Introduction
Complex coronary multi-vessel disease patients often pose difficult therapeutic decisions in terms of modality of revascularisation (complex percutaneous coronary interventions (PCI) versus coronary artery bypass grafts (CABG)). One of the most important elements included in heart team treatment algorithms is the SYNTAX Score (SS) (which received a class I, Level of Evidence A indication in the 2018 ESC/EACTS Guidelines on myocardial revascularisation) [1].
The SYNTAX Score is an algorithm computing coronary atherosclerotic burden [2]. Its main purpose is to help the heart team make an evidence-based therapeutic decision. A severity score is assigned to each segment of the coronary artery corresponding to the quantity of myocardial muscle at risk.
The above guidelines stated that in the cohort of the SYNTAX study and (subsequently) in external validation cohorts, the SS was found to be an independent predictor of long-term major adverse cardiac and cerebrovascular events and of death in patients treated with PCI but not with CABG [3, 4]. However, the papers quoted do not take into account other studies demonstrating the long-term prognostic power of SS in CABG-treated patients [5, 6].
Two recent ESC papers (the 2018 Fourth universal definition of myocardial infarction and the ESC Joint Working Groups on Cardiovascular Surgery position paper) [7, 8] have established a new definition for type 5 myocardial infarction (post-CABG MI), which requires a cardiac troponin (cTn) cut-off > 10 times the 99th percentile upper rate limit (URL) values. At the same time, both documents state that marked isolated elevation of cTn values within the 48 hours post-operative period, even in the absence of electrocardiographic/angiographic or other imaging evidence of MI, indicates prognostically significant cardiac procedural myocardial injury [4, 9, 10]. In addition, important studies showed that early rise of cardiac biomarkers after cardiac surgery was independently associated with death [11–13]. In a similar clinical setting, heart-type fatty acid binding protein (hFABP) peaked earlier and proved to be a superior independent predictor of postoperative mortality in comparison with traditional markers of myocardial injury (cTnI and creatine kinase-MB – CK-MB) [14, 15].
Aim
To date, there are no data exploring the relationship between the complexity of coronary atherosclerotic burden (e.g. SS) and early myocardial injury after CABG. Therefore, we sought to analyse the correlations and predictive strength of SS for early myocardial injury after on-pump CABG (rise of CK-MB, cTnI or hFABP). If confirmed, SS could become a simple and efficient indicator for post-operative major adverse cardiac and cerebrovascular events (MACCE).
Material and methods
Study population and inclusion criteria
Between May 2015 and May 2017, one hundred and twenty consecutive patients undergoing elective CABG surgery in the Cardiovascular Diseases Institute from Iasi, Romania, were included in our analysis. All patients over 18 years of age scheduled for elective surgery were eligible for the study. Exclusion criteria were: 1) emergency/off-pump CABG, 2) prior heart surgery, 3) concurrent valve surgery or aneurysmectomy, 4) prior myocardial infarction within the last 2 weeks, 5) severe coagulation abnormalities, 6) other concomitant procedures (MAZE procedure, tumours, pulmonary vein isolation). The time interval between coronary angiography and CABG was less than 90 days in all patients.
The surgery technique was decided by cardiac surgeons. The following variables were assessed: age, sex, cardiovascular risk factors (diabetes mellitus, arterial hypertension, chronic kidney disease), presence of heart failure assessed according to the New York Heart Association (NYHA), peripheral arterial disease, findings obtained in the preoperative transthoracic echocardiogram and coronary angiography. Laboratory tests analysed routine haematological and biochemical parameters (lipid panel, coagulation, inflammatory profile, renal and liver function). A post-operative echocardiographic evaluation was performed. All subjects agreed and signed an informed consent form. The study was approved by the “Grigore T. Popa” Iasi University Ethics Committee and was conducted according to the Declaration of Helsinki. No sex-based or racial/ethnic-based differences were present.
SYNTAX score
The score calculator and therapeutic indications are available on the SS website (www.syntaxscore.com). Our analysis was performed retrospectively by two independent operators. Every significant inter-observer difference required a recalculation.
Cardiac biomarkers
We analysed myocardial injury related to CABG using 3 cardiac biochemical markers (CK-MB, cTn-I and hFABP). hFABP is a small cytosolic protein (15 kDa) rapidly released in the circulation when membrane integrity is affected in response to cardiac ischaemia [16]. A sample of venous blood was obtained from the subjects at 6 hours after aortic unclamping. The cut-off value in early myocardial injury for hFABP was 6 ng/l, as previously described in other studies [17, 18]. Moreover, the cut-off levels for CK-MB (25 UI/l) and cTn I (0.01 ng/ml) were chosen according to the guidelines for acute myocardial infarction [7]. The serum time to peak is shortest for the hFABP assay, with early rise specificity (6 hours, compared to 14–18 hours for cTn-I and 9–24 hours for CK-MB), although serum levels increase as early as 30 minutes for hFABP (3–6 hours for cTn-I, 3–8 hours for CK-MB). Amongst the three cardiac markers, hFABP has the shortest half-life, returning to normal within 24 h [19].
Surgical procedure
The majority (99%) of patients underwent on-pump bypass surgery (according to the internal protocol) by means of aorto-atrial cannulation and systemic hypothermia. The pump flows were fixed to maintain a cardiac index of more than 2.4 l/min/m2. Myocardial protection was attained by intermittent antegrade administration of a hypothermic, St. Thomas’ II cardioplegic solution. Pump circuit was primed with Ringer solution, heparin and mannitol. Any artery with an obstruction of more than 80% in the coronary angiography was grafted at the surgeon’s convenience. Complete revascularisation was intended in all patients. Since the bilateral internal mammary artery (IMA) and radial artery for non-LAD targets have been shown to provide better patency rates than saphenous veins [20], particularly for the left coronary artery system, we used only arteries as coronary grafts: left IMA, right IMA and radial artery.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation and categorical data as number with percent frequency. Normality of variables’ distribution was checked with the Shapiro-Wilk test. Independent t test and 1-way ANOVA were performed for continuous variable comparisons. Nominal data were compared using the χ2 test. Stepwise multivariate linear regression analysis was performed to evaluate independent variables correlated with hFABP, cTn I and CK-MB. Statistical analyses were performed with SPSS 20.0 (IBM since version 19.0) and MedCalc (MedCalc Software bvba, Belgium). A two-tailed p-value < 0.05 was considered significant.
Results
From 149 patients screened, 120 patients entered in the final analysis (8 could not provide signed informed consent, 11 had improper echo acquisitions, 10 with missing data). The mean age was 65.93 ±9.83; 91 were male (75.2%); 60.3% (n = 73) were smokers and 98.3% (n = 111) were hypertensive patients. In the hypertensive group, 90% of patients were identified with moderate left ventricular concentric hypertrophy, with a mean left ventricular mass index of 143.31 ±46.40 g/m2.
The majority of patients had at least a form of atherosclerotic disease, 62.8% (n = 76) having a history of MI, 2.9% of peripheral arterial disease, and 5% of stroke. The mean body mass index (BMI) was 29.4 ±3.02 kg/m2, 52.1% (n = 63) were diabetics, with a mean glycemia of 138.53 ±57.43mg/dl, and total cholesterol of 181.54 ±46.33 mg/dl. Eighty-one patients were admitted with NYHA class ≥ II (67%) and had a mean left ventricular ejection fraction (LVEF) of 43.47 ±7.32%.
After coronary angiography assessment, the mean SYNTAX score was 30.43 ±3.4. After surgical myocardial revascularisation, early myocardial injury (defined as elevation of the serum cardiac biomarkers over the established thresholds) was detected in 97% of patients. The mean for hFABP was 68.5 ±46.1 ng/ml, for troponin I was 0.75 ±0.3 ng/ml, and for CK-MB was 26.5 ±2.17 UI/l.
All the baseline characteristics of the studied population are included in Table I.
Table I
Descriptive statistics of the study population
In our study population we identified only two (out of 120 patients) acute early graft failures (needing reintervention/angioplasty). Due to the lack of transit time flow measurement (TTFM) device, and to logistical and infectious reasons (we could not transfer the patients to angio-CT in the first 6–12 hours after CABG), we considered a graft failure in a patient with haemodynamic instability and high necrosis troponins/CK-MB).
Postoperative complications were as follows: atrial fibrillation/atrial flutter occurred in 23 (19.1%) patients, with a peak incidence on the second and third postoperative days, 9 (7.5%) patients developed renal dysfunction (1 patient required dialysis), 28 (23.3%) patients developed pericardial effusion (2 patients developed a large effusion requiring emergency reopening of the median sternotomy).
Using linear regression model and univariate generalized linear model we assessed multiple variables for clinical prediction of myocardial injury (Table II). In the univariate analysis were the following variables: age, gender, BMI, smoking, MI, left ventricular mass index, history of peripheral arterial disease, history of stroke, diabetes, creatinine clearance, LVEF, and SYNTAX score.
Table II
Predictors of myocardial injury by univariate analysis of the study population
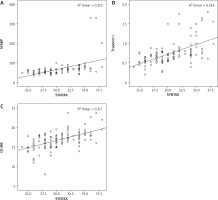
The most significant predictor for myocardial injury was the SYNTAX score, being strongly correlated with the rise of all three cardiac biomarkers (p < 0.001, OR = 66.36, 95% CI: 4.17–8.55 for hFABP, p < 0.001, OR = 0.05, 95% CI: 0.037–0.063 for troponin I, and p < 0.01, OR = 0.21, 95% CI: 0.105–0.325 for CK-MB) (Figure 1). Hypertension was associated only with the rise of hFABP (p < 0.017, OR = 26.28, 95% CI: 4.76–47.81) and was weakly associated with troponin I (p < 0.06, OR = 0.19, 95% CI: 0.05–0.33). Creatinine clearance was strongly correlated with hFABP (p < 0.02, OR = 0.60, 95% CI: 0.09–0.91) and troponin I (p < 0.02, OR = 0.01, 95% CI: 0.002–0.03).
Figure 1
Graphical representation of univariate analysis of SYNTAX score and hFABP (A), troponin I (B) and CK-MB (C) by linear regression models. P-values for all, 0.001. OR = 5.79, 6.49 and 0.844 respectively
A multivariate analysis was conducted including all significant pre-operative clinical/paraclinical predictors from univariate correlations, except hypertension due to its high prevalence and lack of homogeneity among the studied population (which could affect the outcome of the multivariate analysis). After the adjustment of all clinical variables, SYNTAX score remained an independent predictor for myocardial injury, being strongly associated with the rise of hFABP (p < 0.001, OR = 5.79, 95% CI: 3.59–7.98) and troponin I (p < 0.001, OR = 6.49, 95% CI: 4.78–8.20), but not with CK-MB (95% CI: 0.61–1.07) (Table III).
Table III
Independent predictors of myocardial injury after multivariate analysis
Discussion
To our knowledge, this study is the first one to demonstrate a strong connection between a higher SYNTAX score and early myocardial injury after on-pump CABG.
Since all patients received CABG, the SS was situated in the highest tertile category (values over 26) [21], a validating element for our cohort. Having in mind the “window” between 1 and 10 times the 99th percentile URL values (which means between “normal” values and “type 5 MI”cut-off), we do not refer to myocardial infarction after CABG, but to myocardial injury (7), which seems to be an important predictor of post-operative major cardiovascular events [8, 22].
Recently, ESC Joint Working Groups on Cardiovascular Surgery and the Cellular Biology of the Heart released a position paper on Peri-operative myocardial injury and infarction in patients undergoing CABG (7) acknowledging that “[…] isolated elevations of cardiac biomarkers below MI thresholds […] may still be clinically relevant and prognostically significant.”
Apparently, this event of myocardial injury occurs due to a great number of causes different from obvious graft failure or significant ischaemic syndrome on native arteries: arterial graft spasm/micro-embolism, tachyarrhythmia, cardiogenic/ hypovolaemic shock, severe respiratory failure, severe anaemia, left ventricular hypertrophy, inadequate cardioprotection from cardioplegia, cardiac handling during surgery, surgical myectomy, inflammatory injury due to cardiopulmonary bypass, heart failure, severe pulmonary embolism, sepsis, or renal failure [7, 23].
One of the strongest points of our study is that we assessed two traditional markers (CK-MB and cTnI) and a “newer” cardiac bio-marker, hFABP. We checked for concordance and observed that at 6 hours post-operatively almost all patients manifested cTnI and hFABP values over 10 times normal values, even if they had unchanged ECG and echo.
This was an expected observation since other studies reported it for cTnI [7, 22, 24]. On the other hand, it was too early to detect high values of CK-MB (which most presented as “near-normal” at 6 hours, being not “too elevated”, between 1× and 2× times the 99th percentile URL values). For each 1 point increase in SS we found a significant elevation in myocardial injury (as confirmed by two bio-markers), supporting good discriminatory power for SS.
A prospective observational study published in 2007 in the Journal of American College of Cardiology ascertained that hFABP provides direct evidence not only of acute myocyte necrosis, but also of myocardial ischaemia, better than cTnI [25]. This means that even if there is no evidence of important cardiac necrosis, repeated intervals of myocardial ischaemia (during the CABG surgery procedure) could be quantified through hFABP values – expressed as a myocardial injury parameter. Moreover, the same study mentioned that hFABP values were predictive for long-term mortality after acute coronary syndromes, while identifying high-risk patients in a manner that is additive to the GRACE clinical risk factors, troponin, and hs-CRP, possibly as a result of pinpointing the occurrence of myocardial ischaemia with/without necrosis [25].
Another recent study validated the peri-operative hFABP use for risk stratification of acute kidney injury and mortality following cardiac surgery [26]. Thus, the strong correlation between a high SS and hFABP at 6 hours demonstrated by our study could be very important for pre-CABG stratification and selection of patients prone to renal failure. It is a simple way to select those patients with a SYNTAX over the value of 30 and expect a higher hFABP, acute renal complications and significantly more post-operatory cardiovascular adverse events. This information could be used to re-assess CABG protocols and algorithms (on-pump time, number of grafts, a prompt correction of anaemia), and thus to influence the negative prognosis of such patients.
Moreover, we consider that the SYNTAX score could be used to select patients who can benefit from special cardioprotective strategies: ischaemic preconditioning (IPC), ischaemic post-conditioning (IPost) and remote ischaemic preconditioning (RIPC) [7]. A number of smaller studies have reported reduced myocardial damage with IPC, IPost, and RIPC [27]. These studies used cardiac bio-marker assessment (CK, CK-MB, and cTn) to evaluate the size of myocardial injury and to assess the cardioprotective efficacy of novel therapies. If patients at high risk of myocardial injury could be identified before CABG, “customised management pathways comprising more aggressive monitoring, investigations and/or treatment approaches may result in improved clinical outcomes” [7].
The low total number of patients in our study group represents a limitation, as well as possible referral bias, given that the research was performed in a single centre. It would have been more accurate to assess all three bio-markers at three different post-CABG time points (at 6, 12 and 24 hours respectively). Moreover, it would be interesting to include on-pump/clamping time in the analysis and also to perform a one- or two-year post-CABG follow-up.
Conclusions
Since the CABG procedure involves a great number of resources, every effort should focus on minimizing post-surgery complications and outcomes. Thus, defining myocardial injury as elevation of cardiac troponins (cardiac bio-markers) between normal values and the 10× cut-off for MI has tremendous clinical significance as this category of patients maintains high negative prognostic rates. We demonstrated that the SYNTAX score can also be used to predict a post-operative rise of cardiac bio-markers (namely, hFABP and cTn I), the correlation between SYNTAX and myocardial injury being very solid.






