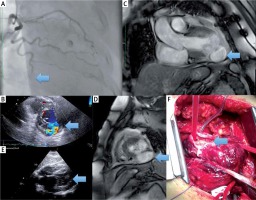
A 75-year-old hypertensive female patient presented at the cardiac department because of chest pain 20 days earlier. A suspicion of a past myocardial infarction (MI) and a pseudoaneurysm developed after echocardiography performed in the admissions office. Coronary angiography showed all vessels patent apart from the occluded left circumflex artery (LCx) (Figure 1 A). Echocardiography showed pseudoaneurysm of the lateral wall of the left ventricle (LV) and small pericardial effusion (Figure 1 B). Clinical status of the patient was stable. Cardiac magnetic resonance (CMR) was performed to rule out other cardiac pathologies – the free heart wall rupture was visualized, and consequently left ventricular pseudoaneurysm was confirmed (Figures 1 C, D). There were no abnormal laboratory results, and biomarkers of myocardial necrosis were negative. The patient was scheduled for urgent cardiac surgery. While waiting for cardiac surgery in the intensive care unit, sudden clinical state worsening was observed with symptoms of cardiogenic shock such as tachycardia (HR 120–130 bpm), blood pressure decrease (BP 65/40 mm Hg) and logic contact impaired. The following echocardiographic imaging showed heart tamponade (Figure 1 E). The patient was prepared for emergency surgery. EuroSCORE II was calculated as 21.75%. Surgery with arterial cannulation via femoral artery access to facilitate extracorporeal circulation was performed. The aneurysmal sac was cut to some degree over the right atrium to perform vein cannulation. In the next step tamponade was decompressed, showing ruptured pseudoaneurysmal sac size 51 × 39 × 31 mm (Figure 1 F). Cooley’s method was used to close the aneurysm. Clamp time was 39 min and whole extracorporeal circulation time was 79 min. The patient was discharged from hospital on the 12th day after surgery in a good clinical state.
Figure 1
A – Coronary angiography showing occlusion of circumflex artery (LCx) in distal part. B – Echocardiography parasternal short axis-view, color Doppler imaging showing pseudoaneurysm of lateral wall of left ventricle and small pericardium effusion. Cardiac magnetic resonance (CMR) imaging confirmed pseudoaneurysm. CMR long axis-view (C) and short axis-view (D) showing pseudoaneurysm. E – Because of worsening of clinical status, while waiting for the urgent cardiac surgery, controlled echocardiography was performed, showing heart tamponade. F – Emergency surgery (EuroSCORE II – 21.75%) in extracorporeal circulation with arterial cannulation via femoral artery access was performed. Cooley’s method was used to close the aneurysm
Despite development of interventional cardiology and widespread use of endovascular procedures in treatment of acute coronary syndrome, there are still observed mechanical complications of myocardial infarction. Left ventricular pseudoaneurysm is a relatively rare complication that is reported in less than 0.1% of all MI patients and the main risk factors are older age, female sex, hypertension and inferior and lateral wall MI [1]. Pseudoaneurysm is formed when cardiac rupture is contained by adherent pericardium or scar tissue, in contrast to true aneurysm which comprises full thickness of the wall [1]. Around 40% of all left ventricular wall ruptures occurred during the first 24 h and 85% within the first week [2]. The most common localization of pseudoaneurysm is inferolateral (posterior) wall (43%), lateral wall (28%), then apex (24%) followed by other segments at equal frequency [3]. Symptoms presented by patients with left ventricular pseudoaneurysm are varied and not specific, which makes the diagnosis challenging [2]. Both transthoracic and transesophageal echocardiography as well as CMR are used in the diagnostic process and in differentiating pseudoaneurysm from true aneurysm [2].
Most cases of this type of MI complications result in death due to cardiogenic shock because of heart tamponade. Knowing the natural course of acute heart pseudoaneurysm, medical therapy should be initiated urgently. The most effective method of treatment is surgical intervention, mostly open heart operation, although percutaneous coil embolization has been reported to be an alternative management in selected patients [4]. Nonetheless, the decision about the operation should be carefully analyzed because of the high surgical mortality rate [2].







