Thermography is a technique that provides real-time temperature measurement and visualization of thermal energy according to color difference. While the coldest regions are observed as blue, the warmest regions are yellow in thermography, and various images are obtained on this color scale according to the temperature value. Thermal cameras can generally measure the temperature range of 10–55°C with an accuracy of 0.1°C [1]. The idea of using the thermal camera for medical purposes was first put forward by Ring in 1990, and he defined some quantitative values according to body regions [2]. Since then, the thermal camera has attracted attention in various diseases such as breast cancer, decubitus ulcer, diabetic foot, etc. [3, 4]. Sönmez et al. put forward the idea of assessing anastomosis success using a thermal camera in coronary artery bypass surgery in 2003 [5]. All medical uses of the thermal camera have emphasized its noninvasive, safe, re-applicable, and radiation-free nature [1]. Here, we aimed to present a few cases in which the thermal camera can be used safely in various thoracic surgery procedures.
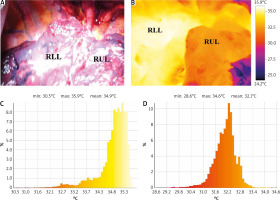
Written informed consent was obtained from each patient for the case reports and each image used. We used the thermal camera for the detection of the surgical margin in a pulmonary lobectomy procedure in a patient with lung cancer. A 65-year-old male patient was referred to us for a lung mass which was diagnosed as adenocarcinoma by transthoracic biopsy. We planned right upper lobectomy and mediastinal lymph node dissection and detected that the horizontal fissure was incomplete (Figure 1 A). After the division of pulmonary arterial and venous branches of the right upper lobe, we applied thermography to detect margins between ischemic and perfused lung areas (Figure 1 B). We also determined that there was a quantitative difference between the mean temperatures of the ischemic and perfused regions after the images were processed in the software of the thermal camera on a computer (Figures 1 C, D).
Figure 1
A – We detected that the major fissure of the right lung was incomplete. B – The thermal mapping shows color and temperature differences between ischemic and perfused lung areas. Surgeons can easily detect the resection margins by thermography. C, D – The temperature difference between ischemic and perfused areas was also quantitatively demonstrated by computer processing of images using thermal camera software
RUL – right upper lobe, RLL – right lower lobe, min.– minimum, max. – maximum.
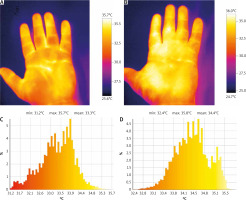
We used thermography to detect whether palmar temperature increased after an endoscopic thoracic sympathectomy (ETS) procedure for primary palmar hyperhidrosis, in another case. Usually, R3-R4 sympathectomy is performed for primary palmar hyperhidrosis, and palmar temperature is expected to rise after the procedure [6]. A 21-year-old male patient presented to us with excessive palmar hyperhidrosis. We planned an ETS procedure and performed thermography of both hands consecutively before and after R3-R4 sympathectomy. We detected both qualitative and quantitative temperature increases in the hands after the procedure (Figures 2 A, B).
Figure 2
A – The figure shows the qualitative view of the temperature increase in the hand after sympathectomy at level T3-4. B – Graphical representation of temperature difference before and after sympathectomy procedure. C – The thermal mapping effectively showed the temperature difference at the forehead and between both hands of the patient. We found that the anhidrotic right forehead and right hand were warmer than the left. D – Histograms show that the temperature difference between halves of the forehead was significant
L – left, R – right, min. – minimum, max. – maximum.
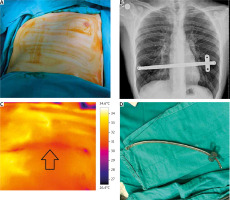
Another use of the thermal camera was in detecting a pectus implant. A 24-year-old male patient was referred for the removal of an implant which had been placed for pectus excavatum deformity 3 years previously. We performed thermography at the operating table and detected prominent coldness at the pectus implant region (Figures 3 A–D). We suspected that the reason for the temperature difference was the greater cooling in the pectus implant, the raw material of which is a nickel-steel alloy.
Figure 3
A – View of the patient’s chest on the operation table. B – Chest X-ray of patient showed the pectus implant radiologically. C – Thermography showed that the area where the pectus implant was located was colder. The arrow indicates the course of the metallic implant. D – Macroscopic view of the pectus implant which was removed
Thermography is used in various diseases for medical purposes, and we aimed to present its use in the field of thoracic surgery in this article. While inflammation and increased blood flow cause increasing temperature, ischemia, hyperhidrosis, and metallic implants cause cooling. In the first case, we used the thermal camera to determine the lobe margins in a pulmonary lobectomy procedure in a patient with an incomplete lung fissure. Defining the pulmonary parenchymal resection margins is very important in terms of both oncological and postoperative pulmonary functions in patients undergoing lung cancer surgery. Surgeons have used several maneuvers to determine the resection margins, especially in pulmonary segmentectomies, such as the indocyanine green, inflation and deflation methods. The indocyanine green technique has some negative features, such as low-cost effectiveness, need for additional imaging systems and intravenous drug administration. Ineffectiveness is the weakness of inflation-deflation methods. However, thermography may be preferred for this situation due to its principle of mapping the cooling ischemic region. Moreover, there is no need for an additional imaging system and intravenous drug administration in the thermography technique [7].
The main concern of surgeons in ETS is to achieve effective sympathetic interruption at the correct level. It is expected that palmar temperature will rise in ETS surgery performed for palmar hyperhidrosis, and it is measured by palmar temperature probes. Thermography can be a non-invasive and effective solution for determining whether the temperature rises in the upper extremity. We demonstrated this in the second case.
The implant inserted into the retrosternal region for pectus deformity consists of a nickel-steel alloy and as expected, this metal cools down faster than the normal body [8]. Thermography can detect this temperature difference, and physicians can easily locate the implant with a thermal camera. We used the thermal camera for detecting implant localization at the operating table in the third case.
In conclusion, thermography, which is a noninvasive and radiation-free imaging technique, can be useful in thoracic surgery. These case examples can be considered as an informative preliminary study for researchers.






