Purpose
Low-dose-rate brachytherapy is widely considered the standard treatment for localized prostate cancer. Major systemic complications during and immediately after brachytherapy are rare. The reported incidences of peri-operative and sub-acute post-operative cardiopulmonary complications after brachytherapy for prostate cancer are < 2% [1]. Firstly reported in 1991, Kounis syndrome was defined as the concurrence of acute coronary events, including coronary spasm, acute myocardial infarction, and stent thrombosis, with allergic or hypersensitivity reactions as well as anaphylactic or anaphylactoid reactions [2]. However, the epidemiology of Kounis syndrome remains unclear. One study reported that in the United States, the overall prevalence of Kounis syndrome among patients hospitalized for allergic, hypersensitivity, or anaphylactic reactions was 1.1%, with a subsequent all-cause in-patient mortality rate of 7.0% [3], indicating that Kounis syndrome is rare but has a high mortality rate. Kounis syndrome can be caused by allergens present in drugs or substances used during surgical procedures. Herein, we reported a case of a patient with a banana allergy, who developed acute myocardial infarction due to Kounis syndrome after low-dose-rate brachytherapy.
Case presentation
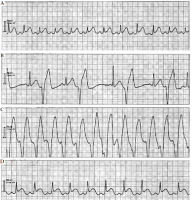
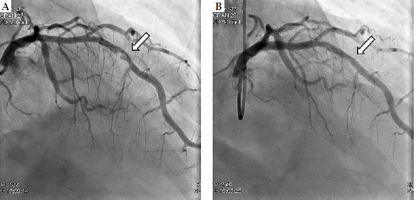
A 70-year-old patient with prostate cancer (prostate-specific antigen level of 5.5 ng/ml, Gleason score of 5 + 4 = 9, and cT2cN0M0) was referred to our hospital to undergo combination therapy comprising brachytherapy, external beam radiation, and hormone therapy. He had a history of a banana allergy and endovascular aortic repair for an abdominal aortic aneurysm. Latex-free gloves and condoms were used for endovascular aortic repair and trans-rectal prostate biopsy performed at the referring hospital. The patient received seed implantation under general anesthesia. During trans-rectal ultrasound examinations at our institute, probes were used with regular condoms rather than latex-free condoms. The needle was punctured transperineally using the standard technique, and radioactive seeds were sequentially implanted. A total of 48 seeds were transperineally inserted throughout the entire prostate, using 15 needles under ultrasound guidance and a Mick applicator. Intra-operatively, blood pressure gradually decreased; systolic blood pressure, which was 140 mmHg at the time of intubation, decreased to 70 mmHg after 55 min. The anesthesiologist administered ephedrine, a vasopressor agent, to control blood pressure, and the procedure was completed without complications. The operation time was 47 min, and anesthesia lasted for 82 min. After extubation under general anesthesia and awakening, the patient complained of itching throughout the body. Latex allergy was suspected and d-chlorpheniramine maleate was administered accordingly. The patient’s pruritus disappeared; however, his blood pressure decreased again, and electrocardiography showed ST elevation. Furthermore, the patient developed ventricular fibrillation from ventricular bigeminy, which improved with cardiac massage and epinephrine injection (Figure 1). Cardiac catheterization was performed by a cardiologist. Subsequently, percutaneous coronary intervention was performed promptly for 99% stenosis in segment 7 of the left anterior descending artery (Figure 2). The guide catheter was engaged in the left coronary artery, and percutaneous coronary intervention was initiated. The lesion was crossed with a guide wire and evaluated using optical coherence tomography. A massive thrombus was observed in the lesion; therefore, thrombus aspiration was performed with an aspiration catheter. After thrombus aspiration, a drug-eluting stent (3.0-23 mm) was placed in segment 7 of the left anterior descending artery. Optical coherence tomography revealed stent expansion failure; thus, post-dilation was performed using a non-compliant balloon (3.5-15 mm). Subsequently, long inflation was done with a perfusion balloon (3.5-22 mm) to address the thrombus that appeared within the stent. The procedure was completed after confirming the disappearance of a filling defect within the stent. The patient recovered well after the procedure, and was discharged in good general condition.
Discussion
In this case report, the patient experienced a myocardial infarction immediately after brachytherapy. A previous report has described a case of acute myocardial infarction due to the migration of a seed into the coronary artery 2 years after prostate brachytherapy. However, in our case, chest fluoroscopy performed immediately after the procedure did not reveal any migration of seeds into the coronary artery, which indicated that the myocardial infarction was not caused by seed migration [4]. Considering the symptoms and clinical course, the patient was diagnosed with acute coronary thrombosis induced by allergic and anaphylactic reactions, namely Kounis syndrome.
Kounis syndrome is defined as the concurrence of acute coronary disorders, including coronary spasm, acute myocardial infarction, and stent thrombosis, caused by allergy-induced release of mediators from mast cells. A detailed pathophysiology is suspected to involve an allergic reaction that trigger the release of inflammatory mediators, such as histamine, leukotrienes, and a platelet-activating factor. These mediators induce coronary vasospasm, destabilize atherosclerotic plaques, and promote thrombus formation, ultimately leading to acute coronary syndrome [5]. Recent studies have categorized Kounis syndrome into three types: type 1 corresponds to allergic vasospastic angina caused by endothelial dysfunction; type 2 is caused by a rupture of coronary artery plaque and subsequent thrombus formation; and type 3 is triggered by allergic stent thrombosis [6]. Here, the patient had vascular risk based on his medical history, and cardiac catheterization revealed 99% stenosis in the left anterior descending artery, consistent with type 2 Kounis syndrome.
Despite the seriousness of complications, immediate diagnosis and treatment by the anesthesiologist and cardiologist were crucial in avoiding potentially fatal outcomes. It is important to create a medical system in each institution that is prepared to manage such serious complications during brachytherapy.
To identify the exact allergen that caused Kounis syndrome, the dermatologist recommended a skin prick test with several allergens, including latex and some of the drugs used during the procedure after myocardial infarction treatment, but the patient refused the test because of the possibility of anaphylactic shock. Therefore, we could not verify the cause of allergic reaction with an allergy test. However, the allergen considered was the latex in condoms, knowing that the patient was allergic to bananas, and a regular latex condom was used to cover the trans-rectal ultrasound probe. Allergies to latex and rubber are known to have cross-reactivity with allergies to plant foods (bananas, kiwis, avocados, chestnuts, tomatoes, papayas, potatoes, etc.) [7, 8]. Latex allergies can be triggered by direct contact, such as those with materials of powdered latex gloves. Despite the patient’s banana allergy being noted and the use of latex-free gloves, one of the staff members overlooked this aspect and prepared the ultrasound probe with a regular latex condom.
In this patient, brachytherapy for the prostate was performed by a team comprising urologists, radiation oncologists, anesthesiologists, nurses, and radiology technologists. The fact that information regarding the patient’s allergies was not shared with the entire team is a point that should be reflected upon. To our knowledge, no studies have reported anaphylactic shock during trans-rectal ultrasound; however, anaphylactic shock that might be caused by latex in condoms used during trans-vaginal ultrasound examinations has been shown [9]. Moreover, several cases of Kounis syndrome due to latex allergy have been reported [10, 11]. Latex allergy can present with a variety of symptoms, ranging from mild ones, such as itching or swelling of the skin, to more severe ones, including anaphylaxis. In our patient, we observed an allergic reaction following his complaint regarding general pruritus after extubation. However, the decrease in blood pressure during surgery, which required the administration of a vasopressor agent, might indicate the possibility of intra-operative occurrence of allergic reaction.
In addition to condom latex, other potential causes of allergies included muscle relaxants and other drugs used during the surgery. Previous reports have indicated that rocuronium bromide, a muscle relaxant we applied in our case, can cause anaphylactic shocks [12, 13]. However, we confirmed with the previous institution where the patient had undergone endovascular aortic repair, to ensure that the same muscle relaxant was used, which had not resulted in any significant post-operative complications previously. Furthermore, careful consideration is required regarding a titanium allergy as iodine-125 seeds contain titanium capsules. Titanium has long been considered highly bio-compatible, with allergic reactions regarded as extremely rare. However, in recent years, reports on titanium allergy have emerged in the fields of orthopedic and dental implant treatments. In these reports, the primary symptoms of titanium allergy included dermatitis, pruritus, erythema, and tissue inflammation, while the underlying mechanism was presumed to be a type IV (delayed-type) hypersensitivity reaction [14, 15]. To our knowledge, no cases of anaphylactic shock attributed to titanium have been reported. Similarly, in our case, the possibility of an allergic reaction caused by titanium was considered doubtful. Therefore, we strongly suspected that condom latex was the allergen that induced Kounis syndrome in this patient.
Conclusions
We encountered a case of myocardial infarction after low-dose-rate brachytherapy, which was attributed to Kounis syndrome. The cause was strongly suspected to be a latex allergy to condoms used for trans-rectal ultrasound probe. Although serious complications rarely occur after brachytherapy, prompt responses to sudden adverse changes in the patient’s general condition, such as cardiac disease, during and after the procedure are important.