Summary
Identifying patients in the high-risk group and reducing cardiovascular risk with lifestyle changes and, when necessary, pharmacological treatment is essential. Therefore, this study evaluated the treatment and lifestyle change recommendations given by cardiologists to patients. In the 104 participants included in the analysis, the rate of recommending lifestyle changes, diet, and exercise to patients in cardiology outpatient clinics is very low. SGLT2i and ARNI have become highly regarded drugs in heart failure patients. The rate of achieving the target low-density lipoprotein cholesterol value in patients admitted to the cardiology outpatient clinic needs to be higher.
Introduction
Cardiovascular (CV) diseases are the most common cause of morbidity and mortality worldwide. The increasing average age of the population, irregular and unhealthy diet, inactive life, and widespread smoking are among the main causes of CV diseases [1]. Myocardial infarction (MI), stroke and peripheral arterial diseases (PAD) can be prevented to a great extent by correcting modifiable risk factors in CV diseases. Therefore, the role of cardiologists in primary and secondary prevention is critical [1, 2].
High blood pressure is a major risk factor for coronary artery disease (CAD), heart failure (HF), cerebrovascular disease and PAD. Therefore, in the presence of comorbid diseases, antihypertensive drug selection and lifestyle changes recommended to patients are important [3]. Smoking cessation should be one of the most important goals in primary prevention of CV disease, especially in young people [4]. With regular physical activity, weight decreases, LDL cholesterol (LDL-C) and triglyceride levels decrease, HDL cholesterol (HDL-C) levels increase, insulin sensitivity increases and blood pressure decreases [5]. There is a protective relationship between weekly moderate exercise and CV mortality [5, 6].
Just as it is important to recommend lifestyle changes such as exercise, diet, and smoking cessation to patients in the low-medium-risk group in terms of protection from CVD, it is also important to identify patients in the high-risk group and reduce CV risk with lifestyle changes and, when necessary, pharmacological treatment. Cardiology physicians have important responsibilities in these matters.
Aim
Therefore, this study evaluated the treatment and lifestyle change recommendations given to cardiac patients by cardiologists.
Material and methods
The study targeted cardiologists working in university hospitals, state hospitals, training and research hospitals, private hospitals, and private practices throughout Turkey. In addition, it is a survey study and was conducted prospectively.
In this study, the predetermined questionnaire was shared with cardiologists via e-mail from January 2024 to February 2024 and answered online. One hundred five cardiologists participated in our survey; 104 (99.05%) cardiologists gave consent for the survey results to be used and shared in the analysis.
This questionnaire, consisting of 30 questions about treatment and lifestyle change recommendations given to patients applying to cardiology outpatient clinics, was used to assess the awareness of cardiologists on this issue. Patients included in the study, who were recommended by cardiologists, were patients admitted to cardiology outpatient clinics, older than 18 years, with one or more of the following diagnoses: coronary artery disease, hyperlipidemia, hypertension, diabetes mellitus, arrhythmia, and heart failure. Participants were advised to exclude certain patient groups (unstable patients, active malignancy, disabled patients) from their responses to the survey in order not to influence the study results. Our questionnaire covered topics related to CV prevention, diet, eating habits, lifestyle, diagnosis and treatment strategies for CAD, HF, arrhythmia, and dyslipidemia.
The responses from physicians who voluntarily completed the questionnaire were analyzed through the SurveyMonkey survey research site, which uses an Internet database. The responses of participants who completed the questionnaire but did not approve the use of the data for scientific purposes were excluded from the analysis.
Statistical analysis
The SurveyMonkey statistical analysis program was used to analyze the data. Categorical variables are given as numbers (n) and percentages (%). The program G*Power 3.1.9.7 was used for sample size calculation. The sample size was calculated using Student’s t-test with 80% power, error level α = 0.05, and Cohen (d) effect size = 0.3. Accordingly, completing the study with at least 71 participants was deemed appropriate. Data are presented as mean ± SD for continuous variables and absolute numbers (%) for binary variables. A p-value < 0.05 was considered statistically significant.
Results
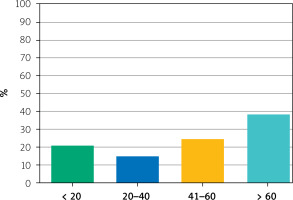
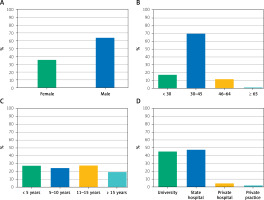
The study included 105 physicians working as specialists in the cardiology units; 104 (99.05%) cardiologists gave consent for the survey results to be used in the analysis and shared. Of the 104 participants included in the analysis, 37 (35.58%) were female, and 67 (64.42%) were male. Eighteen (17.31%) participants were < 30 years old, 73 (70.19%) were between 30 and 45 years old, 12 (11.54%) were between 46 and 65 years old, and 1 (0.96%) was > 65 years old. Twenty (19.23%) of the participants had been working as cardiologists for > 15 years, 29 (27.88%) for 11–15 years, 26 (25.0%) for 5–10 years, and 29 (27.88%) for < 5 years. Forty-seven (45.19%) worked in a university hospital, 50 (48.08%) in a state hospital, 5 (4.81%) in a private hospital, 2 (1.92%) in a private practice (Figure 1). Among the participants, 39 (38.46%) saw more than 60 patients daily in the outpatient clinic, and 22 (21.15%) participants saw fewer than 20 patients (Figure 2).
Figure 1
Demographic characteristics of the participants. A – Gender, B – age, C – professional experience, D – institution
The number of participants who recommended regular exercise to all of their patients was 25 (24.04%), and the number of those who did not recommend it to any of their patients was 3 (2.88%). The majority of the participants did not refer their patients to cardiac rehabilitation programs after acute MI, or they referred very few of them (Table I).
Table 1
Recommendations for lifestyle changes
In this study, 86 (82.69%) of the participants recommended SGLT2 inhibitors to reduce HF-related hospitalization or CV death in patients with HFpEF (HF with preserved EF) and/or HFmrEF (HF with mildly reduced EF). In comparison, 11 (10.58%) did not recommend them and 7 (6.73%) were undecided (Table II). Participants recommended aspirin for primary prophylaxis in patients with moderate to severe CV risk at the rate of 57.69%. The percentage of those who directly recommend coronary angiography to this patient population is 24.04%.
The number of participants who frequently recommended the use of low-dose colchicine (0.5 mg 1 × 1) in patients with ACS who had recurrent CV events while under optimal medical treatment was deficient, at 14 (13.46%). Influenza vaccination was rarely recommended by 39 (37.50%), frequently recommended by 37 (35.58%), and never recommended by 15 (14.42%) of the participants (Table II). One of the study’s striking findings was that the rate of achieving the target LDL-C value was very low, at 3 (2.88%), in patients admitted to the cardiology outpatient clinic. PCSK9 inhibitors were recommended at a low number of 23 (22.12%) in patients using statin + ezetimibe to reach the target LDL-C value (Table III).
Table II
Treatment recommendations
Table III
Risk management
Discussion
Cardiovascular diseases have predispositions and risk factors at behavioral, biological, and social levels. The etiology and pathogenesis of these diseases largely depend on lifestyle. Major risk factors include smoking, lack of physical activity, and unhealthy diet [1–3]. Behavioral risk factors can lead to HT, increased blood sugar and lipid levels, and obesity [4, 5]. Such mediating factors can be controlled within primary prevention. Determining factors also exist at social, economic, and cultural levels, such as urbanization and population aging. Additional risk factors include male gender, poverty, stress, and genetic predisposition [1, 3]. Evidence shows that a large proportion of the burden of CV disease is associated with behavioral factors and that heart disease, stroke and type 2 diabetes can be prevented mainly by mitigating or eliminating these health risk behaviors [7, 8]. Therefore, lifestyle change and treatment recommendations given by cardiologists in the CV center are essential. As a result of our study, it was determined that cardiologists do not currently give enough lifestyle change recommendations to patients. Still the recommendations of the European Cardiology Guidelines are highly followed in terms of medical treatment.
Despite evidence showing that lifestyle change improves health outcomes and reduces health care costs, lifestyle counseling is not routinely implemented in doctors’ clinical practices [9, 10]. Similar to the literature, as a result of our study, a low percentage (24.04%) of the participants recommend exercising to all of their patients.
In the 2023 ESC update for the treatment of ACS, the addition of ezetimibe is recommended with a Class 1 recommendation level if LDL-C targets (LDL-C < 1.4 mmol/l or 55 mg/dl) are not achieved with maximally tolerated statin alone after 4–6 weeks following ACS [9–11]. Initiation of PCSK9 inhibitor treatment is recommended with a Class 1 recommendation level in patients who cannot achieve the LDL-C target (LDL-C < 1.4 mmol/l or 55 mg/dl) despite maximum tolerated statin and ezetimibe treatment [2, 6, 12]. In our study, the majority of the participants, 56.73% (n = 59), did not prefer to give PCSK9 inhibitors to patients using statin + ezetimibe to reach the target LDL-C value. In the ESC 2023 update on the diagnosis and treatment of acute and chronic HF, SGLT-2 inhibitors are recommended with Class 1 (Level of evidence A) to reduce HF-related hospitalization or CV death in patients with symptomatic HFpEF and/or HFmrEF [11]. In our study, most of the participants (82.69%) stated that they would recommended SGLT-2 inhibitors to reduce heart failure-related hospitalization or CV death in patients with HFpEF and/or HFmrEF.
In the ESC 2023 update for the diagnosis and treatment of acute and chronic HF, iron replacement with ferric carboxy maltose or ferric derisomaltose is recommended with Class 2a (Level of evidence A) to reduce HF-related hospitalization in patients with symptomatic HF with reduced EF (HFrEF) or HFmrEF with iron deficiency, while intravenous iron replacement is recommended with Class 1 (Level of evidence A) to improve HF symptoms and improve quality of life in patients with symptomatic HFrEF or HFmrEF [11]. In our study, 51.92% (54) of the participants frequently used intravenous iron carboxymaltose/iron derisomaltose treatment to reduce HF-related hospitalization and improve quality of life in patients with iron deficiency and symptomatic HFrEF or HFmrEF. In the 2023 ESC update on the treatment of ACS, influenza vaccination is recommended in all patients with ACS with Class 1 (Level of evidence A) [2, 13]. In our study, influenza vaccination was routinely recommended by only 9.62% of the participants in patients followed up after ACS.
The main limitations of our study are that it consists of a predominantly young-middle age group (30–45) with professional experience of 11–15 years and a relatively limited number of participants (104 participants). Since the number of participants included in the study was relatively limited, the study’s results cannot be generalized to the whole country. However, this study will provide a foundation for more comprehensive studies on this subject.
Conclusions
The rate of recommending lifestyle changes, diet and exercise to patients in cardiology outpatient clinics is very low. As for medical treatment recommendations, the rate of compliance with the current ESC Guidelines appears to be high. SGLT2i and ARNI have become highly regarded drugs in heart failure patients. One of the study’s most striking findings was that the rate of achieving the target LDL-C value in patients admitted to the cardiology outpatient clinic remains very low.