Introduction
Splenosis was first described by Albrecht in 1896 and subsequently named by Buchbinder and Lipkoff in 1939 [1]. Splenosis is defined as the autotransplantation of viable splenic tissue throughout various anatomic compartments of the body. Previous splenectomy, abdominal trauma or splenic rupture predisposes to splenosis [2]. Intra-abdominal splenosis involving the serosal surface of the small or large bowel, parietal peritoneum and mesentery is relatively common [3]. However, intrahepatic splenosis (IHS) is rare, with many authors quoting fewer than 50 cases published to date [4-6]. Diagnosis of IHS is often challenging as patients are often asymptomatic or present with non-specific abdominal pain, and radiological imaging findings may resemble other hepatic lesions, particularly hepatocellular carcinoma (HCC), adenoma and focal nodular hyperplasia (FNH). With the increase in abdominal imaging for patients with vague abdominal symptoms and better quality of imaging technology, incidental liver lesions are common. Once a liver lesion is detected, a clinician is faced with a challenge to diagnose the lesion with certainty with the primary goal of ruling out a malignancy. IHS is a benign condition and does not warrant surveillance or intervention unless the patient is severely symptomatic. Definitive diagnosis of IHS is possible with percutaneous needle biopsy, intra-operative frozen section or post-operative histopathological analysis or technetium-99m-tagged (Tc-99m) heat-damaged red blood cell (RBC) scintigraphy. However, patients undergoing additional diagnostic tests may bear unnecessary costs and morbidity. This is compounded by anxiety associated with the waiting interval or knowledge of false negative reports. Hence it is important to understand this pathological condition and its clinical features. To date, there are two literature reviews on IHS which summarize reported cases [4, 7]. However, these reviews do not include the clinical presentation, presence of risk factors for malignancy, laboratory investigations and imaging characteristics. This study aims to provide a comprehensive overview on IHS.
Material and methods
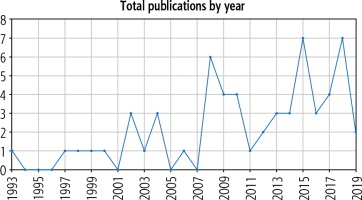
A literature review was performed on PubMed database for the keywords “intrahepatic splenosis” OR “hepatic splenosis” from the period of 1939 to 2019. The last search was performed on 18 January 2020. The search yielded 81 articles: 11 articles were not in English, 6 articles were not case reports or series, 5 articles included isolated extrahepatic splenosis, 1 article was on splenosis in animals, 1 article included an incidental finding of splenosis on autopsy, and the full text was not available for 1 article. The remaining 56 articles were included in the analyses, with a total of 59 reported cases (Table 1) [4-59]. Year of study, age, sex, reason for splenectomy, time from splenectomy to presentation, presence of risk factors for HCC, clinical presentation, laboratory investigation results, imaging features, initial differential diagnoses and method of confirming diagnosis were extracted from the articles. Figure 1 is a graphical representation of the trend of reporting of cases of IHS, which shows an increasing trend in reporting.
Table 1
Summary of 59 reported cases of intrahepatic splenosis from 1939 to 2019
| No. | Year | First author | Age/ Sex | Reason for splenectomy | Time* (years) | Risk factor for HCC | Clinical presentation | Laboratory investigations# | No. of lesions | Location | Size (cm) | Initial diagnosis | Confirmatory diagnosis |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1993 | Yoshimitsu [8] | 51/F | Banti syndrome | 23 | Cirrhosis | Asymptomatic | ALP elevated | 1 | S3 | 2.5 | HCC | Surgery (liver resection) |
| 2 | 1997 | Gruen [9] | 38/F | Trauma | 20 | Fatty liver | Asymptomatic | ALT, AST, ALP, bilirubin elevated | 1 | S3, S4 | 3.9 | HCC/FNH | Surgery (liver resection) |
| 3 | 1998 | D’Angelica [10] | 38/F | Trauma | 20 | Alcohol | Asymptomatic | ALT, AST, ALP, GGT, bilirubin elevated | 1 | S3, S4 | 2.5 | Adenoma/FNH | Surgery (liver resection) |
| 4 | 1999 | Foroudi [11] | 59/F | NM | 47 | Nil | Upper abdominal pain and back pain | Normal | Multiple | Right lobe | NM | Liver metastasis | Tc-99m DRBC |
| 5 | 2000 | De Vuysere [12] | 50/M | Trauma | 34 | Nil | Epigastric pain | Normal | Multiple | S2 | 6 | Hepatic splenosis | Surgery (biopsy) |
| 6 | 2002 | Gamulin [13] | 49/M | Trauma | 37 | Nil | Asymptomatic | Normal | 1 | Left lobe | 6.6 × 4.2 | B-cell lymphoma | Surgery (explorative laparotomy) |
| 7 | 2002 | Lee [14] | 43/M | Trauma | 20 | HBV Cirrhosis | Asymptomatic | Normal, except for INR | 1 | S6 | 3.5 | HCC | Surgery (liver resection) |
| 8 | 2002 | Pekkafali [15] | 21/M | Trauma | 15 | Nil | Epigastric pain | Normal | 1 | Left lobe | 3.4 × 2.3 | Hepatic splenosis | Tc-99m DRBC |
| 9 | 2003 | Kim [16] | 43/M | Trauma | 21 | HBV Cirrhosis | Asymptomatic | Normal | 1 | S6 | 3 | HCC | Surgery (liver resection) |
| 10 | 2004 | Di Costanzo [17] | 58/M | Trauma | 46 | HBV Cirrhosis | Abdominal pain | AFP elevated | 1 | S2 | 4.8 | HCC | Needle biopsy, Tc-99m DRBC |
| 11 | 48/F | Trauma | 41 | HCV Cirrhosis | Asymptomatic | ALT, AST and AFP elevated | 1 | S3 | 3.1 | HCC | US-guided biopsy | ||
| 12 | 2004 | Kondo [18] | 55/M | Trauma | 31 | HCV | Asymptomatic | NM | 1 | S7 | 3.5 | HCC/FNH/ haemangioma | US-guided percutaneous biopsy |
| 13 | 2006 | Ferraioli [19] | 40/M | Trauma | 28 | HCV | Asymptomatic | Normal | 1 | S7 | 6 × 3.1 | Hepatic splenosis | US-guided biopsy |
| 14 | 2008 | Choi [20] | 32/M | Trauma | 26 | HBV carrier | Asymptomatic | AST elevated | Multiple | S4a, S6 | 1.0-3.0 | HCC | Surgery (explorative laparotomy) |
| 15 | 2008 | Grande [21] | 41/M | Trauma | 35 | Nil | Asymptomatic | Normal | Multiple | S7 | 0.5-4.5 | Hepatic splenosis | Tc-99m DRBC |
| 16 | 2008 | Imbriaco [22] | 39/M | Trauma | 24 | Nil | Abdominal pain | NM | Multiple | Left and right lobes, pancreatic tail, adjacent to upper pole of left | 3.0 | Neoplasm | Surgery (explorative laparotomy) |
| 17 | 2008 | Lu [23] | 59/M | Trauma | NM | HBV | Asymptomatic | Normal | Multiple | S7, left lobe | 1.2-2.2 | Hepatic splenosis | Tc-99m DRBC |
| 18 | 2008 | Nakajima [24] | 41/M | Trauma | 21 | Nil | Incidental finding on work-up for acute enteritis | NM | 1 | S6 | NM | Hepatic splenosis | US-guided biopsy |
| 19 | 2008 | Yeh [25] | 64/M | Trauma | 8 | HCV | Asymptomatic | ALT, AST elevated | 1 | S6 | 2.5 | HCC | Surgery (liver resection) |
| 20 | 2009 | Hilal [26] | 60/M | Trauma | 46 | Cirrhosis | Flu-like symptoms, loss of weight, loss of appetite | LFT deranged, AFP elevated | Multiple | S7 | 2 × 2.5 and 4.5 | HCC | Explorative laparoscopy |
| 21 | 2009 | Kashgari [27] | 52/M | Trauma | 30 | HCV Cirrhosis | Asymptomatic | ALT, AST elevated | 1 | S7 | 2.1 × 1.5 | HCC | US-guided biopsy |
| 22 | 2009 | Menth [28] | 43/M | Trauma | 25 | HCV Cirrhosis | Asymptomatic | ALT, AST elevated | Multiple | S2 | 0.4-3.6 | HCC | Tc-99m DRBC |
| 23 | 2009 | Yu [29] | 54/M | Trauma | 20 | Nil | Asymptomatic | Normal | 1 | S2 | 4 | Uncertain | Surgery (liver resection) |
| 24 | 2010 | Mescoli [30] | 68/F | No splenectomy | NA | Cirrhosis | Abdominal pain | NM | Multiple | S3, S5, S7 | 6.2-11 | FNH/ haemangioma | Percutaneous biopsy |
| 25 | 54/M | Iatrogenic | 12 | Nil | Asymptomatic | NM | 1 | Left lobe | 3 | Liver metastasis | Surgery (explorative laparotomy) | ||
| 26 | 2010 | Tsitouridis [31] | 63/M | Trauma | 20 | Nil | RUQ pain | NM | 1 | Left lobe | 8 | Splenosis | CT-guided biopsy |
| 27 | 64/M | Gastric leiomyo-sarcoma | 1.5 | Nil | Asymptomatic | NM | 1 | NM | 5 | Peritoneal implantation | CT-guided biopsy | ||
| 28 | 2011 | Kang [32] | 54/M | Trauma | 15 | Nil | Asymptomatic | Normal | 2 | S2 | 0.7 × 0.6, 2.3 × 1.9 | Liver metastasis | Surgery (liver resection) |
| 29 | 2012 | Li [33] | 61/M | Trauma | NM | Nil | Asymptomatic | NM | Multiple | NM | NM | Hepatic splenosis | Needle biopsy |
| 30 | 2012 | Liu [7] | 38/M | Trauma | 14 | HBV | Asymptomatic | Normal | 1 | S2 | 3.3 × 2.7 | Liver tumour | Surgery (laparoscopic resection) |
| 31 | 2013 | Inchingolo [34] | 53/M | Trauma | 33 | NASH | Asymptomatic | GGT elevated | 1 | S3 | 3.5 | HCC/adenoma | Surgery (laparoscopic converted to open liver resection) |
| 32 | 2013 | Krawczyk [35] | 39/F | Trauma | NM | Nil | Abdominal pain | NM | 2 | S2, adjacent to major curvature of stomach | 3.2 × 2.0 | Adenoma | Tc-99m DRBC |
| 33 | 2013 | Leong [36] | 56/M | Trauma | NM | Nil | Chronic epigastric pain | NM | 1 | S3 | 3.7 × 4.6 × 3.1 | Carcinoid neuroendocrine tumour | Surgery (liver resection) |
| 34 | 2014 | Kandil [37] | 45/F | Haemolytic anaemia | 20 | HCV | Chronic abdominal pain | Normal | 1 | Left lobe | 5 × 4 | HCC | Surgery (explorative laparotomy) |
| 35 | 2014 | Sato [38] | 58/M | No splenectomy | NA | HCV Cirrhosis | Asymptomatic | ALT, AST, AFP elevated | 1 | Right lobe | 3.9 × 3 | HCC | Surgery (liver resection) |
| 36 | 2014 | Tinoco Gonzalez [39] | 60/M | Trauma | NM | HCV | Asymptomatic | NM | 1 | S3 | 4.8 | HCC/ Adenoma | Surgery (liver resection) |
| 37 | 2015 | Grambow [40] | 53/M | Trauma | 9 | Alcohol Cirrhosis | Incidental finding due to refractory ascites secondary to decompensated cirrhosis | Normal | 1 | S3, S4b | 3.5 | HCC | Surgery (laparotomy) |
| 38 | 2015 | Li [41] | 67/F | Trauma | 5 | HCV Cirrhosis | Asymptomatic | LFT deranged, AFP elevated | 1 | Left lobe | NM | HCC | Surgery (explorative laparotomy) |
| 39 | 2015 | Liu [6] | 33/M | Trauma | 30 | Nil | Asymptomatic | Normal | Multiple | Left and right lobes | 4.2 × 3.0 | HCC | FNA biopsy |
| 40 | 2015 | Tamm [42] | 43/M | Trauma | NM | Nil | RUQ pain | NM | 1 | S3 | 2.8 | Nil | Tc-99m DRBC |
| 41 | 2015 | Toktas [43] | 40/F | Idiopathic thrombocytopenic purpura | 7 | Nil | Asymptomatic, persistent low platelets | NM | 1 | S2/S3 | 7.0 × 3.0 | Nil | Surgery (liver resection) |
| 42 | 2015 | Wu [44] | 33/M | Trauma | 12 | Nil | Asymptomatic | Bilirubin elevated | 1 | S2 | 3.5 × 2.0 | HCC | Surgery (explorative laparotomy) |
| 43 | 2016 | Fung [45] | 55/M | Trauma | 37 | Nil | Asymptomatic | Normal | 2 | S6, S7 | 2.27 × 3.04 and 1.15 × 1.21 | Nil | Surgery (liver resection) |
| 44 | 2016 | Chen [46] | 51/M | Trauma | 20 | Nil | Asymptomatic | NM | 2 | Left and right lobes | 2.1; 3.3 × 2.6 | HCC | US-guided biopsy |
| 45 | 2016 | Jereb [47] | 22/M | Trauma | 18 | Nil | Asymptomatic | Normal | Multiple | S2, S6, S7 | 2.6 | Liver metastases | Surgery (explorative laparoscopy) |
| 46 | 2017 | Keck [48] | 66/M | NM | NM | Chronic HCV | Asymptomatic | Normal | Multiple | S7, S8 | 5.3 | Nil | Needle biopsy |
| 47 | 2017 | Somsap [49] | 51/M | Thalassemia | 20 | Nil | Abdominal pain | ALT, AST, bilirubin elevated | 1 | Left lobe | NM | HCC | Surgery (liver resection) |
| 48 | 2017 | Wang [5] | 54/M | Trauma | 23 | Chronic HBV | RUQ pain | Normal | 1 | Right lobe | 3.9 × 3.6 | HCC | Surgery (liver resection) |
| 49 | 2017 | Wang [50] | 42/M | Trauma | 16 | HBV, HCV, fatty liver | Chronic low back pain | Normal | 1 | S4 | 2.3 × 1.8 | HCC | Surgery (liver resection) |
| 50 | 2018 | Aramoana [51] | 58/M | Trauma | 37 | Nil | RUQ pain | Normal | 1 | S6 | 4.6 × 3.4 | HCC | Surgery (liver resection) |
| 51 | 2018 | Budak [52] | 46/M | Trauma | 30 | Nil | NM | NM | 2 | S6, S7 | 3.6 | HCC/hepatic splenosis | Tc-99m DRBC |
| 52 | 2018 | Guzman [53] | 43/M | Trauma | 16 | Nil | Acute RUQ pain | ALT, AST elevated | 1 | S2 | 2.5 | Adenoma | Percutaneous needle biopsy |
| 53 | 2018 | Smolen [54] | 35/M | Trauma | 12 | Nil | Chronic abdominal pain | Normal | Multiple | Left and right lobes | 4.3 | Adenoma/FNH | Tc-99m DRBC |
| 54 | 2018 | Teles [55] | 73/M | NM | NM | Nil | Low back pain | CEA elevated | Multiple | Left and right lobes, lumbar spine | 4.9 | Primary or secondary neoplasia | Surgery (open liver resection) |
| 55 | 2018 | Varghese [56] | 50/M | Trauma | 40 | Nil | Asymptomatic | NM | 1 | Right lobe, multiple extrahepatic nodules | 3.0 | Nil | Contrasted CT scan resembling splenic enhancement and clinical judgement |
| 56 | 2018 | Vergara [57] | 69/M | Trauma | NM | Nil | RUQ pain, dyspnoea, lower limb oedema | Normal | Multiple | S6, near falciform ligament, left para-vesical space | 6.5 × 4.6 | Nil | Needle biopsy |
| 57 | 2018 | Xuan [58] | 54/M | Trauma | 5 | Nil | Asymptomatic | Normal | 1 | S4 | 4.5 × 3.3 | HCC | Surgery (liver resection) |
| 58 | 2019 | Guedes [59] | 68/M | Trauma | 44 | Nil | Chronic epigastric and right hypochondrium pain | Normal | 1 | S6 | 3.0 | HCC/Adenoma | Surgery (laparoscopic liver resection) |
| 59 | 2019 | Luo [4] | 41/M | Trauma | 21 | Nil | Asymptomatic | 1 | Right lobe | NM | HCC | Surgery (explorative la |
AFP – α-fetoprotein, ALP – alkaline phosphatase, ALT – alanine aminotransferase, AST – aspartate aminotransferase, CT – computed tomography, F – female; FNA – fine needle aspiration, FNH – focal nodular hyperplasia, GGT – γ-glutamyltransferase, HCC – hepatocellular carcinoma, INR – international normalized ratio, LFT – liver function test, M – male, NA – not applicable, NM – not mentioned, RUQ – right upper quadrant, S1-S7 – segments I to VII of the liver, Tc-99m DRBC – technetium-99m-tagged heatdamaged red blood cell scan, US – ultrasound
Results
Fifty-nine patients with IHS are reported with male predominance (n = 49, 83.1%) and a median age of 51 years (range 21-73 years). The majority of the patients had a prior history of splenectomy (n = 57, 95.0%). Two patients did not have any history of abdominal trauma or splenectomy. The median time from splenectomy to diagnosis of splenosis was 21 years (range 1.5-47 years). Reported risk factors for HCC were as follows: 1) hepatitis B (n = 8, 13.6%), 2) hepatitis C (n = 12, 20.3%), 3) heavy alcohol use (n = 2, 3.4%), 4) fatty liver (n = 3, 5.1%) and 5) cirrhosis (n = 12, 20.3%). 33 (55.9%) patients did not have any of the abovementioned risk factors for HCC. The majority of the patients were asymptomatic (n = 37, 62.7%). 19 patients (32.2%) presented with abdominal pain and/or discomfort and 3 patients (5.1%) had atypical presentations: 1 patient had flu-like symptoms, loss of weight and loss of appetite and 2 patients had chronic lower back pain.
Many of the reported cases do not include the essential laboratory investigations such as alanine aminotransferase (ALT), aspartate aminotransferase (AST) and α-fetoprotein (AFP). Of those cases which included these investigations, 12 out of 36 patients (33.3%) had transaminitis, and 6 out of 34 patients (17.6%) had raised AFP. The majority of the reported cases were isolated IHS; 4 (6.8%) of the cases included both intrahepatic and extrahepatic splenosis. The specific imaging features and patterns of enhancement can be found in the appendix (Table 2).
Table 2
Patterns of enhancement on imaging of all cases (n = 59) of intrahepatic splenosis from 1939 to 2019
| No. | Year | Author | CT findings | MRI findings | Angiography |
|---|---|---|---|---|---|
| 1 | 1993 | Yoshimitsu [8] | Non-contrast: homogeneous low attenuation mass Contrast: enhanced from the periphery in the early phase, low attenuation in the delayed phase | T1-W: homogeneously low intensity T2-W: not obtained PDI: high intensity | Mass supplied by the left hepatic artery No definite neovascularity |
| 2 | 1997 | Gruen [9] | Contrast: high-attenuation mass | NA | NA |
| 3 | 1998 | D’Angelica [10] | Contrast: high-density mass | NA | NA |
| 4 | 1999 | Foroudi [11] | Contrast: multiple foci of enhancing soft tissue densities | NA | NA |
| 5 | 2000 | De Vuysere [12] | Non-contrast: slightly hypodense Contrast: homogeneously hyperdense in the arterial phase, isodense in the portal venous phase, and slightly hypodense in the late phase | Pre-contrast T1-W: hypointense Pre-contrast T2-W: hyperintense Post-contrast (small iron oxide particles (SPIO-Endorem): remained slightly hyperintense relative to the hypointense liver | NA |
| 6 | 2002 | Gamulin [13] | Contrast: heterogeneous enhancement | NA | NA |
| 7 | 2002 | Lee [14] | Contrast: early contrast enhancement and washout on delayed phase | NA | Tumour stained in segment 6 through the inferior phrenic artery No feeding vessel from hepatic or superior mesenteric artery |
| 8 | 2002 | Pekkafali [15] | Non-contrast: slightly hypodense with prominent hypodense rim around the lesion Contrast: hyperdense in the arterial phase, isodense in the portal venous phase and hypodense in the equilibrium phase | Pre-contrast T1-W: homogenously hypointense with hypointense rim Pre-contrast T2-W: isointense to liver with thin hypointense rim Post-contrast: hyperintense to liver | NA |
| 9 | 2003 | Kim [16] | Contrast: homogeneously well enhanced in the arterial phase and isodense in the equilibrium phase | NA | Mass supplied by inferior phrenic artery |
| 10 | 2004 | Di Costanzo [17] | Contrast: arterial hypervascularization and rapid “washout” of the contrast medium on portal venous phase | NA | NA |
| 11 | Contrast: early enhancement on the arterial phase and complete “washout” of the lesion on portal venous phase | NA | NA | ||
| 12 | 2004 | Kondo [18] | Contrast: low-density tumour in arterial phase, with vessels penetrating inside the tumour. Nearly homogeneous enhancement | T1-W: low signal intensity T2-W: high signal intensity | Hypervascular tumour supplied by the right hepatic artery |
| 13 | 2006 | Ferraioli [19] | NA | Contrast material-enhanced T1-W: liver tumour and accessory spleen were hypointense T2-W: liver tumour and accessory spleen were hyperintense | NA |
| 14 | 2008 | Choi [20] | Contrast: Lesion in segment IVa: slight enhancement during both the arterial and portal phase Lesion in segment VI: slight enhancement only in the portal phase | Contrast: enhancement during arterial phase and slightly hyperintense signal in the liver parenchyma during portal phase | Subtle tumour staining in segment IVa and no tumour staining in segment VI |
| 15 | 2008 | Grande [21] | Non-contrast: slightly hypodense compared to the liver Contrast: hyperdense in the arterial phase and isodense in the portal phase | NA | NA |
| 16 | 2008 | Imbriaco [22] | Non-contrast: hypodense Contrast: heterogeneous enhancement in the arterial phase, hypodense compared with the surrounding parenchyma during the portal and equilibrium phases | Pre-contrast T1-W: hypointense Pre-contrast T2-W: slightly hyperintense Post-contrast: nonhomogeneous enhancement during the arterial phase, hypointensity during the portal and equilibrium phases | |
| 17 | 2008 | Lu [23] | Non-contrast: two hypodense nodules Contrast: homogeneously hyperdense in the arterial phase, isodense in the portal venous phase, and slightly hypodense in the equilibrium phase. | Pre-contrast T1-W: homogeneously hypointense Pre-contrast T2-W: hyperintense contrast (Gd-DTPA): global enhancement in arterial phase, isointense in portal phase | |
| 18 | 2008 | Nakajima [24] | Non-contrast: hypodense mass Contrast: strong enhancement at the early phase and pooling enhancement at the late phase | T1-W: hypointense mass T2-W: hypointense mass | |
| 19 | 2008 | Yeh [25] | Non-contrast: isodense Contrast: persistent homogeneous enhancement in the arterial and portal venous phases | Pre-contrast T2-W: intermediate to high signal Plain phase: iso-signal in the plain phase Post-contrast: heterogeneous enhancement in the arterial phase and persistent homogeneous enhancement in the portal venous phase | Tumour stain with blood supply via perirenal vessel |
| 21 | 2009 | Kashgari [27] | NA | Pre-contrast T1-W: mildly hypointense Pre-contrast T2-W: homogenously hyperintense Contrast (gadopentetate dimeglumine): heterogenous early arterial enhancement, isointense in porto-venous and equilibrium phase | NA |
| 20 | 2009 | Hilal [26] | Contrast: hypervascular nodule with increased enhancement in the venous phase | Contrast (gadolinium): hypervascular nodule in arterial and portal venous phase | NA |
| 22 | 2009 | Menth [28] | NA | Contrast (Gd-DTPA): marked enhancement in early arterial phase Contrast (SPIO) T2-W: lacks iron uptake | Regular branches of hepatic artery No pathologic vessels or parenchymal foci of hypervascularity |
| 23 | 2009 | Yu [29] | Contrast: strong and slightly inhomogeneous enhancement in the arterial phase, diminished enhancement in the portal venous phase | T1-W: hypointense T2-W: | |
| 24 | 2010 | Mescoli [30] | Contrast: hyper-enhancement in arterial and portal phases The largest nodule showed a hypodense central (necrotic) area | NA | NA |
| 25 | Contrast: hypervascular nodule | NA | NA | ||
| 26 | 2010 | Tsitouridis [31] | Non-contrast: slightly hypodense Contrast: increased enhancement during arterial phase with hypodense rim surrounding lesion. Lesion is isodense during portal phase | Pre-contrast T2-HASTE: intermediate-to-high signal intensity Post-contrast T2-HASTE: homogeneous enhancement with imaging characteristics of an extrahepatic-intraperitoneal lesion | NA |
| 27 | Contrast: hypodense with peripheral enhancement in both arterial and portal phases | Pre-contrast T2-HASTE: intermediate-to-high signal Post-contrast T2-HASTE: delayed peripheral enhancement Coronal plane: imaging characteristics of an extrahepatic lesion mimicking peritoneal implantation | NA | ||
| 28 | 2011 | Kang [32] | No parenchymal abnormality in liver | T1-W: low signal intensity T2-W: slightly high signal intensity slightly high signal intensity on the SPIO-enhanced T2-W: high signal intensity | NA |
| 29 | 2012 | Li [33] | Non-contrast: isodense masses mirroring residual spleen Contrast: enhancement in both hepatic mass and residual spleen | Pre-contrast T1-W: hypointense Pre-contrast T2-W: hyperintense Contrast: heterogeneous enhancement in arterial phase | NA |
| 30 | 2012 | Liu [7] | Non-contrast: homogeneous soft tissue mass with surrounding low-density aureole Contrast: slightly lower density than the liver especially in arterial phase | NA | NA |
| 31 | 2013 | Inchingolo [34] | Contrast: marked enhancement in arterial phase, remained hyperdense in portal venous phase | Post-contrast (gadolinium): increased arterialization after gadolinium injection with some loss of signal in the in-phase, indicating hemosiderin accumulation in the tissue DWI: restricted diffusion within the lesion | NA |
| 32 | 2013 | Krawczyk [35] | NI | Pre-contrast T2-W: hyperintense lesion in liver, with additional lesions dorsal to stomach that looks typical for regenerate spleen tissue Post-contrast T1-W: homogeneous enhancement | |
| 33 | 2013 | Leong [36] | Hypervascular lesion | Non-cystic irregular lesion with features suggestive of neuroendocrine tumour | |
| 34 | 2014 | Kandil [37] | Contrast: enhancement in arterial phase | NA | NA |
| 35 | 2014 | Sato [38] | Contrast: slightly inhomogeneous enhancement in arterial phase, with diminished enhancement in the equilibrium phase | Pre-contrast T2-W: hyperintense Post-contrast (Gd-EOB): hypointense compared to surrounding liver parenchyma | NA |
| 36 | 2014 | Tinoco | NA | Hypervascular lesion | NA |
| [39] | Contrast: homogeneous enhancement in arterial phase, with | ||||
| lavage in the portal phase and equilibrium | |||||
| 37 | 2015 | Grambow | Contrast: hypervascular mass with enhancement typical for HCC | NA | NA |
| [40] | |||||
| 38 | 2015 | Li [41] | Contrast: strong homogeneous enhancement in arterial phase and | Pre-contrast T1-W: slightly hyperintense | Hypervascular tumour supplied by the |
| hypodense during portal phase | Pre-contrast T2-W: slightly hyperintense | branches of the hepatic artery | |||
| Post-contrast T2-W: hyperintense during arterial phase and | |||||
| hypointense during the portal phase | |||||
| 39 | 2015 | Liu [6] | NI | T2-W: intermediate-to-high signal intensity | NA |
| 40 | 2015 | Tamm | Non-contrast: slightly hypodense | Pre-contrast T1-W: hypointense | |
| [42] | Contrast: hypodense during arterial phase and hyperdense during | Pre-contrast T2-W: mildly hyperintense | |||
| portal venous phase | Post-contrast: no brisk arterial enhancement was present after | ||||
| contrast administration. Presence of homogeneous enhancement | |||||
| at 1 minute, with central washout and a residual rim of peripheral | |||||
| enhancement at 5 minutes | |||||
| 41 | 2015 | Toktas [43] | Isodense with spleen | NA | NA |
| 42 | 2015 | Wu [44] | Non-contrast: homogeneous hypodense mass | T1-W: low signal intensity | NA |
| T2-W: high signal intensity | |||||
| 43 | 2016 | Fung [45] | Contrast: early arterial enhancement with | Pre-contrast T1-W: hypointense | NA |
| contrast washout in delayed phase | Pre-contrast T2-W: hyperintense | ||||
| Post-contrast T2-W: enhancement in arterial phase followed by | |||||
| washout in delayed phase | |||||
| 44 | 2016 | Chen [46] | Contrast: marked | Pre-contrast T1-W: low signal intensity | NA |
| enhancement at arterial phase and delayed phase | Post-contrast T1-W: lower enhancement after contrast | ||||
| administration | |||||
| 45 | 2016 | Jereb [47] | Contrast: hypodense lesions in portal phase | Post-contrast T1-W: hypointense in both arterial and late phase | NA |
| Post-contrast T2-W: hyperintense during arterial phase, | |||||
| hypointense in late phase | |||||
| 46 | 2017 | Keck [48] | NA | Arterial enhancement with washout | NA |
| 47 | 2017 | Somsap | NA | Pre-contrast T1-W: hypointense | NA |
| [49] | Post-contrast T1-W: heterogenous enhancement during arterial | ||||
| phase, more homogeneous in portal and delayed phase | |||||
| 48 | 2017 | Wang [5] | Non-contrast: hypodense | Pre-contrast T1-W: slightly hypointense | NA |
| Contrast: strong homogeneous enhancement in arterial phase and | Pre-contrast T2-W and DWI: high signal intensity | ||||
| hypodense during portal phase | Post-contrast T2-W: uneven enhancement with decreased signal | ||||
| 49 | 2017 | Wang [50] | Contrast: marked homogeneous enhancement in arterial and portal | Pre-contrast T1-W: hypointense | NA |
| venous phase, with diminished enhancement in the equilibrium phase | Pre-contrast T2-W: hyperintense | ||||
| Post-contrast: moderate homogeneous enhancement with marked | |||||
| delayed ring enhancement mimicking a pseudocapsule similar to | |||||
| hepatocellular carcinoma (HCC) in equilibrium phase | |||||
| 50 | 2018 | Aramoana | Contrast: enhancement in arterial phase | Post-contrast T2-W: peak enhancement at 60 s and washout | NA |
| [51] | at 10 min | ||||
| 51 | 2018 | Budak | NA | T2-HASTE: hyperintense | NA |
| [52] | Post-contrast T1-W: hepatic lesion showed marked enhancement | ||||
| in arterial phase. Multiple nodule formations in peritoneal cavity | |||||
| similarly showed similar contrast uptake pattern | |||||
| 52 | 2018 | Guzman | NI | NI | NA |
| [53] | |||||
| 53 | 2018 | Smolen | Non-contrast: multiple isodense lesions | NA | NA |
| [54] | Contrast: hyperenhancement in arterial phase, iso- to | ||||
| hypoenhancement in portal and delayed phase) | |||||
| Carcinoma could not be ruled out | |||||
| 54 | 2018 | Teles [55] | NI | NI | NA |
| 55 | 2018 | Varghese | Contrast: heterogeneous “arciform” enhancement in arterial phase, | NA | NA |
| [56] | with continued homogeneous enhancement in delayed phase with | ||||
| slow washout | |||||
| 56 | 2018 | Vergara | Contrast: mild enhancement in arterial phase | Pre-contrast T1-W: low signal intensity | NA |
| [57] | Pre-contrast T2-W: slightly hyperintense | ||||
| Post-contrast T1-W: lower enhancement compared surrounding | |||||
| liver parenchyma | |||||
| 57 | 2018 | Xuan [58] | Non-contrast: slightly hypodense | Pre-contrast T1-W and T2-W: slightly hypointense | NA |
| Contrast: inhomogeneous enhancement during arterial phase and | DWI: slightly hyperintense | ||||
| diminished enhancement during the portal and equilibrium phase | Post-contrast: strongly heterogeneous and hyperintense during | ||||
| the arterial phase and relatively hypointense during the portal | |||||
| 58 | 2019 | Guedes | NA | Pre-contrast T1-W: hypointense | NA |
| [59] | Pre-contrast T2-W: hyperintense | ||||
| Post-contrast: increased vascularity and washed out during late | |||||
| venous phase | |||||
| 59 | 2019 | Luo [4] | Non-contrast: multiple hypodense lesions | NA | NA |
| Contrast: enhancement during arterial phase with hypodense rim |
HCC was considered the initial diagnosis in 29 patients (49.2%). IHS was considered as the primary diagnosis in 9 patients (15.3%). There were several reported modalities for confirmatory diagnoses: open liver resection (n = 21, 35.6%), laparoscopic liver resection (n = 2, 3.4%), explorative laparotomy (n = 7, 18.9%), explorative laparoscopy (n = 3, 5.1%), percutaneous needle biopsy (n = 15, 25.4%), and Tc-99m denucleated RBC scintigraphy (n = 10, 16.9%). One patient (1.7%) only had the contrasted CT scan resembling splenic enhancement and was diagnosed with IHS based on the clinical history of splenectomy and absence of risk factors for HCC [56].
Discussion
Splenosis is an acquired condition and is defined as the autotransplantation of splenic tissue following abdominal or splenic trauma or splenectomy, displacing fragmented splenic tissues which may subsequently regrow at implanted sites by acquiring a vascular supply. It has been suggested that local hypoxia induced by hepatic diseases and/or aging may induce splenic erythropoiesis of previously seeded tissues [60]. This is in contrast to an accessory spleen, which is a congenital condition due to the failure of embryological fusion of the splenic primordium and arises from the left side of the dorsal mesogastrium [2, 38].
The major dilemma in the diagnosis of IHS is the need for exclusion of malignancy such as HCC or liver metastases. Radiological findings for IHS mimic the hallmarks of HCC: hyperenhancement in the arterial phase with delayed washout in the portal venous phase and low signal intensity in the hepatobiliary phase [61]. In the presence of risk factors such as hepatitis B, hepatitis C, heavy alcohol use and/or cirrhosis, primary liver malignancy such as HCC should always be excluded. Our study shows that the majority of the patients present with incidental liver lesions and do not have risk factors for HCC. In this group of patients, IHS should be considered and non-invasive or minimally invasive methods of confirmatory diagnosis should be explored. A non-invasive method to confirm the diagnosis of splenosis is the use of Tc-99m heat-damaged RBC scintigraphy [9]. This involves in vitro labelling of the patient’s RBC with Tc-99m, heating the RBC at 49ºC for 20 minutes, and subsequently injecting the patient with the Tc-99m labelled heatdamaged RBC and imaging with planar and singlephoton emission computed tomography (SPECT) 30 minutes later [62]. Splenic tissues will phagocytose the heat-damaged RBCs, enabling radioisotope uptake of Tc-99m labelled RBCs. This is a specific and relatively sensitive method of diagnosis of splenosis as compared to the use of sulfur colloid, as the spleen takes up more than 90% of heat-damaged RBC as compared to 10% of sulfur colloid [42, 63]. However, improper preparation of heat-damaged RBCs such as overheating or underheating may result in false negatives [64]. In addition, scintigraphy has poor anatomic localization, which warrants the need to correlate the lesions with higher definition scans such as magnetic resonance imaging (MRI). Our study shows that Tc-99m labelled heat-damaged RBC is not widely used to diagnose IHS. This could be due to its limited availability or cost. Another clue suggestive for IHS is the absence or decreased number of Howell-Jolly bodies seen in peripheral blood smears, which would be normally seen in patients with asplenia [65].
In addition, though radiological findings for splenosis may mimic other hepatic lesions, Tsitouridis et al. described the characteristic imaging of IHS on CT and MRI imaging: hypodense lesion on non-contrast CT. Following contrast administration, the lesion is hyperdense in the arterial phase, isodense in the portal venous phase and hypodense in the delayed phase [31]. MRI findings include homogeneous hypointensity and hyperintensity prior to contrast administration on T1-weighted and T2-weighted images respectively, with a characteristic hypointense rim surrounding the lesion on T1-weighted imaging [31]. In addition, demonstration of classic heterogenous or arciform enhancement in the arterial phase with homogeneous enhancement in the delayed phase is classic for splenic enhancement and may suggest HIS [56]. Based on available data, the diagnosis of IHS can be made based on the ‘triad’ of 1) history of splenectomy or abdominal trauma, 2) absence of risk factors for liver malignancy and 3) typical imaging pattern on contrast enhanced imaging. Considering this ‘triad’ as a diagnostic hallmark of IHS, sensitivity of this triad in all the 59 reported cases was: 96.6% (n = 57/59) for one or more features, 52.5% (n = 31/59) for two or more features and 5.1% (n = 3/59) for all three features. Undoubtedly, the presence of all three cardinal features is rare, but is likely able to confirm the diagnosis of IHS without the need for surgical resection. We were unable to analyse the specificity of this triad as all the cases reported are diagnosed to be IHS.
Other imaging modalities such as the use of contrast-enhanced ultrasound can exclude HCC. On contrast-enhanced ultrasound, HCC appears as homogeneous and hyperechoic compared with the surrounding liver tissue after contrast administration, with a rapid washout and becoming a hypoechoic lesion in the portal and sinusoidal phases [19]. Superparamagnetic iron oxide (SPIO) administration in MRI scans can aid in tissue characterization. SPIO is taken up by the reticuloendothelial cells of the liver and spleen and has been shown to improve the detection rate of benign hepatocellular tumours [66]. IHS will demonstrate hypointensity on T2-weighted MRI due to phagocytosis of iron particles by splenic reticuloendothelial cells. Abdominal imaging does have its limitations and may not provide a definite diagnosis. Absolute diagnosis as with any malignant lesion is possible by sampling the tissue. Percutaneous image-guided needle biopsy can establish a definite diagnosis by demonstrating normal splenic tissue with red pulp and white pulp, lymphocyte B cells and CD3-positive lymphocyte T cells [27]. The use of fine needle aspiration cytology has been previously reported to avoid unnecessary surgery [67]. However, results may be inconclusive, and patients may have to bear additional costs of further diagnostic tests.
Surgical resection should be reserved for patients with inconclusive imaging scans or biopsy findings, abdominal symptoms not attributed to any other pathology, those in whom malignancy cannot be ruled out with certainty, or those with presence of risk factors for HCC. Explorative laparoscopy with intraoperative frozen section could be considered to reduce morbidity following liver resection [7, 26]. Should patients be diagnosed with IHS using non-invasive or minimally invasive methods, surgery can be avoided if patients are asymptomatic [57]. It has been reported that the average interval from trauma and abdominal splenosis is 10 years (range from 5 months to 32 years) [68, 69]. This is in contrast to our review, which demonstrated a median time of 21 years (range 1.5-47 years) from splenectomy to diagnosis of splenosis. Nevertheless, splenosis should still be considered in patients with a history of splenectomy regardless of the time from splenectomy. There have been two reported cases of IHS without any history of abdominal trauma or splenectomy: a 68-year-old woman presenting with recurrent abdominal pain [30]; and an asymptomatic 58-year-old man presenting with work-up for transaminitis [38]. There is no explanation for this phenomenon, but these occurrences are rare and IHS should only be a diagnosis of exclusion in the absence of prior history of abdominal trauma or splenectomy.
In conclusion, this review summarizes the available body of evidence for IHS. We also report a diagnostic triad: 1) history of splenectomy or abdominal trauma, 2) absence of risk factors for liver malignancy and 3) typical imaging features on contrast-enhanced imaging. In the presence of risk factors for HCC, malignancy should be ruled out. Non-invasive diagnostic tests such as Tc-99m heat-damaged RBC scintigraphy are useful in diagnosis. Surgery is reserved for patients with (1) abdominal pain or other symptoms which cannot be attributed to pathology or (2) inability to rule out malignancy. Clinicians should be aware of this rare pathology and all cases should be reported to enhance the knowledge and understanding of this disease.