Purpose
In aging societies, the incidence of several most common cancer entities, such as breast (BC), colorectal (CRC), and hepato-cellular carcinoma (HCC), is rising [1, 2]. The same applies to renal cell carcinoma (RCC), occurring more frequently in developed countries with increasing incidence rates, especially in elderly patients [3]. Due to frequent comorbidities in older patients, tumor resection might not be feasible to treat primary or secondary tumor lesions. Other reasons for ineligibility might include tumor stage, risk factors for general anesthetic, or patient’s refusal to undergo surgery.
Minimal invasive local treatment modalities, such as radio-frequency ablation (RFA), cryoablation (CA), or microwave ablation (MWA), can be alternative treatment options in patients with unresectable primary or secondary liver cancer [4, 5], renal cancer [6], and patients with lymphatic or adrenal metastases. In a palliative treatment setting, local ablative therapy can be applied for cyto-reduction; thus, lowering disease burden and prolonging survival [7]. In small renal cell carcinoma (cT1a) with a size below 4 cm, thermal ablation should be considered first-line therapy to reduce morbidity [6].
Another feasible treatment option can be computed tomography-guided interstitial high-dose-rate brachy-therapy (HDR-BT). It is an ablation technique using single-fraction irradiation with iridium-192 (Ir192) source placed in a target volume via percutaneously inserted catheters [8, 9]. This technique comes with a series of advantages. There are no limitations regarding tumor size or adjacency to larger vessels, which can cause a cooling effect in thermal ablation therapy. Moreover, there are no therapy restrictions regarding heat-vulnerable structures [10, 11].
Compared with stereotactic body radiation therapy (SBRT), which has advantages due to its’ non-invasive approach, fractionating and dose distribution, and therefore a possible decrease in radiation damage [12], HDR-BT eliminates respiratory motion by skin fixation of the catheter, which might spare healthy renal tissue and other adjacent organs.
It is mainly applied in colorectal metastases and hepato-cellular carcinoma [13, 14], but has also been used to ablate adrenal gland masses [13]. Furthermore, Damm et al. concluded HDR-BT to be a feasible treatment modality for the ablation of renal masses, also evaluating patients with previous complete or partial nephrectomy [8].
In this prospective study, we aimed to analyze functional parameters of the kidney and potential morphologic changes of the renal parenchyma after treatment with HDR-BT in patients with renal cell carcinoma, or post-treatment of adjacent metastases of the adrenal gland, lymph nodes, or liver.
Material and methods
Patients’ selection
This prospective study was approved by the institutional review board, and all patients provided oral and written informed consents. Patients were selected for HDR-BT due to inadequate clinical performance to undergo surgery safely, imminent hemodialysis after surgery due to past contralateral nephrectomy, or metastatic disease in a palliative treatment setting.
The inclusion criteria were: (1) Renal or adjacent renal masses with an indication for local ablative treatment; (2) Ineligibility to undergo surgical treatment; (3) Good physical performance status according to ECOG, to safely tolerate interventional treatment under conscious sedation; and (4) Written informed consent.
Patients with a life expectancy of less than 6 months were excluded. Furthermore, treatment was not feasible if the estimated dose exposure to organs at risk (OARs) was above clinical standards, or if there were insufficient laboratory parameters to undergo the procedure safely, including hemoglobin level < 6.0 mmol/l, thrombocyte count < 50 gpt/l, international normalized ratio > 1.5, and partial thromboplastin time > 50 sec. Patients who had undergone previous HDR-BT or SBRT were not excluded.
Radio-ablation by HDR brachytherapy
Before treatment, patients received antiemetic prophylaxis consisting of 8 mg dexamethasone and 8 mg ondansetron administered intravenously. After initial sedation with 1 mg midazolam and 50 to 100 μg fentanyl intravenously, the tumor mass was punctured percutaneously by an 18 G coaxial needle under computed tomography (CT) fluoroscopy (Aquillion, Canon Medical Systems, Neuss, Germany). A guidewire (Amplatz SuperStiff™, Boston Scientific, Marlborough, USA) was placed via the needle in the mass. Subsequently, a 6 F angiographic catheter sheath (Terumo Radifocus® Introducer II, Terumo Europe, Leuven, Belgium) was inserted, followed by a 6 F irradiation catheter (afterloading catheter, Primed® medical GmbH, Halberstadt, Germany). This afore-mentioned process was repeated in larger or complex-shaped lesions for enhanced coverage of the ablation zone, while reducing exposure to organs at risk. Depending on the pain level, we increased the administration of midazolam and fentanyl during the procedure in steps of either 50 μg fentanyl or 0.5 mg midazolam, or both. After placing the catheters, we performed a multi-slice contrast-enhanced CT exam to visualize the catheter position in the renal, adrenal, lymph nodal, or hepatic masses. Imaging data (axial slices with 3 mm thickness) were transferred to irradiation planning system (Oncentra® Brachy, Elekta Instrument AB, Stockholm, Sweden). In a 3D treatment plan, gross tumor volume (GTV) was delineated by hand. An automated algorithm generated a 5 mm safety margin to define clinical target volume (CTV), which was not edited to anatomic boundaries, and was directly adopted as planning target volume (PTV).
Depending on the tumor entity, a single dose of 15 Gy or 20 Gy was administered to PTV. In the ablation of renal cell carcinoma, HCC, and metastases of breast cancer, 15 Gy was applied. In patients with cholangiocarcinoma (CC), biliary duct, and CRC, the dose was increased to 20 Gy. In treating RCC tumor recurrences after partial resection or radio-frequency ablation, the dose was escalated to 20 Gy [14, 15]. In patients with recurrences after HDR-BT, the dose was escalated by 5 Gy, depending on the dose applied during first procedure.
Following the ablation procedure, we removed the catheters and sheaths, and placed rolls of gelatin sponge in the catheter path to prevent any complications from excessive bleeding. Any complications during the procedure were recorded and assessed by Clavien-Dindo classification [16]. Radiation-induced adverse events were classified by common terminology criteria for adverse events (CTCAE) version 4.02.
Imaging
Before treatment, we obtained images via magnetic resonance imaging (MRI) or contrast-enhanced CT. Patients with hepatic lesions received an MRI with a contrast agent (gadoxetate) unless there were contraindications. CT images of the thorax and abdomen were also obtained to detect possible metastases. In the follow-up period, all patients received MRI of the liver or abdomen every three months, and additional CT every three months if the patient had further known metastases or a high probability of metastatic spread. Two readers with over 10 years and 4 years of experience in abdominal imaging, performed the analysis of medical imaging regarding morphologic changes of the renal parenchyma. They matched the irradiation plan to the kidney. In the irradiation plan, 5, 6, 9, 12, 15, 22.5, 30.0, 37.5, and 45 Gy were illustrated. Any diminished perfusion in contrast-enhanced studies and/or edema within the renal parenchyma was matched to isodoses in the irradiation plan qualitatively.
Renal function tests
All patients received dynamic renal scintigraphy with technetium-99 mercaptoacetyltriglycine (Tc99m-MAG3) to determine the tubular extraction rate (TER) before and 3, 6, and 12 months after treatment with HDR-BT. TER for both kidneys was quantified separately to assess the effects of radiation exposure in the ipsilateral and contralateral kidneys. Blood samples were taken to determine creatinine level and estimate glomerular filtration rate (eGFR via chronic kidney disease epidemiology collabo-ration; CKD-EPI formula) before HDR-BT and 3 days, 3 months, 6 months, and 12 months post-treatment. The CKD-EPI formula is the recommended method for GFR estimation in adults, and includes serum creatinine, age, sex, and race [17].
Statistical analysis
IBM SPSS Statistics version 26.0® (IBM Corp., Armonk, NY, USA) and Excel (Microsoft®, Office version 16) were applied for statistical analysis. For patients’ characteristics, descriptive statistics were used. Renal function tests and V5 volumes (volume receiving 5 Gy) were evaluated with Wilcoxon’s signed-rank test. We used V5 volumes as a reference for radiation exposure to the kidney [18] as there are no known dose constraints for renal parenchyma in interstitial brachytherapy. Therefore, we used V5 to ensure comparability between the effects on the renal parenchyma in patients with renal and extra-renal lesions. Parameters were evaluated separately for patients treated for renal and extra-renal lesions as well as collectively. We evaluated changes over time within one group and drew comparisons between both groups. Tests were carried out two-sided. A p-value ≤ 0.05 was considered statistically significant.
Results
Patients’ characteristics
We included 35 patients in the study (21 males, 14 females; Table 1). All the patients were treated with HDR-BT in the time frame from November, 2011 to January, 2018. The follow-up for the renal function was 12 months. The average follow-up period for morphologic changes was 36.3 ±27.6 months. Most patients were treated for RCC (n = 27). A quarter of these patients (25.9%) had already undergone complete resection of the contralateral kidney or partial resection of the ipsilateral kidney (Table 2). Eight patients received treatment of extra-renal masses, with treatment sites in the liver, adrenal gland, and lymph nodes close to the right kidney (liver, n = 5; lymph node, n = 1; adrenal gland, n = 1) or left kidney (lymph node, n = 1). Apart from RCC, other tumor entities included cholangiocellular carcinoma (CC, n = 2), CRC (n = 2), BC (n = 2), HCC (n = 1), and adrenal gland carcinoma (ACC, n = 1). The patients did not receive any form of chemo- or immunotherapy concomitantly. Three patients with RCC started therapy with tyrosine kinase inhibitors, and two patients with extra-renal lesions received systemic treatment within one year after HDR-BT. One patient suffered a recurrence, and was treated with a second HDR-BT after nine months.
Table 1
Characteristics of 35 patients treated for 27 renal, 2 lymph nodal, 1 adrenal gland, and 5 hepatic masses
Table 2
Treatment specifics of renal cell carcinoma (n = 27)
Treatment characteristics
We applied a mean number of 2 catheters (range, 1-5) for sufficient dose application per treated lesion. The average CTV was 28.0 ±36.4 cm3. For patients with renal lesions, the mean CTV was 26.6 ±35.6 cm3, and for patients with lesions adjacent to the kidney, the mean CTV was 33.4 ±41.8 cm3. With radiation application, a mean effective tumor-surrounding dose (D100 = minimum dose covering 100% of CTV) of 16.47 ±2.82 Gy was achieved for renal lesions. We reached a D100 of 18.03 ±2.4 Gy within extra-renal lesions, including a 5 mm safety margin. The mean irradiation time for all the treated lesions was 1,176 ±788 s (19.6 ±13.1 min). In patients treated for RCC, V5 was 77.8 ±42.2 ml, with a mean renal volume of 177.2 ±101.7 ml. The fractional volume percentage receiving 5 Gy (V5%) was 48.7 ±24.0%. We determined a V5 renal volume of 44.0 ±33.0 ml (range, 17.9-99.2 ml; V5% of 32.0 ±25.3%), with a mean renal volume of 165.6 ±74.2 ml after treatment of extra-renal lesions. As suspected, renal volume receiving 5 Gy during the treatment of extra-renal masses was significantly lower than in renal masses (p = 0.024). Summarizing all patients independent of the treated lesion, the mean V5 was 70.0 ±42.4 ml, with a relative volume of the kidney parenchyma exposed at 44.9 ±24.9%.
Renal function analysis
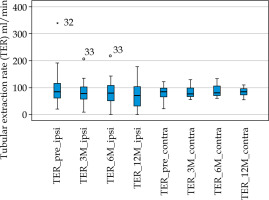
Before brachytherapy and 3 months, 6 months, and 12 months after HDR-BT, renal scintigraphy was performed, and TER was determined. The median TER decreased from 152.0 ml/min (range, 42.6-340.0 ml/min) at baseline to 139.5 ml/min (range, 60.0-225.0 ml/min) after 3 months, and remained stable with 143.0 ml/min (range 0.0-234.0 ml/min) after 6 months and decreased further to 129.3 ml/min (range, 0.0-186.0 ml/min) after 12 months follow-up. However, only a third of all study patients (n = 12) received final renal scintigraphy after 12 months.
Similarly, TER of the treated kidney side or possibly compromised side due its’ proximity to the radiation zone slightly decreased from a baseline median TER of 83.6 ml/min (range, 20.9-340.0 ml/min) to 79.0 ml/min (range, 9.5-207.0 ml/min) after 3 months, 76.9 ml/min (range, 0.0-218.0 ml/min) after 6 months, and 71.1 ml/min (range, 0.0-177.6 ml/min) after 12 months. There was a significant difference between TER at baseline and 12 months after brachytherapy (p = 0.021). The contralateral side seemed to be unaffected, with 85.1 ml/min (range 21.7-122.9 ml/min) at baseline, 80.8 ml/min (range, 55.9-129.6 ml/min) after 3 months, and 85.3 ml/min (range, 55.0-110.2 ml/min) after 12 months follow-up (TER baseline – TER 12 months, p = 0.844).
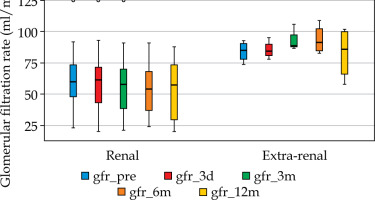
After treatment of extra-renal lesions, there was no significant TER reduction or increase in ipsilateral (TER baseline – TER 12 months, p = 0.174) or contralateral (TER baseline – TER 12 months, p = 0.053) sides after 12 months. The glomerular filtration rate was estimated using the CKD-EPI formula after laboratory assessment of serum creatinine at baseline and 3 days after HDR-BT, with consecutive evaluations after 3, 6, and 12 months of follow-up. Before treatment, the median GFR was significantly higher in the extra-renal treatment group, with a median of 89.0 ml/min (range, 74.0-101.0 ml/min) compared with the renal treatment group, with 65 ml/min (range, 23.0-125.0 ml/min) (p = 0.04).
In all patients, we found a slight, yet not significant median decrease of GFR from 71.0 ml/min (range, 23.0-125 ml/min) at baseline to 68.0 ml/min (range, 24.0-109.0 ml/min) after six months (p = 0.126). However, there was a further significant reduction to 59.5 ml/min (range, 20.0-102.0 ml/min) after 12 months of follow-up (p = 0.005).
At baseline, the median KDOQI CKD (chronic kidney disease) stage was 2 (GFR, 60-89 ml/min) in all patients. Nine patients (25.7%) were classified with KDQOI stage 3. Three patients (8.5%) had severely deteriorated renal function, and were ranked in stage 4 before treatment. Before treatment, patients with extra-renal masses were classified as stage 1 or 2 (range, 74.0 to 101.0 ml/min).
After 12 months, there was a slight increase to a median CKD stage of 3 (GFR, 30-59 ml/min) in patients with renal ablation, whereas in patients with extra-renal treatment, the GFR statistically improved to stage 1 (GFR > 89 ml/min). Overall, there was no significant increase of the KDOQI CKD stage in all patients (p = 0.109), patients treated for renal lesions (p = 0.070), or extra-renal lesions (p = 1.0) after 12 months of follow-up (Figure 3).
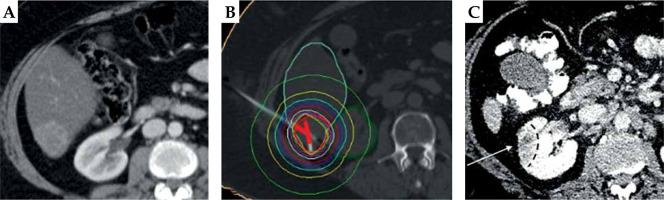
Fig. 1
Image data set showing computed tomography-guided brachytherapy for colorectal metastasis of the liver (S VI) close to the right kidney. A) Computed tomography fluoroscopy with image-guided insertion of a coaxial needle; B) Diagnostic computed tomography with the depiction of 2 catheter placements with the hepatic lesion; C) Irradiation plan showing the tip of iridium-192 source (red line) and corresponding isodoses for radio-ablation

Morphologic changes of renal parenchyma after HDR-BT
Matching the isodoses of the radiation plan with follow-up images, we detected morphologic changes in the kidneys of 3 patients treated for extra-renal metastases. Two patients showed distinctive matching renal lesions in contrast-enhanced CT or MRI approximately 13 and 22 months after treatment of the liver with HDR-BT. One patient developed an aneurysm of the renal artery about 10 months after therapy of a lymph node adjacent to the left kidney. Of these three patients, only one treated for liver metastasis experienced an increase in the KDOQI CKD stage from 2 to 3 after 12 months. The other patients were unaffected. Isodoses in the affected areas ranged from 10.0 to 18.7 Gy. Figure 4 depicts these morphologic changes after HDR-BT of liver metastasis in liver segment VI. Apart from expected changes to the treated lesions in patients with renal cell carcinoma, only one patient showed further morphologic changes in the kidney at six months after treatment.
Fig. 4
Illustration of irradiation-induced damage of the right kidney after close irradiation in liver segment VI. A) Diagnostic computed tomography before brachytherapy; B) Irradiation plan showing isodoses for radio-ablation with the depiction of isodoses reaching the kidney parenchyma; C) Diagnostic computed tomography approximately one year after HDR-BT showing irradiation-induced damage
Discussion
In this prospective study, we investigated changes in renal function and morphology via renal scintigraphy, glomerular filtration rate, and CT and MRI imaging after treatment of renal and extra-renal primary tumors or metastatic lesions in various tumor entities. To our knowledge, this study is one of only a few studies on renal function after ablation that systematically analyzed tubular extraction rate via renal scintigraphy [8, 19].
We especially put emphasis on the evaluation of renal function loss after HDR-BT of metastases of the liver, lymph nodes, or adrenal gland adjacent to the right or left kidney. Various function loss can be expected in patients treated with HDR-BT for renal cell carcinoma [8]. However, the safety of adjacent organs, including the kidney, when treating extra-renal masses is critical.
Evaluation of renal function after HDR-BT
There were no acute radiation-induced effects on the renal function or adjacent organs to the treatment location immediately after treatment with HDR-BT. The majority of our study cohort was treated for renal masses. Hence, evaluating all patients, we expected to find a decrease in renal function on the ipsilateral renal side [8], showing a significant reduction of the tubular extraction rate in renal scintigraphy on the ipsilateral side after 12 months of follow-up. As expected, there was no significant reduction of TER on the untreated contralateral side for the duration of the follow-up period. We found a significantly decreased filtration rate in all patients after 12 months of follow-up. However, there was no significant deterioration of the renal function according to the KDOQI stage. We found no significant GFR or KDOQI CKD change in patients treated for extra-renal lesions after 12 months. Only one patient treated for liver metastasis experienced a relevant decrease in renal function from the KDOQI stage 2 to 3 after 12 months. The other patients were unaffected.
Similarly, there was no significant increase of the KDOQI CKD stage after 12 months in all other patients treated for renal masses. This is an important finding since the progress of CKD stage correlates with increasing occurrences of hypoalbuminemia, hypertension, hyperparathyroidism, and anemia, and thus elevating the cardiovascular risk [20]. Over one-third of all the patients, and almost half of those with renal lesions were classified with KDOQI stage 3 or 4 before therapy. Additionally, approximately a quarter of all RCC patients had been treated with partial or complete nephrectomy before treatment. A study on the risks of significant GFR decline after nephrectomy identified elevated levels of pre-operative creatinine, increasing age, and female gender as the significant risk factors for functional deterioration. In cases with an increased risk, the authors favored approaches with nephron preservation [21]. Like thermal ablation techniques [23], HDR-BT generally seems to preserve nephron function with no significant decline in the CKD stage in treating extra-renal and renal lesions.
Evaluation of morphologic changes after HDR-BT
We detected no acute morphologic changes after HDR-BT in CT or MRI follow-up images. However, morphologic changes in the ipsilateral kidney in four patients after a follow-up period of 6 to 22 months were identified, 3 of whom were treated for extra-renal masses. Only one of these patients experienced a relevant function decrease from KDOQI stage 2 to 3 after 12 months. Radiation-induced long-term changes manifest in interstitial fibrosis and loss of nephron mass [22]. It is suspected that triggering inflammation through ionizing radiation and cytokines released upon apoptosis after high doses of radiation, may lead to renal fibrosis [23].
Surprisingly, more distinctive changes were detected (which matched isodoses) in patients treated for extra-renal lesions than for renal lesions.
As the catheters in treatment of extra-renal lesions were not fixated on the kidney, this could be due to breathing motion leading to dose variations, which cannot be reproduced. However, as there are no known dose constraints for renal parenchyma in interstitial brachytherapy, it remains largely unclear.
In partial body irradiation, keeping the mean dose for both kidneys below 18.0 Gy is recommended to prevent tissue damage [22]. As the isodose for the affected area in patient experiencing relevant function decrease only reached 10.0 Gy, we suspect a high V5 volume percentage of over 60%, contributing to the function decrease. However, secondary underlying causes cannot be ruled out.
Overall, a distinct area of morphologically altered kidney parenchyma associated with a specific isodose, as regularly encountered in HDR-BT of the liver [24], seems to be a rare event.
Limitations
This was a prospective study comprising a small study group with advanced age and predominately pre-existing reduction of renal function. As we treated renal and extra-renal treatment locations, our study cohort was very heterogenic due to different tumor entities and pre-existing medical conditions, which might influence the occurrence of adverse advents. However, we focused on the effects of radiation on the kidney, which should be independent of the tumor entity. Furthermore, a relevant portion of the patients was lost to follow-up regarding renal scintigraphy after 12 months due to availability and scheduling conflicts, which hampered the evaluation of TER. However, we analyzed TER in 22 patients after 3 months, and the creatinine level in almost all patients for the entire follow-up period and coverage of imaging were sufficient.
Conclusions
Computed tomography-guided HDR-BT is a viable treatment modality for local ablative treatment of renal and renal adjacent masses in patients with pre-existing renal insufficiency, ineligibility for surgery, and patients with a high-risk of function loss due to partial or complete contralateral nephrectomy, or in a palliative treatment setting.
Despite a significant decrease in renal function parameters after 12 months, no significant increase of the KDOQI CKD stage as a predictor for complications arising from chronic kidney disease was observed.
Within our studied period of 12 months, HDR-BT is a safe procedure in treating extra-renal lesions close to the kidney, as there was no significant change in TER, GFR, or KDOQI stage in the subanalysis.
Contrary to tissue damage frequently seen in liver parenchyma after HDR-BT, only rare cases of focal edema or diminished perfusion in follow-up imaging were noted.
For investigation of survival and tumor control, we are currently analyzing data from a larger study cohort that might also give more insights into the vulnerability of renal parenchyma.