, 3 and 5-year PFS of approximately 50%, 22% and 10%. Histology of the tumor in connection with the location of the primary tumor established that the highest PFS occurs in cases of colorectal adenocarcinoma. In 1 year it is 71%. In follow-up, PFS drops quite significantly to 23% after five years, equating to kidney cancer. In turn, the lowest PFS was observed in patients with bone/soft tissue sarcomas (1 year – 37%, 5 years – 9%). At the start of treatment and follow-up of 1 year, PFS was 64%, second only to colorectal adenocarcinoma. The DFI time influenced the PFS parameter, which was particularly noticeable in the 3- and 5-year observations. The presence of lymph node metastases and gender did not differentiate the PFS. Detailed data are presented below (Table I). A multivariate Cox analysis was also performed. It confirmed the predictive value of unilateral radical metastasectomy and the effect of longer time since primary surgery as factors increasing the probability of prolongation of PFS. The histological type showed a similar pattern as in the univariate analysis. The influence of age was not as strong as in the univariate analysis. Lymph node metastases and gender did not differentiate PFS. Details of the multivariate Cox regression are presented below (Table II).
Table I
Survival estimates overall and by group
| Characteristic | Time 12 | Time 36 | Time 60 | P-value1 |
|---|---|---|---|---|
| Overall | 60.7% (56.8%, 64.8%) | 34.6% (30.9%, 38.8%) | 24.4% (20.9%, 28.4%) | |
| Sex: | 0.065 | |||
| Female | 62.7% (57.1%, 69.0%) | 39.4% (33.7%, 45.9%) | 28.7% (23.4%, 35.2%) | |
| Male | 59.1% (53.9%, 64.7%) | 30.8% (26.1%, 36.4%) | 20.8% (16.6%, 26.2%) | |
| Age group: | 0.029 | |||
| < 50 | 51.0% (43.6%, 59.7%) | 30.2% (23.6%, 38.5%) | 20.7% (14.9%, 28.7%) | |
| 50–60 | 55.6% (48.4%, 63.9%) | 31.0% (24.6%, 39.1%) | 21.1% (15.4%, 28.7%) | |
| 60–70 | 69.5% (62.8%, 76.8%) | 38.5% (31.6%, 46.8%) | 29.3% (22.7%, 37.9%) | |
| > 70 | 68.7% (60.1%, 78.5%) | 40.4% (31.7%, 51.6%) | 27.2% (19.2%, 38.5%) | |
| Operation: | < 0.001 | |||
| Unilateral | 82.7% (78.8%, 86.7%) | 50.1% (45.0%, 55.7%) | 35.1% (30.1%, 40.9%) | |
| Bilateral | 25.3% (20.2%, 31.8%) | 9.93% (6.68%, 14.8%) | 7.47% (4.66%, 12.0%) | |
| Radical surgery: | 0.004 | |||
| No | 50.0% (38.3%, 65.3%) | 22.2% (13.5%, 36.6%) | 9.88% (4.20%, 23.2%) | |
| Yes | 61.6% (57.5%, 66.0%) | 35.5% (31.5%, 39.9%) | 25.8% (22.1%, 30.2%) | |
| Hist/primary tumor: | < 0.001 | |||
| Colon-adenocarcinoma | 71.2% (64.5%, 78.5%) | 41.2% (34.2%, 49.7%) | 22.7% (16.5%, 31.2%) | |
| Kidney-renal cell carcinoma | 56.3% (48.7%, 65.0%) | 33.7% (26.8%, 42.5%) | 23.1% (16.8%, 31.8%) | |
| Bones/soft tissue-sarcoma | 37.3% (28.3%, 49.4%) | 14.5% (8.57%, 24.4%) | 8.67% (4.19%, 18.0%) | |
| Germ cell-germ cell tumor | 63.6% (46.4%, 87.3%) | 54.5% (37.2%, 79.9%) | 54.5% (37.2%, 79.9%) | |
| Other | 65.0% (58.0%, 72.8%) | 36.3% (29.5%, 44.7%) | 29.8% (23.4%, 38.1%) | |
| Time from primary surgery: | < 0.001 | |||
| < 60 | 46.7% (40.7%, 53.7%) | 18.6% (14.0%, 24.7%) | 6.73% (3.18%, 14.2%) | |
| 60–120 | 66.7% (60.3%, 73.7%) | 38.6% (32.2%, 46.2%) | 23.3% (17.7%, 30.6%) | |
| 120–180 | 73.6% (64.1%, 84.5%) | 50.0% (39.7%, 63.0%) | 43.0% (32.9%, 56.1%) | |
| > 180 | 75.0% (65.1%, 86.4%) | 60.9% (50.1%, 74.1%) | 51.3% (40.4%, 65.2%) | |
| Lymph node metastases: | 0.4 | |||
| Yes | 59.6% (47.1%, 75.4%) | 27.5% (17.3%, 43.8%) | 21.9% (12.4%, 38.5%) | |
| No | 60.8% (56.8%, 65.1%) | 35.3% (31.4%, 39.6%) | 24.6% (21.0%, 28.8%) |
Table II
Multivariate Cox regression results
Discussion
When analyzing the history of surgical treatment of neoplastic lung metastases, it seems that everything has already been said about this issue. Numerous authors in separate studies have determined which parameters may improve treatment outcomes and, consequently, OS. In the present study, PFS after the first metastasectomy was analyzed. This parameter is defined as an alternative surrogate endpoint in relation to OS [8]. An attempt was made to determine the extent to which surgical treatment of pulmonary metastases affects the health outcome and how long it allows for living in relative comfort. At the same time, it should be borne in mind that we are not able to determine what the natural course of the disease would look like. PFS objectively determines the time without feeling sick, which is confirmed by numerous studies. The guiding principle is that the treatment effect observed for an important surrogate endpoint can reliably and accurately predict the effect of this treatment on the clinical endpoint [9]. PFS is a substitute for OS. It is to some extent measurable in the chemotherapy of proliferative disease. Some authors, comparing stereotaxic ablative radiotherapy (SABR) with metastasectomy, did not find any differences in the indicators of local tumor control and OS. However, an improvement in the PFS parameter was described after metastasectomy. In this group 41.6% remained disease-free compared to 11.9% in the SABR group after two years of follow-up [10–12]. Here an attempt was made to investigate the PFS value in surgical treatment. It should be remembered that regardless of the method of treatment, each of them has temporary or, even worse, sometimes permanent effects deteriorating the patient’s well-being. Surgical treatment, similarly to non-surgical oncological methods, has a transiently stronger effect on the deterioration of the patient’s health. Stress related to the procedure, perioperative pain, and reduced overall performance reduce the patient’s quality of life. However, unlike chemotherapy, these symptoms are usually temporary. At the same time, the number of reported complications is small. In our research, the rate was around 7%, of which around 30% were not related to the surgery. The risk of perioperative death in the study group was 0.5% [3, 4]. For the purposes of the present study, the PFS time was defined as the appearance of new lung lesions after metastasectomy or the date of death or the date of completion of the observation assuming that the patient was alive up to that date. It should also be remembered that the exact date of progression is not exactly known. At the time of its diagnosis, it was known that it appeared between the last negative assessment and the next one, when the stage of the disease was reclassified. While death is the absolute endpoint of the study, radiographic progression is a subjective measure prone to read errors [13]. Thus, the PFS resulting from this reading is prone to errors in identifying endpoints called detection errors. Dancey et al. defined 4 progression criteria: the appearance of new radiologically confirmed lesions, an increase in the size of previously observed lesions, a marked increase in symptoms not related to cancer and/or the occurrence of symptoms unrelated to the presence of lung lesions [6, 8]. These doubts are particularly high in cases of non-surgical oncological treatment. This is related to greater difficulties in histological verification of new lesions in the lungs using minimally invasive methods. In the case of surgical resection, it is obvious that the diagnosis can be quickly verified already in the intraoperative examination. The most problematic aspect is establishing whether disease progression is detectable but not measurable (Figure 1). When examining the usefulness of PFS in planning surgical treatment, it was found that it is a valuable parameter. It was established which parameters, already known at the stage of qualification for the procedure, influence its extension. PFS increases with the patient’s age, and is distinctly longer in the presence of metastases in only one of the lungs. The histological type in the method does not require an extension of the progression-free time. In observations of 1, 3, 5 years, PFS did not decrease linearly at the same time for different cancers. The DFI time influenced the PFS parameter, which was clearly visible in the 3- and 5-year periods. Although this parameter will follow the evaluation of the results of chemotherapy treatment, the monitoring of surgical treatment of secondary proliferative disease should be performed.