Synovial chondromatosis is a rare benign disorder characterized by proliferation of cartilaginous nodules within the synovial lining of joints, tendon sheaths, or bursae. While it primarily affects large joints such as the knee, hip, and elbow, its occurrence in smaller joints is uncommon. Synovial chondromatosis involving the sternoclavicular joint, particularly in elderly patients, is exceedingly rare [1]. Herein, we present an uncommon case of an 89-year-old female patient diagnosed with synovial chondromatosis affecting the sternoclavicular joint, emphasizing the diagnostic challenges, therapeutic strategies, and favorable postoperative outcomes. To our knowledge, this is only the second documented case worldwide of synovial chondromatosis localized within this joint. Through a comprehensive review of the literature, we identified a single case involving a 9-year-old patient with a similar anatomical presentation [2].
An 89-year-old female patient presented with dyspnea, fever, and a progressively enlarging mass in the right neck region over a 6-month duration. Imaging studies revealed a cystic mass adjacent to the right sternoclavicular joint, demonstrating connection to the joint space along with joint space expansion and adjacent degenerative changes. Computed tomography (CT) and magnetic resonance imaging (MRI) characterized the mass as a smooth-edged lesion exhibiting T2 hyperintensity and T1 hypointensity, initially suggestive of a ganglion cyst (Figures 1, 2). It is important to note that a preoperative biopsy or histological examination was not conducted in this case. After extensive discussion with our radiology team and considering the imaging findings, the lesion was strongly presumed to be a ganglion cyst of the sternoclavicular joint. This assumption guided our approach, as a biopsy was not judged necessary preoperatively. Surgical resection was deemed necessary due to symptom progression and the size of the mass. Intraoperatively, a substantial cystic formation infiltrating the right sternoclavicular joint was observed, necessitating en bloc resection of the mass along with part of the first rib (Figure 3). Postoperatively, the patient’s cardiac complications were managed pharmacologically with medications including amiodarone, apixaban, and diuretics. Histopathological examination revealed marked degenerative cartilage proliferation with extensive calcium pyrophosphate deposits involving the manubrium sterni, first rib, and clavicle, establishing the diagnosis of synovial chondromatosis. The patient exhibited favorable postoperative recovery and was discharged with a healed wound on the 19th postoperative day. Subsequent follow-up assessments at 1 week and 1 month revealed no abnormalities.
Figure 1
MRI images depicting the mass in the sternoclavicular joint (arrow) using T1 and T2 sequences. A, B – Coronary reconstructions. C, F – Transverse images. D, E – Sagittal reconstructions

Figure 2
Computed tomography images reveal the mass in the sternoclavicular joint (arrow). A, B – Transverse images. C – Coronary reconstruction. D, E – Sagittal reconstructions
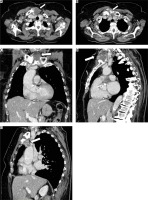
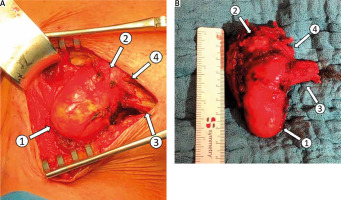
Figure 3
Intraoperative visualization of synovial chondromatosis in the sternoclavicular joint. A – In situ exposure of the mass. B – En bloc resected specimen. Labels: (1) mass formation, (2) manubrium of sternum, (3) clavicle, (4) first rib
Synovial chondromatosis of the sternoclavicular joint is extremely rare and presents a unique diagnostic challenge, as it can mimic malignancies and other serious conditions [3]. The etiology of synovial chondromatosis is not fully understood, but it is thought to result from metaplasia of synovial cells or mesenchymal transformation within the synovium. Some cases are associated with joint pathologies such as osteoarthritis or trauma, while others appear sporadically [1]. The disease typically progresses through three phases: an active synovial phase, a transitional phase with free cartilaginous nodules, and a metaplastic phase characterized by calcified nodules within the joint, potentially causing pain and restricted movement [1].
Common clinical features include joint pain, swelling, and limited motion. Although synovial chondromatosis usually affects larger, weight-bearing joints, it occasionally involves smaller joints such as the sternoclavicular joint [4]. Diagnosis relies on clinical assessment, imaging (CT, MRI), and histopathological examination [5]. In this case, initial imaging suggested a ganglion cyst, with MRI findings further complicating the diagnosis. Post-surgery histopathology confirmed extensive synovial chondromatosis affecting the manubrium, first rib, and clavicle, with degenerative cartilage proliferation and calcium pyrophosphate deposits.
Although generally benign, untreated synovial chondromatosis may cause significant joint dysfunction. Prompt surgical intervention successfully managed the condition in this case, though cardiac comorbidities demonstrated the importance of a multidisciplinary approach. The patient’s positive recovery illustrates the effectiveness of timely intervention, particularly in unusual joint locations.
This case highlights synovial chondromatosis as a rare cause of sternoclavicular joint pathology, presenting unique diagnostic challenges due to its unusual location. Although benign, the condition’s rarity can lead to diagnostic misinterpretations. Successful treatment in this case underlines the value of clinical judgment, interdisciplinary collaboration, and awareness of atypical joint pathologies.






