Recently, there has been a rise in thoracic empyema in the pediatric population [1]. The uniportal video-assisted thoracoscopic surgery (U-VATS) for chronic empyema in adult patients has been advantageous as it is associated with less pain, faster recovery and better cosmetic results [2]. However, the role of U-VATS in pediatric patients below 3 years old is still anecdotal and less reported to date. Likewise, one-lung ventilation (OLV) in infants and young children is not unknown, but challenging, as the advantages of respiratory mechanics while positioned in lateral decubitus, as seen in adults, are absent in this age group [3]. Although OLV is described in children for video-assisted thoracoscopic surgery (VATS), experience and reports with U-VATS are scarce. We present a case of chronic empyema with lung abscess in a 2-year-old pediatric patient managed with U-VATS under general anaesthesia employing OLV.
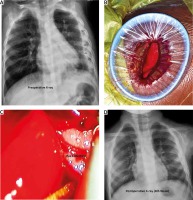
A 2-year-old boy presented with dyspnea, fever, and cough for 4 weeks. On examination, he was tachypneic (35/minute) with room air SpO2 92%, heart rate 145/minute, and blood pressure 70/50 mm Hg. A chest X-ray showed consolidation with a loculated collection of the left lung (Figure 1). He was admitted to the intensive care unit (ICU) and started on empirical antibiotic treatment, which was changed later based on culture and sensitivity. Ultrasound chest was suggestive of the diffuse multiloculated collection; aspiration revealed minimal pus. However, fever and overall condition did not improve, and U-VATS decortication under general anaesthesia (GA) was planned.
Figure 1
Preoperative chest X-ray showing loculated collection and left lung compression (A), surgical incision for U-VATS with wound protector in-situ (B), pus collection seen through endoscope (C), and expanded lung in postoperative chest X-ray (D)
With informed consent from the parent, the boy was taken under GA with OLV using single-use polyvinyl single-lumen, un-cuffed, an endotracheal tube of size 4 mm ID, intentionally progressed to the right endobronchial position. The tube position was confirmed using fibreoptic bronchoscopy. OLV was instituted and the patient positioned on the right lateral side. The diaphragm was marked according to the ultrasonographic appearance of a subpulmonic area before the incision.
A 2.5 cm muscle splitting incision was placed on the 5th intercostal space between the mid-axillary and posterior-axillary line. A pediatric wound protector was inserted, followed by a 5 mm 30° camera at the posterior aspect of the incision. Intraoperatively, an abscess over the superior segment of the left lower lobe was detected incidentally. A harmonic device was used to rupture the loculi, debridement was performed, and adhesions were lysed. Residual debris was removed using a forester sponge holding forceps. Parietal and visceral pleurectomy was done, and the lung was mobilized completely. Lung parenchyma was tested for air leak, followed by a single drain placed at the level of the diaphragm with its tip directed towards the apex. Port-site local anaesthetic infiltration was done, and the patient was reversed and extubated on the table. Intraoperatively, the patient was hemodynamically stable. However, desaturation up to 88% was noted, which was managed with 100% oxygen, and 3-cm H2O positive end-expiratory pressure; SpO2 was maintained within 92-94% after that. The postoperative course was uneventful; the chest drain was removed on postoperative day 3. Chest X-ray showed good lung expansion, and the child was symptom-free. Four weeks’ follow-up was uneventful with good lung expansion (Figure 1). Histopathology for pleura was suggestive of non-specific pleuritis. GeneXpert did not reveal Mycobacterium tuberculosis.
The present case shows the feasibility and safety of U-VATS for empyema in a 2-year-old child. However, the case had challenges from both anaesthesia and surgical viewpoints. Although double-lumen tube (DLT) is the gold standard for lung isolation, the appropriate size DLT for a 2-year-old child is not available, and the same is true of the univent tube. Further, an uncuffed tube has a risk of an improper seal, contrary to a cuffed tube, which has a risk of blocking the right upper lobe ventilation. Lung mechanics in infants and young children are also not favorable in the lateral position due to softer chest walls and relatively higher diaphragmatic positions [3, 4]. All these factors make OLV in young children challenging. Information on OLV for U-VATS in such young children is also scarce or missing.
The open thoracotomy leads to significant morbidity in a pediatric patient. Development of thoracic musculoskeletal and nervous structures during the first two years of life is crucial, and open thoracotomy carries the risk of developing scoliosis, winging of the scapula and muscular weakness. On the other hand, using traditional VATS bimanual instrumentation, nullifying the torsional angle is not possible [5]. U-VATS has a significant advantage regarding these aspects. Nevertheless, the learning curve is steep, and it is necessary to have good knowledge of the anatomical characteristics of the chest as the morphology of the pediatric chest changes with age [4]. Hence various morphological characteristics have to be acknowledged before an incision, and pre-incision ultrasound helped us delineate the diaphragmatic position.
U-VATS is an emerging technique, and knowledge, especially in the pediatric population, is minimal. It makes U-VATS in young children a challenging task. In 2004 Rocco et al. described this technique for diagnostic procedures and pneumothorax in adults [6]. Gonzalez-Rivas et al. in 2011 applied this technique for anatomical lung resection in adults, which bought a new evolution in the field of thoracic surgery [7]. Aragon et al. reported the first experience in U-VATS in an 11-year old male patient [8]. Later Fernandez-Pineda et al., 2019, described their experience with modified U-VATS in 11 children with pulmonary nodules [9]. Recently, U-VATS has been used in various complex thoracic procedures in pediatric patients, primarily across advanced countries and set-ups with success. Recent literature shows a satisfactory result for U-VATS, even for stage III empyema in adult patients [10]. We believe that the successful and safe management of OLV using a single-lumen tube for U-VATS in a 2-year-old with chronic empyema stage III will further boost the use of this technique.
In conclusion, surgical treatment of stage-III empyema by U-VATS technique using OLV in a 2-year-old is a challenge but feasible and safe.






