Introduction
Cervical cancer treatment has always represented a challenge for surgeons, radiotherapists, radiologists and medical oncologists [1]. It is the twelfth most frequent cancer in women in developed countries, and patients may experience changes in their sexual functioning and quality of life resulting from the cancer itself and its treatment [2]. If on the one hand surgery and adjuvant radio- and chemotherapy are able to be curative in the majority of cases at the early stage, on the other hand the young age of affected women determines the exposure of patients to the long-term consequences of treatments, affecting health and different aspects of the quality of life, which can be disrupted by urinary, gastrointestinal, neurologic, reproductive, and sexual side effects primarily related to surgery and radiotherapy [3]. The purpose of the surgical treatment, is that of removing, with the exception of microinvasion, beside the cervix the connective tissue around it and the upper vagina, known as paracolpos or paracolpium, with or without lymphadenectomy in a measure progressively greater depending on the size, aggressiveness of the tumor and lymph node status [1, 4, 5]. Preoperative conization plays a potentially protective role in patients with an IB1 tumor [6].
Such connective tissue in the present paper is called in general parametrium, which may not be anatomically correct, but since this term has gained an unreplaceable place in the mind of most gynecologic surgeons, the Authors continue to use it in its extensive meaning. At the same time it is important to precise that according to the Terminologia Anatomica [7] the term parametrium should be referred to the cranial portion (above the ureter) of the cardinal ligament (unofficial term), instead paracervix should be related to the caudal portion (below the ureter) of the same ligament.
The reason to extend the resection to the surrounding parametrium is based on the fact that the more voluminous and poor differentiated is the tumor, the higher is the chance that the tissue around the cervix and upper vagina is infiltrated by neoplastic cells [1].
In order to define and standardize the limit of such a resection in relationship with tumor grade and stage, clinicians had to balance the risks of surgery with the necessity to excise an amount of parametrium adequate to ensure clear margins (> 3 mm) [8].
Based on the amount of resected parametrium various classes of radical hysterectomy have been developed, from the old Piver-Rutlege-Smith [9] to the most recent Querleu-Morrow classification [10]. Recent recommended clinical indications [1] for such operations are reported in Table 1.
Table 1
Indications for different classes of radical hysterectomy – Guidelines 2018 European Society of Gynaecological Oncology
The description of radical hysterectomy given in the current literature is more or less directed to surgeons specialized in gynecologic oncology. The authors wanted to evaluate whether adding specific educational materials (medical illustrations created ad hoc) to the reading comprehension of the latest Querleu-Morrow Classification of radical hysterectomy [11] may help Ob/Gyn residents and general Ob/Gyn attendees to better understand the limits of parametrial resection in radical hysterectomy from type A to type C2.
Material and methods
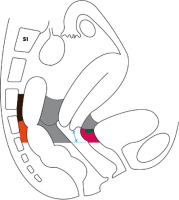
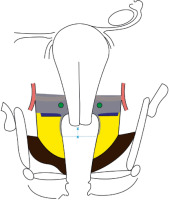
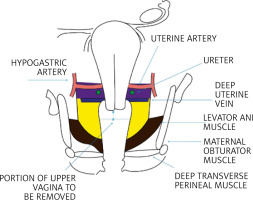
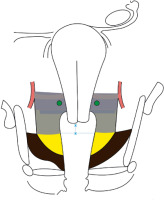
On the basis of the necessary anatomical premises (see Appendix 2), the authors asked a medical illustrator to prepare two schematic topographic pictures of the female pelvis (Fig. 1, 2), where ideally all sub-peritoneal spaces are dissected and all parametrium components, dorsal (posterior), ventral (anterior) and lateral (paracervix), are represented and differentiated from each other using a color code for each of them.
Fig. 1
Schematic representation of dorsal and ventral parametrium in a paramedian sagittal section of the female pelvis (imagined after dissection of all subperitoneal spaces and going approximately through one of the bladder pillars and the omolateral uterosacral ligament)
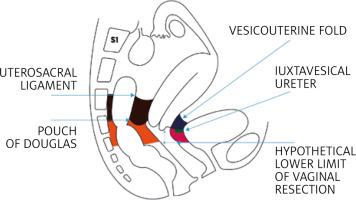
Fig. 2
Schematic representation of lateral parametrium (both sides) in a coronal section of the female pelvis going through the crossing of the uterine artery with the ureter (imagined after dissection of all subperitoneal spaces with the uterus placed in upward traction)
The extent of parametrial resection which characterizes each type of radical hysterectomy taking into consideration A, B1 and B2, C1 and C2, according to the latest Querleu-Morrow classification of radical hysterectomy [11], is indicated in Figures 3–10 by coloring in gray the corresponding portions of ventral, dorsal and lateral parametrium, which needs to be removed.
Fig. 3
Limits of resection of the dorsal and ventral parametrium in type A radical hysterectomy (the area of parametrium to be excised is colored in grey, the dissection of the Okabayashi space is not necessary)
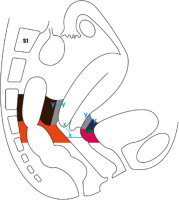
Fig. 4
Limits of resection of the lateral parametrium (paracervix) in type A radical hysterectomy (the area of parametrium to be excised is colored in grey)
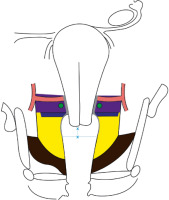
Fig. 5
Limits of resection of the dorsal and ventral parametrium in type B1 and B2 radical hysterectomy. Approximately half of the dorso-ventral length of the dorsal (except sacral attachments) and ventral parametrium (only upper portion) should be removed
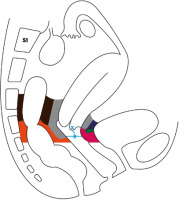
Fig. 6
Limits of resection of the lateral parametrium (paracervix) in type B1 and B2 radical hysterectomy
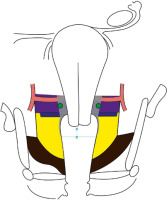
Fig. 9
Limits of resection of the dorsal and ventral parametrium in type C2 radical hysterectomy (the area of parametrium to be excised is colored in grey, the dissection of the medial pararettal space, Okabayashi space, is omitted)
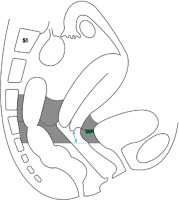
Fig. 10
Limits of resection of the lateral parametrium (paracervix) in type C2 radical hysterectomy (the area of parametrium to be excised is colored in grey)
In order to establish whether these 10 drawing (Fig. 1–10) may have didactic value, 30 senior Ob/Gyn residents and 30 general Ob/Gyn attending physicians were enrolled as participants in a randomized controlled trial. The participants were randomly allotted two groups, each made up of an equal number of residents and attending physicians, defined as group A and group B. The recruitment and randomization process required 2 months, from July 1st to August 30, 2020.
The group A participants were emailed a letter (see Appendix 1) with only a copy of the article) [11] attached for reading comprehension, while the group B participants received, beside the copy of the article, the 10 unpublished medical illustrations prepared on the basis of the article, as a supposed didactic aid.
A brief review of the pertinent pelvic anatomy provided by the authors for prompt consultation (see Appendix 2) was also attached to the email sent to both groups.
The level of understanding of parametrectomy limits in various types of radical hysterectomy was tested in both groups by asking the participants to rate their self-perceived comprehension on a numeric scale graduated from 0 to 10, attached to the emails (see Appendix 1) sent to both groups.
It is true that in general the level of comprehension in students is tested by administering them multiple choice questionnaires on specific subjects [12] whereas a VAS (visual analog scale) is generally used to self-assess pain [13] and/or to measure anxiety or pruritus [14, 15]. However, there are examples in the literature where a VAS has been used for self-assessment of a specific subject understanding [16–18].
Each study participant, after filling out the scale (see Appendix 1), was invited to send it back to the authors within two months from its receipt (sometimes a telephone call, about ten days before the end of the allowed period, was made to solicit an answer). All answers were received by October 30th 2020. Furthermore, in order to compare results also between homogeneous categories of participants group A was divided into 2 subgroups, identified as subgroup Ar (made only by senior Ob/Gyn residents) and subgroup Aa (made only by general Ob/Gyn attending physicians), and similarly group B was divided into subgroup Br and subgroup Ba. The data obtained were statistically analyzed using U Mann-Whitney test. The level of statistical significance was defined by a p value ≤ 0.01 with a 99% confidence interval.
Results
All the recruited participants adhered to the protocol and mailed their answer to the authors within the allowed month.
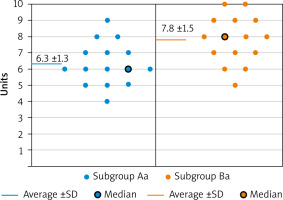
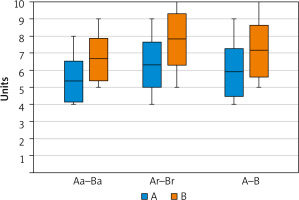
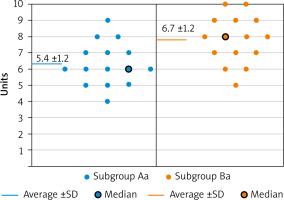
The numeric analogue scale scores, obtained by each participant in the study, are reported for every different subgroup in Figures 11 and 12. As shown in Figure 13 and Table 2, the average understanding value for both attending physicians (5.4 ±1.2) and residents (6.3 ±1.3) is significantly lower (p < 0.01) in subgroups Aa and Ar compared with that in subgroups Ba (6.7 ±1.2) and Br (7.8 ±1.5). Similarly the cumulative average score of residents and attending physicians, taken together, seen in group A (5.9 ±1.4) is also significantly lower (p < 0.01), than that found in group B (7.2 ±1.5).
Fig. 11
Scores distribution and comparison between the 2 subgroups of Obstetrics and Gynecology attending physicians
Discussion
Procedures such as radical hysterectomy today are generally performed by gynecologic surgeons trained in gynecologic oncology, and therefore such didactic illustrations may be seen as redundant and superfluous in certain environments; however, considering that parametrectomy is the main cause of postoperative complications [1, 19], both the general Ob/Gyn attending physicians and the Ob/Gyn residents often deal with the patient in the immediate and/or subsequent postoperative period, and that, sometimes, the patient returns to them for clinical follow-up, the authors think that the 2 aforementioned professional figures deserve a clearer comprehension of the postoperative clinical implications correlated with the extent of parametrium removal which characterizes each type of radical hysterectomy.
Undoubtedly the results of this study show that adding the 10 graphs to the simple reading of the article on the classification of radical hysterectomy [11] ameliorates significantly the level of comprehension of parametrectomy extent in both residents and general attending physicians and this seems to, somehow, fulfil the author’s study objective.
Nevertheless, the authors are aware that the present study has a few limitations, such as the limited number of participants, the fact that the drawings are based on their interpretation of Querleu’s article, and that, in other words, the illustrations proposed, even if considered as faithful to the text, are not validated by the article’s authors, and, last but not least, the difficulty to objectively measure the level of understanding of the participants, measured simply based on a numeric analogous scale score.
Furthermore, the study has at least 2 forms of bias. The first, more important one is that the self-perceived understanding of parametrectomy limits measured in both groups of participants with the visual analog scale does not necessarily reflect a real improvement in comprehension. The truth of the matter is that this type of understanding is hard to test: even all the correct answers to a hypothetical multiple choice questionnaire do not guarantee a real understanding of this specific subject; the authors think that this particular type of comprehension probably could be better verified only by an expert gynecologic oncology surgeon either in the operating room or in the cadaver dissection room.
The other bias, less relevant, is that an improvement in comprehension is in general expected when the amount of educational material on a specific subject is increased. However, such improvement is not automatically achieved and sometimes the added educational resource not only does not ameliorate comprehension, but it even has a detrimental effect on it.
Despite the aforesaid confounders and bias, the authors maintain that their results may, at least, encourage and stimulate future and better didactic efforts in the direction of making the anatomical and functional meaning of parametrectomy and its clinical relevance (in relation to the various classes of radicality) more understandable for general gynecologists or future professionals, not necessarily going to specialize in gynecologic oncology.
Conclusions
The authors, on the basis of the appreciation expressed by residents and attending physicians for their didactic initiative, think that the improvement in knowledge triggered by the graphs will positively affect patient care and that further simplified educational models, either two- or three-dimensional, should be developed in the near future to better serve this purpose. Further illustrations like those presented could be used by clinicians at the time of informed consent to give also patients affected by cervical cancers a better idea of the type of surgery which they will undergo.