Purpose
Cervical carcinoma is the fourth most common cancer in women worldwide [1]. Despite measures taken to spread the awareness of screening and early detection of this disease, majority of patients still present at an advanced stage, especially in low- and middle-income countries [2]. Brachytherapy boost after external beam radiotherapy (EBRT) has long been the standard of care to treat locally advanced cervical carcinoma [3, 4]. Cervical brachytherapy is performed using either an intra-cavitary, interstitial, or combined approach [5]. Recent studies have highlighted that a hybrid (combined) approach, i.e., intra-cavitary/interstitial (IC/IS) brachytherapy yields better results in terms of dose coverage and limiting organ at risk (OAR) toxicity, leading to overall survival advantage [6-8].
In cervical tandem-ovoid brachytherapy, misplacement or sub-optimal insertion of the tandem is not an uncommon occurrence [9]. Sub-optimal or misplaced tandem placement can be defined as inability to pass the tandem beyond external os or internal os, so that the tip of the tandem stays in the cervix rather than at its desired position, i.e., reaching up to the uterine fundus after passing through internal os [9]. Acute angle between the uterine and cervical axis resulting in a poor pelvic geometry is a common cause of failure of tandem insertion [10]. Moreover, it can be caused by post-EBRT fibrosis or obstruction in the cervical canal by gross residual disease [9]. As the tandem fails to cover the intended distance fully, it can result in underdosing of clinical target volume (CTV), leading to potentially increased doses to organs at risk (OARs), such as the bladder, rectum, and sigmoid colon.
One way to overcome this underdosing is to create an iatrogenic path under anesthesia using sharp dissection. However, in low- and middle-income countries, the facility of performing a procedure under anesthesia, 3-5 times within 2 weeks, is not widely available. Furthermore, the risk of complications induced by repeated spinal or general anesthesia is significant. On the other hand, conscious sedation has a comparably lower rate of complications as compared with general anesthesia in cervical brachytherapy [11]. In our center, cervical brachytherapy is efficiently performed under conscious sedation using intravenous analgesics.
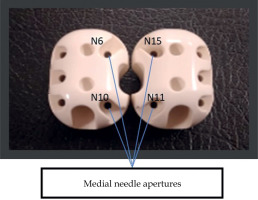
At present, no guidelines or protocols exist to efficiently overcome the dose dilemma caused by sub-optimal tandem insertions. Since interstitial brachytherapy is now being increasingly practiced for optimizing CTV coverage and reducing the dose to OARs, needles close to tandem, if inserted parallel, can serve as surrogates for sub-optimal insertions. For Utrecht apparatus, medial needles (as shown in Figure 1) can be used for this purpose. We hypothesized that instead of creating an iatrogenic path under anesthesia, interstitial insertion of one or more medial needles can optimize CTV dose coverage while minimizing toxicity to OARs.
Fig. 1
Configuration of interstitial needles in cervical tandem-ovoid Utrecht applicator. N6 and N15 are anterior medial needle apertures. N10 and N11 are posterior medial needle apertures
This study aimed to evaluate the dosimetric advantage provided specifically by the insertion of medial needles using Utrecht applicator in patients where tandem was misplaced or sub-optimally inserted.
Material and methods
It was a single institution observational study comparing the dosimetric parameters of brachytherapy in the treatment of cervical cancer. Patients with biopsy proven cervical carcinoma, clinically staged as International Federation of Gynecology and Obstetrics (FIGO) IB2-IVA, Eastern Cooperative Oncology Group (ECOG) 0-2, Karnofsky performance scale (KPS) ≥ 70, with satisfactory renal and hematological parameters, and sub-optimal tandem insertion during brachytherapy were eligible for inclusion.
External beam radiotherapy was delivered via volumetric modulated arc therapy (VMAT) to CTV and pelvic nodes, with or without para-aortic nodes (depending on clinical stage and indication as per EMBRACE II protocol [12]). A dose of 45 Gy, 1.8 Gy per fraction was delivered over a period of 5 weeks, followed by cervical interstitial high-dose-rate (HDR) brachytherapy, 28 Gy in 4 fractions, administered twice a week. Total treatment duration was less than 7 weeks.
A response evaluation MRI was carried out after 25th fraction of EBRT, since MR simulation was not available for brachytherapy treatment. Before the procedure, rectal emptying was ensured with bowel emptying or laxatives. The patient was catheterized and plane draped in lithotomy position. Then, a gynecological examination was performed, and findings were documented. Utrecht IC/IS hybrid applicator (Elekta) was used for all insertions. As per protocol, the uterine length was first assessed with a uterine sound. Sub-optimal implantation was clinically assessed. In patients selected for the study, the uterine cavity was unreachable as tandem could not pass beyond internal cervical os. Rectal retractor was inserted, followed by fixation of the whole apparatus using Elekta’s custom built immobilization board. The patient then had a planning CT scan, and needle insertion was done under image guidance. At least 1 out of 4 medial needles was inserted where maximal length could be achieved. Subsequently, the patient’s final planning CT was done.
Target volume delineation of CTV and OARs, i.e., the bladder, rectum, and sigmoid colon, was assessed according to recommendations by Ohno et al. [13]. Doses were then documented in the GEC ESTRO EQD2 charts, and equivalent biological dose (EQD2) was calculated using linear-quadratic model (α/β = 10 for CTV) [9]. Afterwards, 7 Gy fraction dose was delivered to obtain a desired total biologically effective dose (BED) of 90 Gy to CTV D90. A dose of D2cc of the bladder, rectum, and sigmoid of less than 90 Gy, 75 Gy, and 75 Gy, respectively, was deemed acceptable as per American Brachytherapy Society guidelines [14, 15]. During and immediately after the treatment, early toxicity to the bladder, rectum, and sigmoid colon was evaluated, and severity was assessed as per the Common Terminology Criteria for Adverse Events (CTCAE) [16]. CTCAE grade 3 and 4 adverse events were considered significant. Clinical and radiological response was measured 12 weeks after the completion of treatment via gynecological examination and contrast-enhanced pelvis MRI, respectively.
For the purpose of the study, a separate test plan was created for comparison after the patient was treated with every fraction. Medial needles were inactivated, and a new plan using the remaining lateral needles and intra-uterine applicator was made (Figure 2). Doses were recorded for test plans in the same manner as for treatment plans. Data on dose to CTV D90 (the dose given to 90% of CTV) and D2cc of OARs were retrospectively reviewed for treatment plans (subset with medial needle activated), and recorded on the spot for test plans (with medial needles inactivated). Data were analyzed using SPSS version 21.0, and a p-value of less than 0.05 was considered statistically significant. A comparison of dosimetric data of CTV and organs at risk in the two groups (plans with medial needles activated: treated group vs. plans without medial needles activated: test group) was performed using Wilcoxon signed rank test.
Results
A total of 25 hybrid brachytherapy insertions, with sub-optimal insertions in 7 patients, were included in this study. The descriptive statistics are presented in Table 1. The mean dose per fraction to 90% of high-risk (HR) CTV in the plans with medial needles activated was 1.37 Gy more, as compared with the plans without activation of medial needles, leading to a significant improvement in dose coverage for HR-CTV D90 (p = 0.001).
Table 1
Dose per fraction statistics
Figure 3 illustrates the distribution of dose per fraction in CTV and OARs across the two groups. The median CTV dose per fraction was 24.6% higher in the group with medial needles activated (7.08 Gy), as compared with the group with medial needles inactivated (5.68 Gy). However, statistical analysis of the maximum dose to 2 cc (D2cc) of the bladder, rectum, and sigmoid colon for each fraction revealed comparable dosimetric parameters between the two groups (Table 1). The mean total CTV D90 per patient at the completion of treatment was also significantly higher in the group with medial needles activated, with a mean difference of 8.48 Gy per patient between both the groups. Conversely, no significant difference was observed in the total mean D2cc to OAR in each patient between the two groups (Table 2).
Fig. 3
Comparison of the dose per fraction in the CTV and the OARs, with and without the activation of medial needles
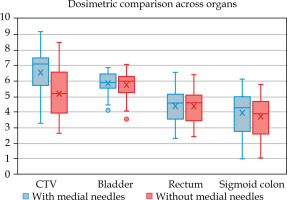
Table 2
Summary of descriptive statistics of cumulative dose per patient across organs after completion of treatment
The details of specific medial needles inserted in patients with sub-optimal tandem insertion are summarized in Table 3. Amongst the medial needles insertions (n = 52), 34 were inserted anteriorly (65.4%). Moreover, 75% of the medial needles inserted (39/52) had more than 2 cm depth. On average, 2 medial needles were used per fraction, accounting for 32% of the total number of needles per fraction (x̄ = 6). The average depth of the medial needles was 3.04 cm (range, 1.5-5 cm).
Table 3
Frequency of specific interstitial medial needles
| Anterior medial needles | Posterior medial needles | Total | |||
|---|---|---|---|---|---|
| Rt: N6 | Lt: N15 | Rt: N10 | Lt: N11 | ||
| Deep medial needles (> 2 cm depth) | 12 | 18 | 6 | 3 | 39 |
| 30 | 9 | ||||
| Total medial needles | 14 | 20 | 9 | 9 | 52 |
| 34 | 18 | ||||
During the treatment, no patient developed CTCAE grade 3 or 4 early toxicity of the bladder, rectum, or sigmoid colon. Twelve weeks after the completion of treatment, response evaluation was performed via contrast-enhanced MRI and local gynecological examination. All the cohort (n = 7) achieved a complete response.
Discussion
In brachytherapy planning, it is crucial to ensure optimal insertion of the tandem and ovoids [17]. Despite the advancements in technique and availability of image guidance, sub-optimal insertion can still occur during the procedure, with its incidence being 6% to 7.5% [18, 19]. Iatrogenic cervical dilation under spinal or general anesthesia can be employed to allow the insertion of the tandem [17]. However, anesthesia, especially general anesthesia, carries a higher risk of complications [11]. Moreover, in resource-limited settings, the logistics of general anesthesia cannot routinely be ensured. Ultrasonography is also being used for real-time image-guided insertion of tandems [20, 21], and for correction of uterine malposition [10]. Ultrasound guidance alone cannot solve the issue of sub-optimal insertion caused by fibrosis or gross tumor obstruction. In situations, where this cannot be corrected even with ultrasound guidance, Lim et al. recommends laparoscopy-assisted tandem placement [10]. Although this is a definitive solution and requires the need for invasive surgery, which has its own set of associated risks, complications, and logistic issues.
In general, in cases where HR-CTV deviates from the usual pear shape or with gross residual disease at the time of procedure, interstitial needles can be used for dose optimization in addition to intra-cavitary applicator [15, 22, 23]. In a cohort study conducted by Laan et al., sub-optimal target coverage was an indication for the insertion of interstitial needles for better dose coverage and OARs sparing [24]. However, the literature lacks needles’ specification regarding dose optimization in cases with sub-optimal tandem insertion. This study shows that interstitial brachytherapy with the insertion of medial needles can offer a minimally invasive dosimetric solution without the requirement of complex invasive surgical techniques, thus, potentially reducing patient morbidity, healthcare burden, and financial toxicity.
We observed that with the utilization of medial needles, there was a significant improvement not only in CTV dose per fraction, but also in total CTV dose for individual patient at the end of the treatment. A mean increase of 8.5 Gy per patient can potentially provide a significant survival advantage. This suggests that the insertion of medial needles can indeed considerably improve the dosimetric parameters of clinical target volume, resulting in better clinical outcomes, as demonstrated by complete response in all our patients.
On the other hand, the comparison between the two groups across OARs revealed statistically insignificant differences, despite a significant increase in the CTV dose with medial needles activated. This was because we focused on maximally increasing the CTV dose while keeping D2cc of OAR within limits. Therefore, no change in OAR doses should be expected with current scheme of this study. Also, no patient developed clinically significant early toxicity in OARs during and up to 3 months after the treatment, thus, justifying the current approach. Medial needle insertion was most frequently done anteriorly (65.4%) than posteriorly (34.6%). A possible reason for this difference is that the bladder was most frequently at the risk of toxicity, and the rectum was relatively spared due to naturally anteflexed uterine fundus in most cases. This resulted in more depth available anteriorly for needle insertion. Unlike the bladder and rectum, the sigmoid colon had a variable location due to its mesocolon, while the position of the uterus did not seem to affect its dose.
Conversely, one fraction in one of the subjects had unexpected results. The dose parameters improved when needles were inactivated. In the treatment plan with medial needles activated, the CTV D90 was 3.47 Gy, D2cc bladder was 5.84 Gy, D2cc rectum was 2.68 Gy, and D2cc sigmoid was 4.35 Gy. In the plan with medial needles inactivated, the CTV D90 was 5.77 Gy, D2cc bladder was 5.18 Gy, D2cc rectum was 3.15 Gy, and D2cc sigmoid was 4.33 Gy. It was observed that the bladder was the dose limiting organ, and medial needle inserted (N15 – anterior medial) was more of a cause of increased bladder toxicity than optimizing CTV coverage. In such clinical scenarios, more caution is necessary, therefore, oncologists and physicists should be open to the possibility of both kinds of situations during brachytherapy treatment planning.
To date, only a few studies have been conducted to address the issue of sub-optimal tandem insertion in cervical brachytherapy. The current study is the first of its kind to evaluate the potential use of medial needles for dose compensation in patients with sub-optimal tandem insertion. Furthermore, our study employs a matched-pair design for dosimetric comparison, i.e., for the creation of a test plan for comparison, each treatment plan (with medial needle inserted) was re-planned after inactivation of medial needles. So, for every fraction, both plans for comparison were made on the same planning CT. This eliminated the likelihood of many confounding factors, including in-patient and between-patient variations.
The clinical outcomes, however, were not prospectively identified. Retrospective nature of data and the absence of control group limits the ability of the study to establish definitive correlation between the insertion of medial needles and clinical outcomes. Another limitation is the small sample size. Moreover, the test plans were created for comparison purposes only. In the clinical setting, unavailability of medial needles may require the treating oncologist to employ other methods for dose compensation (e.g., deeper insertion of lateral needles or increase in number of lateral needles activated). Therefore, in the test group, the planned dose might not be entirely representative of the likely dose in the real-life setting, causing a potential measurement bias that may lead to an overestimation of the dose differences amongst the two groups.
Conclusions
In patients with sub-optimal tandem insertion after cervical interstitial brachytherapy, the insertion of medial needles can significantly improve CTV dosimetry without compromising OARs dose constraints. Further studies among larger cohorts are needed to validate these findings and to optimize treatment protocols.




