Introduction
Cervical cancer is the fourth most common cancer among women worldwide, with an annual incidence of 570,000 cases and 311,000 deaths. In early stage, cervical cancer can be treated by surgery [1]. Treatment of locally advanced cervical cancer relies on a combination of external beam radiotherapy (EBRT) with concomitant chemotherapy, followed by cervix brachytherapy (BT) [2].
Major improvement has been achieved within the previous years, and image-guided adaptive brachytherapy (IGABT) has become the standard of care to improve tumor control and reduce acute and late toxicities [3].
For patients with a history of non-cancer-related partial hysterectomy, the management of cervical stump cancer should follow recommendations for patients without previous sub-total hysterectomy [2]. However, brachytherapy technique must be adapted to patient’s anatomy, especially due to proximity of organs at risk.
Previous studies have reported the efficacy and feasibility of brachytherapy with cesium or radium sources, but to the best of our knowledge, there are very scarce data with modern image-guided brachytherapy [4].
The aim of this study was to report our experience in terms of technique and dosimetric and clinical outcomes of iridium-192 (192Ir) IGABT in cervical stump carcinoma patients.
Material and methods
The study consisted of patients treated with IGABT for pathologically confirmed squamous cell carcinoma (SCC) or adenocarcinoma of the cervical stump at the Centre Léon Bérard between May 2013 and March 2020. All patients were treated using sub-total hysterectomy for non-carcinologic reasons at least 5 years before the diagnosis. All patients had received pelvic EBRT (with or without concomitant chemotherapy) before BT.
Pre-treatment workup encompassed a clinical gynecologic examination performed by a brachytherapist, and an MRI was performed to assess local extension, especially to the vagina and parametrium. Tumor response assessment before BT was based on MRI performed at the completion of EBRT, and a new clinical examination performed by a brachytherapist under anesthesia (general or epidural anesthesia) was carried out in the operating room at the time of BT.
BT procedure
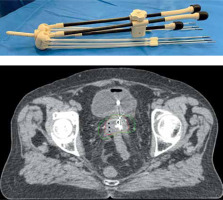
Tandem-ovoid Utrecht applicator (Elekta®, Veenendaal, the Netherlands) was used for all patients (Figure 1). The intra-uterine tube was placed in the residual cervical cavity, with a length adapted to the hysterometry, and two ovoids were inserted as close as possible to the cervix. Additional interstitial needles were systematically inserted within the cervix (using internal holes of the ovoids) and/or within the parametrium (external holes of the ovoids). Whole procedure was guided using pre-operative transrectal echography.
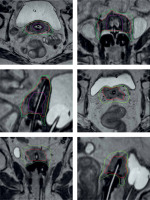
At the end of the procedure, fluoroscopy was performed to verify the position of the applicator and needles. The position of the applicator was secured with a Vaseline gauze placed in the vagina to prevent accidental removing of the applicators. Target volumes (HR-CTV and IR-CTV) and organs at risk (OARs) delineation were performed on a 3D post-operative CT scan and, when available, a post-operative MRI fused with CT [5], following GEC-ESTRO recommendations [6] (Figure 2). Dosimetry was performed on Oncentra® Brachy v.4.5 software (Elekta). Dose prescription for CTVs and dose constraints for OARs followed GEC-ESTRO recommendations [6]. Low-dose-rate (PDR) or high-dose-rate (HDR) BT techniques with 192Ir source projectors (MicroSelectron® Digital v.2) were available. PDR-BT was delivered with one pulse per hour, 24 hours a day, while HDR-BT was delivered in 5 sessions, for 3 consecutive days, 2 sessions per day, at least 6 hours apart.
Results
Patients, tumor characteristics, EBRT, and CT modalities are summarized in Table 1. From May 2013 to March 2020, 6 patients were treated at the Centre Léon Bérard for cervical cancer stump carcinoma (previously treated using sub-total hysterectomy) with brachytherapy using tandem-ovoid Utrecht applicator (Elekta®, Veenendaal, the Netherlands), in addition to pelvic EBRT. The median age was 82.5 years (range, 71-88 years). All tumors were squamous cell carcinoma, p16 positive. Four patients had a parametrial extension associated with a vaginal upper third extension in three cases. One patient was classified as T4 because of a bladder extension (muscle invasion with healthy mucosa on cystoscopy). Two patients were treated by EBRT and concomitant CT, and four patients with EBRT alone because of an advanced age and associated co-morbidities. The median time from the end of EBRT and BT was 22.5 days (range, 10-32 days). A complete or partial clinical response was achieved in 2 and 4 patients, respectively, at the time of BT. External parametrial interstitial needles were used in all patients, associated with internal cervical needles in three cases. Dosimetry was based on CT scan and MRI in four cases, and on CT-scan only in two patients. A pulsed-dose-rate technique was applied in all but one patient.
Table 1
Patients’ characteristics
Dosimetric results
Brachytherapy modalities and dosimetric data are demonstrated in Table 2. Brachytherapy target volumes included residual gross tumor volume (GTV), high-risk clinical target volume (HR-CTV, with GTV and the residual cervix), and intermediate-risk clinical target volume (IR-CTV), including HR-CTV, plus a 5-10 mm margin and the initial tumor extension). The HR-CTV was small, less than 17 cc, except for one patient (35 cc). The mean HR-CTV D90 was 81.2 Gy (> 80 Gy in all but one), with a minimal dose of 64 Gy to IR-CTV D90. The dose constraints to OARs were respected; however, with a high D2cc dose to the bladder (89 Gy EQD2) for the patient with the highest HR-CTV volume.
Table 2
Brachytherapy modalities and dosimetric data. All doses are expressed in Gy EQD2 using and α/β ratio of 10 for CTVs and 3 for OARs, with a summation of EBRT and BT doses
Clinical outcomes
Brachytherapy implantation was performed with no immediate toxicity (no perforation, no bleeding, and no infection). With a median follow-up of 26.5 months (range, 10-92 months), all patients achieved a complete response at the last follow-up. No acute or late grade 2 or more urinary or digestive toxicity were reported.
Discussion
To the best of our knowledge, only one case report of IGABT has been published to date. The technique used and the results are comparable to ours [4]. Six retrospective studies have evaluated brachytherapy in cervical stump cancer [7-12]. These studies were published between 1982 and 1997, and considered patients treated between 1953 and 1990, historically with radium in 4 papers (including one study with additional gold seed implanted in the parametrium), and cesium or iridium wires in 2 studies. In the radium series, oncologic results were similar with carcinomas developed on an intact uterus, but associated with frequent and severe toxicities.
Barillot et al. reported a large multicentric series of 213 patients with a cervical stump cancer treated either with radiotherapy alone (163 patients): EBRT + BT (86 patients), EBRT alone (75 cases), BT alone (2 patients), or radiotherapy associated with surgery (33 cases), most of all with BT first, followed by surgery (29 patients) with additional EBRT in 16 patients [9]. In that large series, brachytherapy combined with EBRT was associated with a higher loco-regional control compared to EBRT alone (81.5% vs. 38.5%). Loco-regional control was similar on equal stages between radiotherapy alone and treatment schemes including surgery, but the combined approach was associated with much more severe toxicity, including lethal complications.
Hannoun-Levi et al. reported a retrospective mono-centric series of 77 patients with cervical stump cancer treated by EBRT + BT (45 patients), EBRT alone (27 patients), BT + surgery (3 patients), BT alone (1 patient) or BT + surgery + EBRT (1 patient) [11]. In this series, exclusive radiation therapy appeared to be as efficient as radio-surgery combination. In Barillot et al. multi-centric series and in Hannoun-Levi et al. mono-centric series, loco-regional control and toxicity rate were similar for cervical stump cancers when compared to data obtained by the authors in carcinomas developed in intact uterus, treated during the same periods in their respective institutions.
Our study presents detailed data to assess the dosimetric and clinical outcomes of modern brachytherapy technics, including 3D-optimized dosimetry, and Utrecht applicator for cervical stump carcinoma in 6 consecutive patients treated homogeneously with EBRT and BT. Because of the advanced age and associated comorbidity, only 2 patients of less than 80 years old received concomitant chemotherapy.
The placement of device is quite easy for a brachytherapist trained in modern cervix brachytherapy technic with interstitial implant. However, there is a need aware of the risk of uterine perforation with the uterine probe, and the need to use interstitial needle to allow an adequate dosimetry. Transrectal ultrasound may be very useful in that situation to adapt the uterine catheter and the length of parametrial needles.
Despite the vicinity of organs at risk (especially the intestine or sigmoid loops and bladder), the dosimetric results were satisfactory, both for target volume and organs at risk dose distribution, except for one patient with the bladder D2cc exceeding 80 Gy. Most of all, these dosimetric results translate to date with the achievement of complete response in all patients, with no grade 2 or more reported toxicities. These results are in agreement with the literature, both in terms of tumor control [5] and toxicity [13-15]. This achievement has certainly been made possible by the insertion of interstitial needles within the residual cervix and the parametrium, considering tumor extension at the time of diagnosis and tumor shrinking after EBRT. Dosimetric and clinical positive impact of adding interstitial needles has been proven in modern series of cervix brachytherapy for intact uterine [16, 17], and this approach was already reported in cervical stump carcinoma series, including those using radium sources. The interest of parametric needles is crucial in the case of cervical stump: they make it possible to go beyond CTV, which is not possible with the uterine catheter.