Summary
The inherent risk of percutanous coronary intervention performed in high-risk patients renders them vulnerable to complications. Nevertheless, there is no universal consensus on whether to use mechanical circulatory support devices in that setting, or on which kind of device is optimum in terms of safety and efficacy. The current study supports the use of well-known intra-aortic balloon pump technology with increased balloon volume because it probably diminishes the risk of significant hypotension during high-risk percutaneous coronary interventions.
Introduction
The recent developments in percutaneous coronary techniques allow for treatment of very sick patients with complex coronary anatomy, who are not suitable candidates for coronary artery bypass grafting (CABG) because of low ejection fraction (EF) and many comorbidities (so-called complex high risk and indicated patients – CHIP) [1]. This is invariably associated with increased risk of acute cardiac decompensation during the procedure, it explains the growing interest in short-term mechanical circulatory support devices (MCS). One of the best-known examples of these is intra-aortic balloon pump (IABP), which was introduced to clinical practice in the late 1960s [2]. Its postulated mechanism of action is the augmentation of diastolic aortic pressure and reduction of left ventricular systolic and diastolic pressures, leading to increased coronary blood flow and decreased heart work, which is accompanied by a small increase in cardiac output and index. Despite controversies generated by negative results of randomized controlled trials (RCTs), especially lack of mortality benefit in acute myocardial infarction (AMI) complicated by cardiogenic shock (CS) in the IABP-SHOCK-II trail [3], failure to reduce major adverse cardiac even (MACE) in high-risk percutaneous coronary interventions (HRPCI) patients in Balloon pump-assisted Coronary Intervention Study (BCIS-1) [4], and the inability of myocardial preservation in anterior AMI in CRISP AMI studies [5], IABP is still widely used by many practitioners worldwide as a valid alternative to much more expensive (Impella, Abiomed, Danvers, MA) or invasive (ECMO) devices, which is supported by the latest American guidelines with a IIb/C class recommendation (unfortunately there are no European guidelines) [6]. The latest modifications of the balloon, i.e. its increased volume, direct pressure measurement by light transmission, and improved synchronisation with cardiac cycle, make it probably more effective [7].
Aim
The present study was designed to compare, in a randomised fashion, outcomes of patients subjected to HRPCI and supported with IABP of larger volume (MEGA) compared to standard volume (STRD) or no balloon support at all (CTRL).
Material and methods
The study recruited patients scheduled for HRPCI after heart team consultation, according to clinical (not suitable candidates for surgery), echocardiographic (EF at or below 35%), and angiographic criteria (unprotected left main (LM), multivessel disease (MVD), or last-remaining vessel or significant left main lesion with the right coronary artery occluded – the last two regardless of EF). The exclusion criteria were CS, acute coronary syndrome (ACS) < 48 h, aortic dissection or severe aortic regurgitation, significant peripheral artery disease, acute stroke, or contraindications for dual antiplatelet therapy (DAPT).
The patients were randomised in a 1 : 1 : 1 fashion with randomly permuted blocks using web-based randomisation tool [8] to support with a larger volume (MEGA: 50 ml > 162 cm and 40 ml < 162 cm), standard volume (STRD: 40 ml > 162 cm and 34 ml < 162 cm), or no balloon control group (CTRL). In patients allocated to balloon treatment the maximum balloon inflation volume and 1 : 1 ratio of support was used throughout the procedure. Before PCI the right and left heart catheterisation (using Pulmonary Artery Catheter (PAC) via femoral or antecubital fossa vein and Pigtail catheter via femoral artery, respectively) was done with the assessment of intra-cardiac chamber pressures (including left ventricle systolic and diastolic pressures, pulmonary artery wedge pressure (PCWP), left ventricle pressure/time ratio (dP/dt), cardiac output (CO), and cardiac index (CI) by Fick principle). All PCIs were performed by two experienced operators in the Interventional Cardiology Clinic of John Paul II Hospital in Krakow between March 2016 and October 2017, with the aim of DES implantation and complete revascularisation according to preprocedural viability testing. The arterial access was either femoral or radial, preferably with 7 Fr sheaths. Coronary rotational atherectomy and intravascular ultrasound (IVUS) were used as needed. The invasive arterial pressure was constantly recorded by a separate line (usually radial). Procedural success was defined as residual stenosis of less than 30%, TIMI 3 flow, and no major complications. Unfractionated heparin (70–100 U/kg) and DAPT were used (ticagrelor in ACS patients, clopidogrel in stable coronary artery disease or when long-term anticoagulation was indicated) as well as optimal medical therapy according to 2014 ESC/EACTS guidelines of myocardial revascularisation [9].
We recorded standard clinical, laboratory, angiographic, and echocardiographic parameters. We assessed symptoms (CCS and NYHA), in hospital and one-year follow-up MACE (deaths, AMI or ischaemia driven revascularisation, exacerbation of chronic heart failure, or stroke), haemorrhagic (major (≥ 3) and minor (< 3) using BARC scale [10]), renal, and vascular complications. To define MI, we used the BCIS-1 definition [11]: periprocedural MI (up to 72 h post intervention) was diagnosed when creatinine kinase MB (CK-MB) increased more than 3× in patients with normal CK-MB at baseline or > 1.5× when they were already elevated. After 72 h the standard ESC (4th) definition of MI was used [12]. For clinical risk assessment we used Euroscore II [13], for angiographic complexity and risk evaluation Syntax Score [14] and BCIS-1 Jeopardy Score [11]. All patients were followed up for 12 months after PCI.
For the purpose of this study a new haemodynamic composite end point was defined. First, we introduced a novel hypotension index – hypotension load (HL), which was calculated according to the following algorithm:
arterial pressure values were sampled in 10-second intervals,
for each minute interval a mean arterial pressure (MAP) value was calculated,
before the PCI the patient-specific arterial hypotension threshold (PSAHT) was set by calculating for a minimum of 5 min average MAP minus two standard deviations,
if, during PCI, for a given minute, the MAP value was below PSAHT, then a hypotension episode was considered to be occurring in this minute, and the difference between PSAHT and MAP was calculated,
HL is the sum of (PSAHT-MAP) divided by PCI duration time in minutes.
The arbitrary cut-off value for HL of ≥ 2 mm Hg/min was chosen as the first condition of a significant hypotension episode. Further, we decided that a MAP decrease of at least 40% of PSAHT at any time during the PCI (maximal hypotension episode (MHEP) = (minimum MAP – PSAHT/PSAHT) × 100%) also qualifies as a significant hypotension episode (second condition). Lastly, we took in consideration the pure clinical definition of haemodynamic instability (third condition), namely when hypotension required intervention (e.g. fluid bolus, administration of catecholamines, intubation, defibrillation, resuscitation, or crossover to salvage IABP therapy). All of above-mentioned conditions (1 to 3) together formed our composite haemodynamic endpoint.
The study protocol was approved by the Local Bioethics Committee.
Statistical analysis
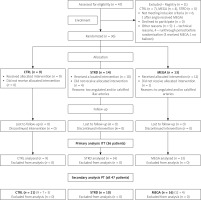
We performed primary intension-to-treat (ITT) analysis for 36 randomised patients and secondary per-treatment (PT) analysis for all 47 patients (randomised and from the registry).
Categorical variables were presented as counts and percentages, and continuous variables were presented as mean with standard deviation or median with the first and the third quartile as appropriate. Normality was assessed using the Shapiro-Wilk test. Equality of variances was tested using the Levene test. Comparisons of continuous variables were preformed using analysis of variance or Kruskal-Wallis test as appropriate. Post hoc analysis was performed using Tukey’s HSD or the Steel-Dwass test, as appropriate. Paired analysis was performed using the mixed effect model. Pearson’s or Spearman’s correlation coefficients were calculated, as appropriate, based on the normality of the data. Fisher’s exact test or the χ2 test were used to compare distributions of nominal variables. Simple logistic regression models were used to calculate odds ratios for the composite endpoints. A multiple logistic regression model was then constructed. All potential predictors were screened. All variables for which simple models showed a p-value less than 0.15 were candidates for the multiple model. A stepwise approach was used and minimisation of a Bayesian information criterion (BIC) was used as a target. The type of balloon used was locked in the model. C-statistic was calculated as a measure of goodness of fit. Bootstrap validation was performed with 1000 iterations. Variance inflation factors (VIF) were calculated to measure collinearity.
All tests were two-sided, and p < 0.05 was assumed to indicate statistical significance. All data management and analysis activities were performed using JMP 14.2 (2019, SAS Institute Inc., Cary, NC, USA) and R 3.5.3 (R Core Team [2019]) [15].
Results
In the study period we were able to screen 47 patients, 36 of whom were randomised: 13 in MEGA, 14 in STRD, and 9 in the CTRL group. Four patients in the CTRL group and one patient in the MEGA group did not receive the allocated intervention because of severely angulated and/or calcified femoral/iliac arteries. Eleven patients were screening failures but finally received one of the analysed treatments (MEGA, STRD, CTRL) and formed a registry (REG). Additional per treatment (PT) analysis was performed to control for cross-over and after adding REG patients, which included 47 subjects: 21 in the CTRL, 10 in the STRD, and 16 in the MEGA group (Figure 1).
The clinical data for randomised patients is shown in Table I. Almost all analysed parameters were equally distributed between the study subgroups, with the exception of more frequent diagnosis of ACS and slightly greater EF in the MEGA group. The randomised patients were characterised by a very high-risk profile with a mean EF of 30%, median Syntax Score of 38 points, median Euroscore II mortality risk of 6%, and median BCIS-1 Jeopardy Score of 12.0. These baseline characteristics were also similar in PT analysis with no difference between the groups, apart from more frequent peripheral artery disease in the CTRL group (Table II).
Table I
Clinical, demographic, echocardiographic, angiographic, and procedural data (ITT)
| Variable | MEGA | STRD | CTRL | Total |
|---|---|---|---|---|
| N (%) | 13 (36) | 14 (38) | 9 (25) | 36 (100) |
| Demographic data: | ||||
| Age [years], mean ± SD | 71.9 ±8.3 | 73.3 ±11.2 | 67.4 ±10.5 | 71.3 ±10.0 |
| Male sex | 11 (84.6) | 11 (78.6) | 8 (88.9) | 30 (83.3) |
| ACS at presentation* | 10 (76.9) | 5 (35.7) | 3 (33.3) | 18 (50.0) |
| Clinical symptoms: | ||||
| CCS class 3/4 | 9 (69.2) | 11 (78.6) | 3 (33.3) | 23 (63.9) |
| NYHA class 3/4 | 8 (61.5) | 12 (85.7) | 8 (88.7) | 28 (77.8) |
| Past medical history: | ||||
| Hypertension | 13 (100.0) | 14 (100.0) | 9 (100.0) | 36 (100.0) |
| Diabetes | 4 (30.8) | 9 (64.3) | 4 (44.4) | 17 (47.2) |
| Smoking | 7 (58.3) | 10 (71.4) | 7 (77.8) | 24 (68.6) |
| Previous MI | 6 (46.2) | 9 (64.3) | 7 (77.8) | 22 (61.1) |
| Previous PCI | 4 (30.8) | 6 (42.7) | 3 (33.3) | 13 (36.1) |
| Previous CABG | 1 (7.7) | 2 (14.3) | 1 (11.1) | 4 (11.1) |
| Previous stroke | 2 (15.4) | 1 (7.1) | 4 (44.4) | 7 (19.4) |
| Heart failure | 7 (53.9) | 10 (71.4) | 8 (88.9) | 25 (69.4) |
| Atrial fibrillation | 2 (15.4) | 6 (42.9) | 3 (33.3) | 11 (30.6) |
| Hypercholesterolaemia | 11 (84.6) | 10 (71.4) | 6 (66.7) | 27 (75.0) |
| Chronic kidney disease | 4 (30.8) | 3 (21.4) | 3 (33.3) | 10 (27.8) |
| Peripheral artery disease | 4 (30.8) | 3 (21.4) | 4 (44.4) | 11 (30.6) |
| Echo examination: | ||||
| EF (%), mean ± SD** | 35 ±12 | 29 ±10 | 25 ±7 | 30 ±11 |
| Significant mitral regurg. | 6 (46.2) | 5 (35.7) | 4 (44.4) | 15 (41.7) |
| Risk scales: | ||||
| SYNTAX score, median (IQR) | 42.0 (30.0; 52.0) | 38.5 (29.6; 47.1) | 36.3 (24.5; 42.8) | 38.0 (29.0; 47.0) |
| EUROSCORE II (%), median (IQR) | 6.0 (3.0; 14.0) | 7.0 (3.0; 13.0) | 5.0 (3.0.0; 19.0) | 6.0 (3.0; 14.0) |
| BCIS-1 Jeopardy score, median (IQR) | 12.0 (10.0; 12.0) | 12.0 (9.5; 12.0) | 10.0 (8.0; 12.0) | 12.0 (8.0; 12.0) |
| Angiographic data: | ||||
| Left main stenosis | 8 (61.5) | 9 (64.3) | 5 (55.6) | 22 (61.1) |
| CTO present | 9 (69.2) | 12 (85.7) | 7 (77.8) | 28 (77.8) |
| PCI MVD (≥ 2 vessels) | 10 (76.9) | 10 (71.4) | 7 (77.8) | 27 (75.0) |
| Radiation [GY], mean ± SD | 2.4 ±1.6 | 2.3 ±1.4 | 2.7 ±1.7 | 2.4 ±1.5 |
| Contrast vol. [ml], mean ± SD | 317 ±94 | 313 ±83 | 293 ±86 | 310 ±86 |
| No. of stents, median (IQR) | 2.0 (1.15; 3.0) | 2.0 (1.8; 2.3) | 2.0 (1.0; 3.0) | 2.0 (1.3; 3.0) |
| Rotablation | 3 (23.1) | 4 (28.6) | 1 (11.1) | 8 (22.2) |
| IVUS | 2 (15.4) | 5 (35.7) | 2 (22.2) | 9 (25.0) |
Table II
Clinical, demographic, echocardiographic, angiographic, and procedural data (PT)
| Variable | MEGA | STRD | CTRL | Total |
|---|---|---|---|---|
| N (%) | 16 (34) | 10 (21) | 21 (45) | 47 (100) |
| Demographic data: | ||||
| Age [years], mean ± SD | 71.4 ±8.4 | 71.3 ±11.5 | 71.7 ±10.1 | 71.5 ±9.7 |
| Male sex | 13 (81.3) | 8 (80.0) | 18 (85.7) | 39 (82.9) |
| ACS at presentation | 11 (68.8) | 3 (30.0) | 8 (38.1) | 22 (46.8) |
| Clinical symptoms: | ||||
| CCS class 3/4 | 10 (62.5) | 7 (70.0) | 10 (47.6) | 27 (57.5) |
| NYHA class 3/4 | 11 (68.8) | 8 (80.0) | 14 (66.7) | 33 (70.2) |
| Past medical history: | ||||
| Hypertension | 16 (100.0) | 10 (100.0) | 20 (95.2) | 46 (97.9) |
| Diabetes | 7 (43.8) | 6 (60.0) | 10 (47.6) | 23 (48.9) |
| Smoking | 8 (53.3) | 8 (80.0) | 16 (76.2) | 32 (69.6) |
| Previous MI | 8 (50.0) | 6 (60.0) | 13 (61.9) | 27 (57.5) |
| Previous PCI | 5 (31.3) | 4 (40.0) | 7 (33.3) | 16 (34.0) |
| Previous CABG | 2 (12.5) | 1 (10.0) | 2 (9.5) | 5 (10.6) |
| Previous stroke | 2 (12.5) | 0 (0.0) | 6 (28.6) | 8 (17.0) |
| Heart failure | 10 (62.5) | 6 (60.0) | 16 (76.2) | 32 (68.1) |
| Atrial fibrillation | 5 (31.3) | 5 (50.0) | 6 (28.6) | 16 (34.0) |
| Hypercholesterolaemia | 13 (81.3) | 6 (60.0) | 15 (71.4) | 34 (72.3) |
| Chronic kidney disease | 7 (43.8) | 1 (10.0) | 5 (23.8) | 13 (27.7) |
| Peripheral artery disease* | 6 (37.5) | 0 (0.0) | 11 (52.4) | 17 (36.1) |
| Echo examination: | ||||
| EF (%), mean ± SD | 33 ±9 | 29 ±11 | 33 ±13 | 32 ±11 |
| Significant mitral regurg. | 8 (50.0) | 4 (40.0) | 8 (38.1) | 20 (42.6) |
| Risk scales: | ||||
| SYNTAX score, median (IQR) | 36.5 (29.1; 49.6) | 38.5 (29.6; 43.0) | 36.3 (27.8; 45.5) | 38.0 (29.0; 44.5) |
| EUROSCORE II (%), median (IQR) | 8 (4; 14) | 6 (2; 8) | 5 (4; 15) | 6 (3; 12) |
| BCIS-1 Jeopardy score, median (IQR) | 12.0 (9.0; 12.0) | 12.0 (10.0; 12.0) | 12.0 (8.0; 12.0) | 12.0 (8.0; 12.0) |
| Angiographic data: | ||||
| Left main stenosis | 11 (68.8) | 6 (60.00) | 15 (71.43) | 32 (68.09) |
| CTO present | 12 (75.0) | 9 (90.00) | 17 (80.95) | 38 (80.85) |
| PCI MVD (≥ 2 vessels) | 13 (81.3) | 7 (70.00) | 17 (80.95) | 37 (78.72) |
| Radiation [GY], mean ± SD | 2.4 ±1.5 | 2.3 ±1.5 | 2.3 ±1.3 | 2.3 ±1.4 |
| Contrast vol. [ml], mean ± SD | 317 ±89 | 310 ±94 | 295 ±71 | 305 ±81 |
| No. of stents, median (IQR) | 2.0 (1.0; 3.0) | 2.0 (1.0; 2.3) | 2.0 (1.5; 2.5) | 2.0 (1.0; 3.0) |
| Rotablation | 2 (12.5) | 3 (30.0) | 5 (23.8) | 10 (21.3) |
| IVUS | 3 (18.8) | 5 (50.0) | 5 (23.8) | 13 (27.7) |
There was no difference in in-hospital and follow-up MACE incidence on ITT analysis for randomised patients: MACE during hospitalisation was observed in 23.1% of patients in the MEGA group, 7.1% of the STRD group, and 33.3% of the CTRL group (p = 0.25) and at FU in 50.0%, 35.7%, and 55.6%, respectively (p = 0.61). Also, we did not observe any difference in safety endpoints: major or minor haemorrhagic complications, acute renal failure, or vascular complications (Table III).
Table III
In-hospital and follow-up MACE and safety endpoints (ITT)
The most frequent causes of major bleeds were: large haematoma at the vascular access site (n = 3), bleeding at the site of intravascular catheter without haematoma formation (n = 2), coronary artery perforation with cardiac tamponade (n = 2), significant haemoglobin drop without obvious cause (n = 2), gastrointestinal bleeding (n = 1), alveolar haemorrhage (n = 1), and vascular surgical intervention (n = 1).
In ITT analysis composite haemodynamic endpoint was achieved in 2 of 13 (15.4%) patients in MEGA, in 7 of 14 (50.0%) patients in STRD, and in 4 of 9 (44.4%) patients in the CTRL group, which potentially indicates clinical relevance, although no statistical significance was achieved (p = 0.12). One patient in the CTRL group required urgent cross-over to IABP therapy due to shock (Table IV).
Table IV
Composite haemodynamic endpoint (ITT)
Due to the occurrence of crossovers a PT set was formed, consisting of 16 patients in the MEGA, 10 in the STRD, and 21 in the CTRL group, including 11 patients initially assigned to REG, who finally received one of analysed treatments (MEGA, STRD, CTRL). In PT analysis there was no difference in study endpoints: MACE during hospitalisation was observed in 18.8% of patients in the MEGA group, 10.0% of the STRD group, and 23.8% of the CTRL group (p = 0.64), MACE at FU occurred in 53.3%, 20.0%, and 57.1% (p = 0.12), major bleeding in 37.5%, 20.0%, and 33.3% (p = 0.62), and minor bleeding in 12.5%, 30.0%, and 9.52%, respectively (p = 0.35) (Table V).
Table V
In-hospital and follow-up MACE and safety endpoints (PT)
Conversely, in PT analysis, we found a significant difference between the study subgroups for the occurrence of the composite haemodynamic endpoint (MEGA 12.5%, STRD 50.0%, and CTRL 52.4%; p = 0.02), although its individual components were not different (Table VI).
Table VI
Composite haemodynamic endpoint (PT)
In addition, patients who had had haemodynamic instability (assessed by a positive haemodynamic composite endpoint) were more likely to have periprocedural MI than patients who did not experience instability (33.3% vs. 3.4%, p = 0.01), with no difference in incidence of acute kidney injury (16.7% vs. 6.9%, p = 0.29).
Finally, on the PT cohort, we performed simple and multiple analyses for the occurrence of composite haemodynamic endpoint. In a simple model we found significant correlations with end diastolic volume (EDV), syntax score, left main (LM) disease, PCI of LM, and PCI with rotablation and PCI complications. Then, using multiple regression analysis, we created a multivariable model that showed that PCI with MEGA balloon in comparison to STRD or CTRL diminished the risk of haemodynamic composite endpoint and, at the same time, performing PCI of the left main coronary artery or rotational atherectomy increased that risk. The C-statistic for the final multiple model was 0.889, and the bootstrap C-statistic was 0.828, which indicates a strong model. All VIFs were smaller than 2 (the highest for rotablation – 1.39, and the lowest for left main – 1.22).
Cardiac index measured pre-procedurally in this model did not have any influence on haemodynamic instability risk (Table VII).
Table VII
Univariable and multivariable models for haemodynamic composite endpoint (PT)
Discussion
The goal of circulatory support in a high-risk PCI setting is to maintain a stable haemodynamic state throughout the intervention by altering the myocardial ischaemic threshold and allowing time for complex procedure, especially when complications (embolisation, dissection, abrupt vessel closure, etc.) develop. Therefore, theoretically, the best cardiac assist device would reduce myocardial oxygen demand (via reductions in myocardial wall tension) and simultaneously increase oxygen supply by augmenting diastolic pressure and coronary blood flow. On the other hand, it should be easily percutaneously implanted and small enough to decrease the risk of vascular complications [16].
The present study is, to our knowledge, the only randomised study comparing larger volume IABP with standard volume or no balloon support during HRPCI. Unfortunately, we could not show any difference between the groups in ITT analysis for the occurrence of MACE during hospitalisation and at 1-year follow-up. This was also true in PT analysis replicating the results of much larger studies, such as BICIS-1, which recruited patients to elective standard volume IABP placement before HRPCI or to a no-balloon control group. The reported 30-day MACE rate in this trial was 15.2% in IABP and 16.0% in CTRL patients (p = 0.85) [4]. It needs to be stressed, however, that after 5 years of FU in the BICIS-1 trial the mortality rate in elective IABP patients was less than in the CTRL group (OR = 0.66, 95% CI: 0.44–0.98; p = 0.039) [17]. Some metanalyses also suggest that there could be mortality benefit of elective IABP during HRPCI [18], but some others did not [19]. The debate is still ongoing whether more potent devices such as the Impella percutaneous axial heart pump (Abiomed, Danvers, MA) should substitute IABP. To date, there is only one randomised trial of Impella 2.5 vs. IABP (standard volume) in an HRPCI setting – the PROTECT II study [20], which failed to meet its primary 30-day composite end-point of reducing MACE in primary ITT analysis (30-day MACE Impella 35.1% vs. IABP 42.2%, p = 0.092), although secondary PT analysis showed superiority of the more potent device (90-day MACE Impella 40.0% vs. IABP 51.0%, p = 0.023). On the other hand, new registry studies raise further doubts on the percutaneous pump, showing higher rates of bleeding, stroke, and even death in both HRPCI and shock indication [21]. Last but not least, there is fresh evidence in favour of IABP – it has recently been shown that 50 ml IABP outperformed inotropes (enoximone or dobutamine) in acute heart failure patients without acute coronary syndrome [22].
Our study did not show a difference in the rate of major or minor bleedings according to BARC definitions between the study groups, similarly to the BICIS-1 study, as well as the risk of vascular and renal complications. The results of IABP-SHOCK II also confirm that IABP therapy is safe, with the same rate of major bleedings as in the control group. At the same time, as was said before, although more potent, the Impella pump, being larger in diameter than IABP, increases the incidence of vascular complications and the bleeding rate in comparison to IABP.
Because our study was not powered enough to access hard clinical outcomes, we compared the occurrence of significant hypotension between the groups as a secondary outcome. Unfortunately, there is no universal definition of severe intraprocedural hypotension. Some authors defined it as a decrease of mean arterial pressure below the cut-off point of 75 mmHg for at least 10 min despite fluid resuscitation or requirement of inotropic support, as was used in the BCIS-1 trial. Others reported severe hypotension if systolic blood pressure or augmented diastolic pressure (the higher of the two) fell below 90 mm Hg for ≥ 5 min requiring inotropic/pressor medication or IV fluids while on device support, as in the PROTECT II trail. For the purpose of this study we introduced novel hypotension indices such as hypotension load (HL), which, as we described, captures all hypotension episodes during the PCI in relation to the baseline mean arterial pressure threshold value and is indexed for units of time and maximum hypotension episode (MHEP), which is the minimum pressure below the threshold value, which, together with pure clinical instability, formed our composite haemodynamic endpoint. In ITT analysis this new composite haemodynamic endpoint was close to reaching statistical significance, which potentially indicates clinical relevance. Conversely, in PT analysis, the observed difference was statistically significant, with the lowest incidence of haemodynamic instability in the MEGA group. Similarly, in the BICIS-1 trial there were fewer procedural complications in the IABP group (1.3% vs. 10.7%, p < 0.001), the majority of which were prolonged hypotension episodes in the no-elective IABP group (in 12% of cases requiring emergency IABP placement). On the other hand, in PROTECT II significant hypotension occurred in 9% of IABP patients and 4.0% of Impella patients, which was not statistically significant (p = 0.07), although cardiac power output (CPO) during PCI was better preserved with Impella than with IABP (maximal drop of CPO of –0.04 ±0.24 vs. –0.14 ±0.27, p = 0.001, respectively). But, as was said before, a standard volume balloon was used. It is then probable that even such a small additional balloon volume could have a substantial effect on hypotension risk. The haemodynamic profile of larger volume balloon was studied by Kapur et al., who demonstrated greater augmented diastolic blood pressure, greater systolic unloading (which were both linearly correlated), and a larger reduction of PCWP of 50 ml balloon in respect to 40 ml in both HRPCI and shock patients [7].
To account for cross-over and after including REG patients to the PT cohort, we subsequently performed multiple regression analysis, which showed that circulatory support with IABP of larger volume was independently correlated with diminished risk of composite haemodynamic endpoint (MEGA vs. STRD: OR = 0.062, p = 0.034 and MEGA vs. CTRL: OR = 0.032, p = 0.002). There is evidence from a recently published paper from the anaesthesiological field that may be clinically relevant because the authors, after analysing various absolute and relative thresholds for hypotension, showed that a decrease of MAP below 65 mm Hg or below 20% from baseline were both related to myocardial injury after noncardiac surgery (MINS) and acute kidney injury (AKI). Moreover, at any given threshold prolonged exposure was associated with increased odds of risk. At a MAP of 50 mm Hg, for example, just one minute was enough to significantly increase the risk for both myocardial and renal injury [23]. In our study the composite endpoint of haemodynamic instability was shown to be correlated to in-hospital (periprocedural) myocardial infarction, but not with AKI.
It should be stressed that all of the IABP implantations in our study were done electively before PCI had started, which, according to various clinical studies, especially on AMICS, would be the preferred timing for MCS usage, instead of inserting it only after the procedure has been completed [24]. On the other hand, only one of our patients initially randomised to the CTRL group had to be crossed over to IABP strategy as a consequence of severe haemodynamic instability.
Finally, we also demonstrated that haemodynamic instability was more frequent if rotational atherectomy was used or PCI of the left main coronary artery was performed, which is in line with common thoughts. But, rather unexpectedly, we found that cardiac index or EF did not have a statistically significant influence on composite haemodynamic endpoint. We speculate that this observation could be explained by the fact that almost all of our patients had relatively low baseline EF (32 ±11%) and CI (mean: 2.6 ±0.68 l/min), and these results could have been different if we had recruited less sick patients with greater EF and CI.
Our study has important limitations. It was designed as a randomised study, but due to the slow recruitment process (single-centre study) we were able to randomise only 36 patients during the study period (18 months). Thus, it was significantly insufficiently powered to show any difference in hard clinical endpoints and should be viewed only as a pilot study. Moreover, we observed some cross-over due to inability to implant the device when tortuous or calcified femoral and iliac vessels were discovered intra-procedurally. To account for this limitation, we decided to perform PT analysis and increase the number of patients adding subjects from the REG and calculate the secondary outcome of composite haemodynamic endpoint using multiple regression models. Moreover, our composite haemodynamic endpoint is novel and needs further investigation to show its clinical significance or lack thereof.