Introduction
Aneurysms of sinuses of Valsalva are rare aortic anomalies having an incidence of 1.4–4.94% in the Asian population. They account for 0.1% to 3.5% of all congenital heart defects and around 0.14% to 3.5% of all open heart procedures [1–3]. These aneurysms are congenital or acquired. The congenital aneurysms are thought to result from congenital absence of elastic and muscular tissue in the wall of the sinus of Valsalva (SOV) [4]. Acquired aneurysms of the sinuses of Valsalva may be secondary to syphilis or infective endocarditis. Males are affected more than females and the reported incidence is higher in people of Asian origin as compared to others [5]. SOV aneurysms are mostly associated with ventricular septal defect (VSD) or aortic regurgitation (AR). Spontaneous rupture is the most common complication. When complicated by rupture, patients usually present with congestive cardiac failure. Ruptured sinus of Valsalva aneurysms (RSOVA), if untreated, have a median survival of 2 years. Once ruptured, surgery is the mainstay of treatment. Surgery for RSOVA is associated with a good success rate and low mortality and morbidity. Hence, it is very important to diagnose early and proceed with surgical repair in patients with RSOVA.
Material and methods
We identified 21 patients in a retrospective review during the period of January 2013 to January 2020 with ruptured sinus of Valsalva aneurysms. All these patients were operated on at a tertiary care centre. The departmental review board approved the study and waived the requirement of individual consent. We chose to exclude patients with a suspicion of infective endocarditis or those with non-ruptured sinus of Valsalva aneurysm. Surgery was performed on semi-emergency basis for these patients once diagnosed. The surgical repair was done on cardiopulmonary bypass (CPB) using moderate hypothermia in an arrested heart using standard aortobicaval cannulation. Median sternotomy was the approach. Myocardial protection was achieved via antegrade del Nido cardioplegia. The follow-up duration of these patients was between 1 year and 7 years. We analysed these patients with respect to gender, age at presentation, site of aneurysm, surgical repair and post-operative course.
Pre-operative evaluation
Diagnosis in these patients was made with the help of trans-thoracic echocardiography. Many of these patients were evaluated with trans-oesophageal echocardiography as well to see for feasibility of percutaneous closure. Echocardiographic examination was conclusive in all patients and no patient underwent any other investigation such as computed tomography (CT) scan or cardiac magnetic resonance imaging (MRI).
Surgery
All patients underwent surgical repair under cardiopulmonary bypass with moderate hypothermia through a median sternotomy. Aortobicaval cannulation was used and the procedure was done on an arrested heart with cold del Nido cardioplegia. An oblique aortotomy was used and cardioplegia was administered directly into the coronary ostia. The right atrium (RA) incision was made parallel to the atrioventricular (AV) groove and the left atrium (LA) was vented through the inter-atrial septum. Through the RA, the windsock formed due to the RSOVA was excised. In cases where it was not excised, on the right atrial/right ventricular side, closure was done with a Dacron patch (Sauvage Filamentous Dacron – BARD) or by direct closure. On the aortic side, a Dacron patch closure was done for all patients. Correction of associated anomalies such as VSD was done during the period of cardiac arrest.
Post-operative evaluation
During the post-operative course in the ward, patients underwent a 2D echo once to look for any residual anomalies or any patch leak. Patients were started on Aspirin 75 mg post-operatively and those who underwent valve replacement were started on warfarin. Once discharged, patients were followed up on an outpatient basis and underwent yearly echocardiograms.
Results
During the 7-year period that we analysed, we found 21 patients who were referred to our department with RSOVA. Out of the 21 patients, 17 were male and 4 were female. The mean age of these patients at referral was 27.8 ±7.79 years (range: 15–45 years). The most common symptoms at presentation were dyspnoea on exertion in 18 (86%) patients and palpitations in 15 (71%) patients (Table I). On admission, all patients were symptomatic and the mean duration of symptoms was 5 months. Out of 21 patients, 13 and 5 patients were in New York Heart Association (NYHA) functional class III and IV respectively. The diagnosis was made on trans-thoracic echocardiography in all patients. Two patients underwent workup for device closure of the RSOVA, but due to technical difficulties during the procedure, they were referred for surgery.
Table I
Symptom profile of patients
| Symptom | Value |
|---|---|
| Dyspnoea on exertion | 18/21 (86%) |
| Palpitations | 15/21 (71%) |
| Chest pain | 5/21 (23%) |
| Fatigue | 11/21 (52%) |
The mean CPB time was 136 ±50 min (range: 85–307 min) and the mean aortic cross clamp time was 98 ±37 min (range: 57–222 min). In 16 patients, the site of origin was the right coronary sinus (RCS) and in 5 patients, it was the non-coronary sinus (NCS). The site of rupture was the right ventricular outflow tract (RVOT) in 14 patients and the RA in 7 patients. The origins of the RSOVA and their chamber of rupture are given in Table II.
Table II
Anatomical distribution of RSOVA
| Site of origin of RSOVA | Site of rupture | Number |
|---|---|---|
| RCS | RVOT | 14 |
| RA | 2 | |
| NCS | RA | 5 |
Eleven out of 21 patients had a VSD in addition to the RSOVA and underwent patch closure. Four out of 21 patients had a bicuspid aortic valve. One patient had a sub-aortic spur causing sub-aortic obstruction which was excised intra-operatively. This same patient also had 2 separate openings of the left anterior descending artery (LAD) and left circumflex artery (LCx). Eighteen patients had less than mild aortic regurgitation (AR) at surgery and 2 patients had moderate AR. One patient had severe AR when taken for surgery and underwent aortic valve replacement (AVR).
The post-operative period generally was uneventful for the majority of patients. The mean ICU stay was 2.3 ±0.8 days and the mean post-operative duration of stay was 8.1 ±3.3 days. Post-operative complications included re-exploration due to bleeding in 1 patient and wound infection in 3 patients.
There was no immediate or 30-day mortality in our series. Out of 21, 15 patients were followed up regularly until the end of the study period. One patient had patch dehiscence and presented at 1 year after the original surgery. This patient underwent redo surgery with RSOVA repair; however, this patient succumbed in the post-operative period due to intractable ventricular arrhythmias. Two patients during follow-up came with severe AR and underwent redo AVR. One patient had a successful term pregnancy during her follow-up and another patient is under close follow-up for moderate AR.
The pre-operative and operative data are summarised in Table III.
Table III
Pre-operative and operative parameters
Discussion
Aneurysms of the sinus of Valsalva are rare cardiac anomalies and have an incidence in the Asian population which is 5 times that of the western population [6, 7]. The description of the morphology of RSOVA was given by Edward et al. in 1957 where he showed that the aetiology is separation of the aortic media of the sinus from the media adjacent to the hinge line of the aortic valve cusp [8]. In 1962, Sakakibara and Konno classified congenital aneurysms of the sinuses of Valsalva into 4 types [9]. A modification was proposed by Xin-jin et al. to classify them into 5 types [10].
We had a very high percentage of male patients (81%) as compared to females (19%). The mean age of our patients was 27.8 years with a range of 15 to 45 years. This is very similar to other reports in the literature which showed a higher frequency of RSOVA in young males. Most of our patients were in NYHA functional class III or IV and had a mean duration of symptoms of around 5 months. Such late presentation is very common in the Indian set up and occurs due to logistical difficulties as well as poor education and literacy levels.
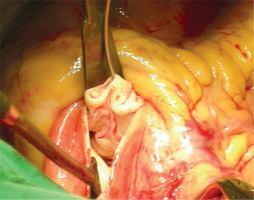
In our study, the right coronary sinus was the most involved followed by involvement of the non-coronary sinus (NCS) (Figures 1, 2). We did not see any case of left coronary sinus (LCS) involvement. LCS involvement is very rarely described even in the literature. The types of RSOVA that we encountered are very similar to the published literature [11–15].
Figure 2
Right coronary sinus – right ventricular outflow tract RSOVA everted and seen through the aortic incision
RSOVA are generally associated with other cardiac anomalies, namely VSD, bicuspid aortic valves, AR, aortic coarctation and tricuspid insufficiency. VSD is most commonly found in these patients and we encountered a very high percentage (52%) of VSDs. Many previous studies have quoted a higher percentage of VSD as compared to AR in these patients [11–18]. Considerable AR was present in only 3 of our patients pre-operatively. Aortic regurgitation in RSOVA results from malcoaptation of the aortic valve cusp due to unbalanced diastolic closing pressure of the opposing cusps. Also, the Venturi effect at the prolapsing cusp can lead to distorted closure of the cusps [19]. In patients who have an associated VSD, prolapsed aortic cusps with a lack of supporting tissue can cause AR [20]. Over a period of time, valve cusps get sclerosed, thus increasing the AR and substantiating the need for aortic valve replacement rather than repair. We performed AVR for the 1 patient in whom the AR was very severe. Most of these operations were performed when aortic valve repair experience was lacking at our centre. The rate of AVR is higher in Asian patients as compared to western patients [21]. Bicuspid aortic valve, which is another commonly encountered entity along with RSOVA, was present in 4 (19%) out of 11 patients.
The surgical times of our series are longer as compared to other published reports. However, we did not encounter any untoward complication that might arise because of longer CPB times. Our patients had an uneventful post-operative stay and were discharged successfully. The reversal of NYHA status was clearly seen in our patients within their hospital stay (Table IV). We did not observe any in-hospital or 30-day mortality, and many surgeons have observed similar low figures of mortality for surgery on RSOVA. The hospital stay of our patients was in correspondence to the mean hospital stay for any of our other cardiac surgical patients. These factors stressed that RSOVA repair on CPB in an arrested heart is a relatively safe procedure to perform.
Table IV
NYHA functional class of patients during the study
| NYHA class | Before surgery | At discharge | Follow-up at 1 year |
|---|---|---|---|
| I | 0 | 17 | 12 |
| II | 3 | 4 | 8 |
| III | 13 | 0 | 1 |
| IV | 5 | 0 | 0 |
Follow-up is very important in patients after operations for RSOVA as they tend to develop AR, which has been highlighted by numerous articles in the past. Pre-operative infective endocarditis, co-existent VSD, bicuspid aortic valve, surgical approach and method of closure have been shown to influence the development of late AR [17]. Jung et al. found aortotomy and the aortic approach to be a significant risk factor for late AR in spite of the fact that the aortic approach facilitates better exposure of the aortic valve and possibility of repair [22]. We encountered 2 patients who presented to us with severe AR during follow-up and both underwent AVR. Both these patients had RSOVA of the RCS-RVOT type with a VSD and moderate AR prior to the first surgery, which had decreased to mild AR on post-operative echo. Over a period of time, its severity increased and they had to undergo a second operation. Probably, progression of the disease could be a reason why they progressed to severe AR as their 2D echo was near normal in the post-operative period.
Patch dehiscence, as can happen with VSDs, did happen in our series in 1 patient, and this patient underwent redo surgery with re-patching. This patient expired during the redo surgery and this patient remains the only mortality in this series.
Various methods of closure of RSOVA are in practice today. Trans-catheter closure is also a safe and non-invasive technique for the treatment of this anomaly [23]. However, it has its own limitations and we had 2 patients who were referred to us due to technical difficulties in performing trans-catheter closure. Mo et al. described a case series of on-pump beating heart repair of RSOVA [24]. Buczkowski described a novel closure of RSOVA using the native aortic valve leaflet [25]. Similarly, minimally invasive trans-thoracic device closure of the aneurysm has been described by Gao et al. [26].
Although with the advent of time, percutaneous and minimally invasive approaches are taking their place in cardiac surgery, the safety of performing the same procedure in an arrested heart on cardiopulmonary bypass cannot be debated. We have obtained results which are comparable to existing literature using the conventional sternotomy approach using a cardiopulmonary bypass and cardioplegia. Hence our technique not only has general effectiveness but also is a very safe and secure technique to handle ruptured sinus of Valsalva aneurysms.
Conclusions
RSOVA has a higher percentage of involvement in young males. VSD, aortic regurgitation and bicuspid aortic valve are anomalies commonly associated with it. Patients generally present with dyspnoea on exertion and palpitations. RCS-RVOT involvement is the most common type. Surgery on CPB with aortobicaval cannulation with moderate hypothermia with del Nido cardioplegia is a safe approach to tackle RSOVA and gives good immediate and long term results. A good quality of life can be given to these patients after surgery and a good follow-up of these patients is important to detect aortic regurgitation.







