Introduction
Colorectal cancer (CRC) has become a major public health concern. It is the third most diagnosed cancer and the fourth cause of mortality worldwide. In 2015, 9.4% of all deaths and 5.1% of all disability-adjusted life years (DALYs) were assigned by cancer in the eastern Mediterranean region; also, it accounted for 722,646 new cases, and in 2005–2015 incident cases increased by 46%. It was estimated that 18,662 and 17,150 were diagnosed with CRC in Iranian males and females, respectively [1]. Colorectal cancer is responsible for 764,000 DALYs among Iranian females and males [1]. The proportion of all age DALY counts due to years lived with disability vs. the years of life lost for all ages and both sexes combined for 2016 in Iran was 0.48–0.64, which, in comparison with other countries, was the highest DALY proportion [2]. The 5-year survival rate of CRC in Kurdistan province, an area located west of Iran, was 33% [3].
Evidence-based policy is an important key for local actors to provide and frame the strategies of the health system. The techniques of measuring the magnitude of diseases on a local level may be more productive and functional than on a national or international level because, finally, all of the policymakers want to inform about the situation of diseases in the scene of homogeneity of populations, because organizing strategies for the planning of prevention and control of diseases will be applied at the local level. Therefore, despite the valuable number of studies in the international, regional, and national levels [4, 5], there is an urgent need for that information on a local level, to be the basis for decision-making for the control of diseases. This study is the first report to achieve the incidence rates of CRC among the residents of the local level in Arak, Iran. Arak is a specific area with air pollution from large industrial factories.
In this article, we analysed current CRC statistics in Arak, including the estimated number of new cases in males and females, with age standardized rates (ASRs) and trends for cases diagnosed in 2009–2014.
Material and methods
Arak is the capital of Markazi province, which is located in the centre of Iran. Arak is a major industrial city with several industrial factories, especially for the metal and machinery industries.
In this study the reported cases of CRC incidence from 2009 through 2014 for Arak residents were obtained from the Arak Cancer Registry database, one of 31 cancer registries in the provinces of Iran, which has collected information on cancer in Arak since 2008. The Cancer Registry records the data from private and public clinics, hospitals, and pathological centres. Data derived from the Cancer Registry included age at diagnosis of CRC, gender, and anatomical site of cancer. Colorectal cancer incident cases were extracted from the Cancer Registry records according to cases coded as colon, recto-sigmoid, rectum, anus, and anal canal with the International Classification of Diseases, tenth revision, (ICD-10), C18, C19, C20, and C21, respectively. Because of a possible mistake in the recorded age, these analyses do not include the CRC cases that were younger than 30 years old at the time of diagnosis (n = 30). In the dataset taken from the Arak Cancer Registry, we found that numerous cases had been duplicated; therefore, we screened records by hand searching independently by 2 authors to identify them and remove them from the data. In data cleaning process, the reported records from the Arak Cancer Registry, in several steps, were sorted by family name, and in the following they were sorted by name, and father’s name. At each step, the repeated records were identified and removed from the original dataset.
Population data for Arak to determine the denominators of incidence rates for the age and gender in the study years was obtained from population census data collected by the Statistical Centre of Iran for 2006, 2011, and 2016. We used the average number of the population for years between censuses; according to this, we estimated 2009 and 2010 based on the average of the population in the 2006 and 2011 censuses, and 2011 to 2014 based on the 2011 and 2016 censuses. Obviously, the population number for 2011 was taken according to the 2011 census.
Statistical analysis
We used the direct method to calculate annual ASRs. Age-standardized rates of CRC for the years 2009 to 2014 per 100,000 persons were adjusted to the world standard population [6]. Age standardized rates with efficient interval estimations were calculated by the provided command by Consonni et al. [7] in STATA software. Joinpoint regression analysis was performed on the ASRs for the whole study period, and we calculated annual percentage changes (APC). These analyses were applied separately for males, females, and both genders. The age at diagnosis of CRC was categorized to < 40, 40–49, 50–59, 60–69, 70–79, and [3] 80 years. We performed joinpoint regression analysis using joinpoint statistical software from the surveillance research program of the US National Cancer Institute.
Results
Descriptive results
Table 1 presents the total number of patients diagnosed with CRC and the age and year of diagnosis and topography codes in Arak. From 2009 to 2014, a total of 533 new CRC cases were included. Among these cases, 245 (46%) were females and 288 (54%) were males. The mean age at diagnosis and its standard deviation for CRC were 62.8 and 14.6 years, respectively (range: 30 to 93 years). Among males and females, slightly more CRC cases occurred in those aged 50–59 (23.3%) and 70–79 (24.1%) years, respectively.
Table 1
Number (percent) of cases with colorectal cancer in Arak, 2009–2014, stratified by gender
Age-standardized rates (based on world standard population)
The findings of this study show that the annual ASRs of CRC per 100,000 population in Arak during 2009–2014 is 13.58 (95% CI: 1.9–15.42), 16.52 (95% CI: 14.62–18.60), 15.00 (95% CI: 13.72–16.35) for females, males, and both males and females, respectively (Table 2). During 2009–2014, most of the ASRs were obtained from females (17.9, 95% CI: 13.3–23.4) in 2013, males (20.9, 95% CI: 15.6–27.4) in 2011, and both of them (18.3, 95% CI: 15.0–22.1) in 2013 (Table 2).
Table 2
Age-standardized rate (per 100,000) for colorectal cancer in Arak, 2009–2014
Trends of age-standardized incidence rates (based on the world standard population)
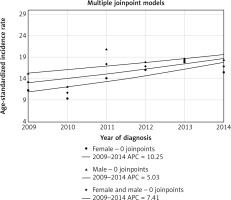
The annual ASRs of CRC during the study period (2009–2014) displayed growing trends among the males and females that were studied (Fig. 1). Females in Arak had an increasing trend in ASRs (APC: 10.25% and 95% CI: –0.79 to 22.53); and a slightly increasing trend was observed among males (APC = 5.03% and 95% CI: –6.14 to 17.53). Among females and males together, ASRs were increased; however, this increasing trend curve lies between the trend curves of female and male (APC: 7.41% and 95% CI: –2.86 to 18.76).
Discussion
In his study, during 2009–2014, the increasing trend of CRC incidence was greater among females than among males in Arak, an industrial area in the centre of Iran. These findings may be of considerable concern, relating to a crucial growing public health problem. Another reason may result from the uncertainty of the data quality related to the cancer registry.
Growing ASRs of CRC may be due to a set of risk factors: nutrition patterns with high amounts of red meat, high-fat foods, high sweetmeat consumption, opium use, insufficient physical activity, obesity, and other risk factors related to the CRC [8]. Any previous comprehensive studies related to the prevalence and patterns of these risk factors have not been conducted in Arak, as addressed them properly. In a study in Isfahan, Najafabad and Arak in 2000–2001 [9], body mass index (BMI) was determined: for females and males it was 26.6 and 24.5 kg/m2, respectively. In accordance with Talaei et al. [10], the prevalence of BMI ł 25 in Arak females and males was 59% and 45%, respectively. High BMI is the second important risk factor contributing to DALYs. In 2013, the proportion of high BMI of DALYs from among all DALYs in the eastern Mediterranean region, including Iranian females and males, were 8.1% and 7.0%, respectively [4]. Gram et al. [11] found that ever-smokers among Norwegian females had a 20% increased risk of CRC (RR = 1.2; 95% CI: 1.0–1.5) compared to never smokers. Therefore, it is clear that the females were more at risk than males for CRC, and the findings of this study also document this. Naghibzadeh-Tahami et al. [8] conducted a case-control study to determine the association between opium use and CRC among residents of Kerman, an area in the south of Iran; the odds of use of opium in CRCs was 4.5 times greater than the odds in the control group.
On the other hand, Arak is an industrial city, with major polluting industries, and most of the residents of Arak are employed in these industries. In different studies, it has been shown that occupational history was associated with CRC incidence and mortality [12, 13]. In a retrospective cohort study conducted in France [14], long-duration occupational asbestos exposure was associated with CRC.
To date, a screening program to detect CRC cases in the early stages has not been conducted in Iran, including Arak. It was recommended to the policymakers to provide screening programs of CRC. Javadinasab et al. [15] identified the most cost-effective strategy for CRC screening in Iranian high-risk individuals. They recommended CRC colonoscopy screening every 10 years in high-risk groups, which is cost-effective in Iran.
It recommended the studies are conducted to identify the risk factors for CRC, especially in Arak, because Arak residents are more differentiated than other areas of Iran, due to the specific air pollution and the occupational exposures.
According to this study, the annual ASRs of CRC for males and females in Arak were 16.52 and 13.58, respectively, that they were higher than the average ASRs in all of Iran. In line with the findings based on the study conducted by Darabi et al. [16], ASRs for males and females in Iran were 11.28 and 10.33 per 100,000 persons in 2010, respectively. Dolatkhah et al. [17] found that the incidence rate of CRC in 2000–2014 in Iran was 8.16 and 6.17 per 100,000 for males and females, respectively. In a study of CRC worldwide, CRC age-adjusted incidence rates in Iranian males in 2012 (according to the world standard population, per 100,000) was in the range 9.0–16.1, while most European countries were in the range > 32.2 [18]. In a similar study conducted in the Fars province of Iran [19], ASRs of colon and rectum cancer in 2007–2010 were 7.49 and 9.57 for females and males, respectively, which is less than for Arak. In comparison, from 1976 to 2005, ASRs CRC in the United States per 100,000 population decreased from 60.5 to 46.4 [20]. Rectal cancer in 1998–2009 in the United States was increasing among younger adults and decreasing among older adults, probably because of the existence of a program of colonoscopy screening [21].
Time trends of the incidence of CRC in France [22] revealed an increased incidence in both males and females, but more for males than females. In comparison, in this study, we found a reverse situation with more for females than males. It possibly returned to the prevalence of different risk factors among two populations. Another issue relates to the better attitude of Iranian females than males about the utilization of health care, which leads to additional attempts to search for a diagnosis of the disease. Furthermore, any increase in the ASRs of CRC may be due to the promotion and improvement in the quality of the Cancer Registry over time.
Some methodological biases exist in this study. By considering the lack of a completely valid cancer registry service in Arak, it may have under-estimated in the incidence of CRC. However, we know that these reported ASRs may be minimum estimations and the real ASRs maybe greater. Also, misclassification in reported ages and identification of the year of diagnosis may be occurring [23], and the authors have not been able to address it. On the other hand, to obtain valid data on the incidence of cancers, it is recommended to promote the quality of the Cancer Registry more than the former.
Conclusions
Generally, our findings showed that the ASRs of CRC in Arak have increased trends in both females and males however, females had a greater increasing trend than males. Age standardized rates of CRC in Arak have been more than ASRs in a number of other areas of Iran. Effective strategies for a screening program for early diagnosis of CRC cases may be required.