Transradial access (TRA) is the recommended approach in guidelines for percutaneous coronary intervention (PCI). Radial artery occlusion (RAO) is one of the most common significant complications following transradial catheterization, with an incidence ranging from 1% to 10% [1].
We describe the case of a 40-year-old patient presenting with typical chest pain, elevated troponin levels, and ST-segment elevation on electrocardiogram. The patient was admitted for urgent coronary angiography (CAG) via right TRA. The radial artery (RA) was punctured and cannulated using a standard 6F sheath and two 6F Judkin’s catheters (Braun, Germany) for the CAG. The angiographic findings revealed no significant atherosclerotic lesions. Post-procedurally, radial artery gauze compression was applied.
Subsequent diagnostic imaging confirmed the diagnosis of acute myocarditis. On the fourth day after CAG, the patient reported pain along the course of the right RA. Doppler ultrasound revealed RAO, with hypoechoic material visible within the lumen of the artery, which was non-compressible, with preserved flow in the ulnar and interosseous arteries. Anticoagulation therapy with therapeutic doses of low-molecular-weight heparin (enoxaparin 70 mg s.c. twice a day) was initiated, alongside analgesic treatment (paracetamol).
On the eighth day of hospitalization, due to persistent severe pain in the right hand, a percutaneous intervention was performed entirely under ultrasound guidance. Despite puncture of the RA, no antegrade flow was observed. Using ultrasound (Fujifilm SonoSite SII, high-frequency linear probe), a coronary guidewire (Hi-Torque Pilot 50) was successfully advanced into the right brachial artery. Multilevel balloon angioplasty (Boston Scientific Emerge 3.0/20 mm) was performed with ultrasound visualization. The procedure restored spontaneous outflow at the puncture site and improved flow on color Doppler (CD) imaging (Figure 1).
Figure 1
Ultrasound-guided balloon angioplasty of the occluded right radial artery. A – Guidewire advanced into the occluded radial artery, with the distal tip reaching the brachial artery; good blood flow is observed in the ulnar artery on color Doppler. B – Multilevel balloon dilatations performed in the radial artery under real-time ultrasound guidance. C – Restoration of adequate blood flow in the radial artery immediately following percutaneous intervention, confirmed by color Doppler imaging. D – Sustained patency of the radial artery observed at 1-month follow-up, with Doppler imaging showing preserved flow dynamics
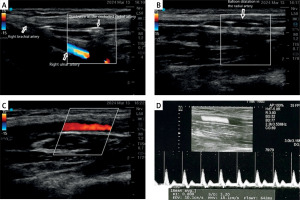
The following day, the RA pulse was well-palpable, and the patient was transitioned to oral anticoagulation therapy (apixaban 5 mg twice daily). The patient reported complete resolution of the pain. Follow-up CD ultrasound 4 weeks later demonstrated adequate flow in the RA.
Currently, no randomized controlled trials provide evidence-based guidelines for the treatment of RAO. However, several investigators have described successful management of RAO with percutaneous transluminal balloon angioplasty performed via puncture of the distal RA (anatomical snuffbox) using the Seldinger technique and the insertion of a 5F radial introducer sheath [2]. The addition of antithrombotic therapy for 3 months has also been shown to promote the safe restoration of RA patency [3]. Ultrasound-guided larger diameter artery access is associated with a lower incidence of vascular complications [4].
This case demonstrates that percutaneous transluminal balloon angioplasty, performed entirely under ultrasound guidance, is a feasible and effective approach for the management of RAO. Real-time ultrasound visualization enhances procedural safety and guidewire navigation, making it a valuable technique in cases requiring revascularization. Given the lack of standardized RAO treatment guidelines, further studies should evaluate the long-term outcomes of this approach.








