Purpose
Local ipsilateral breast tumor recurrences (IBTR) are relatively uncommon and highly heterogeneous. The risk of IBTR depends on numerous factors, including age, inherited susceptibility, tumor characteristics, type of primary cancer treatment, and lifestyle factors such as obesity and alcohol use. Recurrence rates are approximately 10% at 10 years and 20% at 15 years [1]. Several studies [2,3] have sought to identify prognostic factors for recurrent disease after radical treatment for invasive breast cancer. Those studies have found that outcomes are worse in patients who experience a recurrence within two years from the initial treatment compared to those with a longer recurrence-free interval. This difference may, at least partially, be explained by the hypothesis that early recurrences are caused by cell repopulation due to persistent microscopic disease, whereas late recurrences are more likely attributable to be due to a new primary tumor formation.
In recurrent disease, salvage radiotherapy is generally not an option, because most patients who develop locally recurrent disease have previously undergone breast irradiation. As a result, until lately, the standard salvage treatment in these cases was mastectomy. However, in recent years, several single-institution studies [4] have investigated the use of breast-conserving surgery (BCS) with or without adjuvant radiotherapy. A literature review conducted by Hannoun-Levi et al. showed that patients treated with a second breast-conserving treatment (BCT), that is tumorectomy plus radiotherapy, had only a 10% risk of developing another recurrence at the same site, a rate that is comparable to the recurrence rate observed in patients treated with salvage mastectomy. In both groups, overall survival (OS) was the same (75% at 10 years) [4]. In addition, a multicentric trial conducted by the GEC-ESTRO Breast Cancer Working Group found that patients who underwent salvage therapy involving lumpectomy plus re-irradiation by interstitial multicatheter brachytherapy, had a recurrence rate for a second IBTR of approximately 5% [5]. These data suggest that combining BCS with local irradiation may be an emerging standard of care in IBTR, especially when the aim is to preserve the breast. This combined approach is supported by data from several retrospective studies [6], but no randomized trials have yet been performed to determine non-inferiority. In this context, more data to support the safety and efficacy of this approach would be desirable.
The most common approach for re-irradiation in patients undergoing a second BCT is interstitial brachytherapy, either low-dose-rate (LDR) or high-dose-rate (HDR) [7,8,9,10,11,12]. However, external beam radiation therapy (EBRT) and intraoperative radiation therapy (IORT) (50 kV photons) have also been described [13,14].
The aim of the present retrospective study was to evaluate the outcomes and treatment-related toxicity in a series of patients who underwent intraoperative or post-operative multicatheter interstitial brachytherapy for locally recurrent breast cancer.
Material and methods
Between June 2002 and October 2017, 40 patients underwent BCT at our institution (the Catalan Institute of Oncology, Barcelona, Spain) to treat an IBTR. The treatment consisted of a second tumorectomy plus either intraoperative (n = 26) or post-operative (n = 14) multicatheter brachytherapy implant for accelerated partial breast irradiation (APBI). We retrospectively analyzed overall survival, toxicity, and cosmesis. The main characteristics of the primary tumor are summarized in Table 1. In all cases, the treatment included tumorectomy, with a resection margin that included sufficient normal breast tissue to ensure clear margins. Sentinel node biopsy (SNB) was performed in all cases, except for patients who had already undergone axillary lymph node dissection for a primary tumor.
Table 1
Primary tumor characteristics
Eligibility criteria for multicatheter brachytherapy were as follows: 1) Locally recurrent disease; 2) Breast anatomy suitable for multicatheter implantation; 3) Refusal to undergo mastectomy after previous treatment with BCS and adjuvant whole-breast irradiation (WBI); and 4) Unicentric, unifocal tumor with negative margins and negative SNB. Follow-up consisted of a complete clinical examination and was performed during post-operative stage at first or second month, then every 6 months for the first two years, and annually thereafter. All the patients underwent an annual mammography.
This study was conducted in accordance with our institutional protocols, and all of the cases were presented at a breast cancer tumor board. Written informed consent was obtained from every patient prior to treatment.
Implant technique and treatment delivery
All patients underwent tumorectomy. During the surgical procedure, six metallic clips were inserted around the tumor bed margins following the technique described by Major et al. [15]. Multicatheter implantation was performed intraoperatively in 26 patients and post-operatively in 14 patients. Intraoperative implantation is presented in Figure 1. After tumorectomy, tissue samples from the sentinel lymph node and tumor margins were sent for intraoperative pathological evaluation. After the pathological report confirmed a negative result, we proceeded to manually insert metallic needles into the open cavity following the technique described by our group previously [16]. Post-operative implantation is presented in Figure 2.
Fig. 1
Intraoperative implantation: A) Manual insertion of metallic needles into the open cavity; B) Needles inserted in the inferior plane and sutured skin
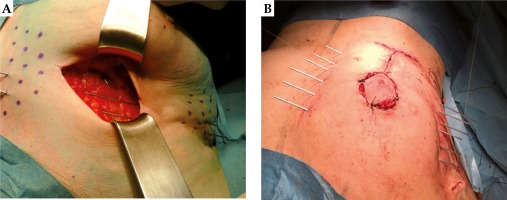
Fig. 2
Post-operative implantation: A) The needles were spaced to form equilateral triangles of 1.6 cm using a plastic template; B) Direct visualization of the seroma using ultrasound guidance
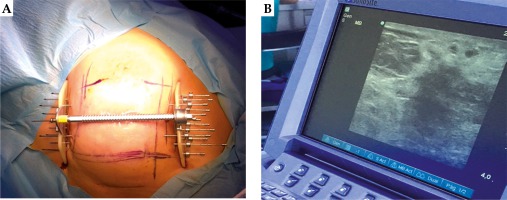
In the 14 patients who underwent post-operative brachytherapy, this procedure was performed from 15-45 days after tumorectomy under direct visualization of the seroma using ultrasound guidance. In all cases, a plastic guide template with needle holes was used to achieve geometric distribution. The needles were spaced to form equilateral triangles of 1.6 cm and inserted in two to four planes. After insertion, the needles were replaced with plastic tubes. The number of applicators and tubes varied on a case by case basis according to the size of the tumor cavity and individual breast anatomy. Next, a computed tomography (CT) scan with 2 mm slice thickness was performed. The Oncentra system (Elekta Company; Veenendaal, the Netherlands) was used to define the planning target volume (PTV), including a 2 cm margin of safety to the tumor edge [15]. In cases in which the PTV overlapped the skin and/or chest wall, a 5 mm margin was cropped out of these structures [17]. A modified Paris system was used for dosimetric purposes [18]. The treatment planning parameters were as follows: ≥ 90% of the defined PTV had to receive 100% of the prescribed dose (coverage ratio ≥ 0.9); maximum dose to the skin: ≤ 70% of the prescribed dose; D90 > 100%; V150 < 50%, with a dose non-uniformity ratio (DNR) < 0.35.
Until September 2012, we used the treatment scheme (3.4 Gy/10 fractions) described by Vicini et al. [19]. However, this treatment scheme was changed in October 2012, as our center participated in the GEC-ESTRO randomized trial [20]. Accordingly, the patients in this study received either 10 fractions of 3.4 Gy (n = 20) or 8 fractions of 4 Gy (n = 19). One elderly patient (age 92) received a single 16 Gy fraction due to her advanced age and poor performance status [21,22]. Notwithstanding these differences in fractionation schedules, the equivalent total dose in 2 Gy fractions (EQD2), with a tumor α/β ratio value of 4 was similar in both schemes (41.93 Gy and 42.67 Gy, respectively), as were the biologically-effective doses (BEDs): 62.9 Gy and 64 Gy, respectively. The EQD2 for a single fraction of 16 Gy is equal to 53 Gy [23,24].
Results
A total of 40 women diagnosed with IBTR underwent salvage HDR brachytherapy after BCS. Of these 40 patients, 26 (65%) underwent intraoperative interstitial multicatheter implant, while the other 14 patients (35%) received a post-operative implant. Median follow-up was 61.5 months (range, 12-153). Median age at recurrence was 65 years (range, 41-92). Most patients (25/40, 62.5%) were ≥ 60 years. The demographic and tumor characteristics are provided in Table 2. The median time to local recurrence (LR) was 10 years (range, 2-29). In one patient, the recurrence-free interval was 29 years; in that case, the recurrence was located at the edge of the primary surgical bed and was interpreted as a late relapse rather than as a new primary cancer in the same quadrant. Most patients (n = 26, 65%) had infiltrating ductal carcinoma (Table 2), and 70% had luminal A disease. A median of 14 tubes (range, 7-18) were inserted. In almost all cases (70%), 3 catheter planes were used. Nineteen patients (47.5%) were treated according to the revised GEC-ESTRO treatment schedule (32 Gy in 8 fractions), 20 patients (50%) were treated with the classic schedule (34 Gy in 10 fractions), and one patient received 16 Gy in a single faction. The mean V100 was 115 cc, with a median of 132.5 cc (range, 54.8-164 cc). Mean V150 was 38.5 cc (range, 16-65 cc). Treatment characteristics and parameters of the dosimetric analysis are provided in Table 3. At least 90% of the defined PTV received 100% of the prescribed dose (coverage index > 0.9). Underdosing of the PTV was accepted only to meet dose constraints for the skin and chest wall. Mean coverage index was 90.1% (median, 92.25%, min 78.61, max 99%).
Table 2
Patient demographics and characteristics of recurrent tumor
Table 3
Treatment characteristics and dosimetric analysis
Disease control
In our series, two patients developed a second relapse at 3 and 5 years after salvage treatment, respectively. One patient underwent salvage mastectomy and remains free of disease and alive 10 years after brachytherapy. The second one developed both local relapse and bone metastasis. She was treated with systemic therapy; the disease is stable at present. Overall survival at 3 and 5 years were 97% and 85.3%, respectively. Five-year CSS was 96%. The rate of local relapse (local relapse-free survival), evaluated with Kaplan-Meier analysis was 96.6% at 5 years and 91.7% at 7 years. Three patients developed distant metastasis: one at 1 month, second at 3 years, and third patient at 10 years. Five-year metastasis-free survival at 3 and 5 years was 94% (±8%). There were two cancer-related deaths, which was due to metastatic disease 4 and 10 years after salvage treatment. Bone and lymph node metastases were detected in one patient 30 days after salvage treatment, a finding that suggests the patient had been understated at the initial surgery. At the time of writing the paper, this patient remains alive, currently undergoing chemotherapy. A total of 3 patients (7.5%) died of causes unrelated to cancer. No evidence of relapse was observed in most cases (34/40 patients, 85%).
Toxicity and cosmetic outcomes
One patient developed a G2 hematoma. Acute infectious mastitis was observed in 7 patients (17.5%). Due to this relatively high infection rate, prophylactic antibiotics are now routinely administered at our institution for all intraoperative approaches. None of the patients who underwent post-operative catheter implantation developed an infection, even without the use of prophylactic antibiotics. Grade (G) 0-2 late fibrosis was observed in 65% of the patients, while 27.5% (n = 11) and 7.5% (n = 3) developed G3 and G4 late fibrosis, respectively. At the last follow-up visit, late toxicity in the series was as follows: mastitis (6 cases, 15%), hypochromic skin spots at the catheter entrance and exit points (8 patients, 20%), telangiectasia (7 patients, 17.5%), and fat necrosis (one case). Cosmetic outcomes determined according to on the 4-point Harvard breast cosmesis scale [25] were as follows: good (n = 23, 57.5%), fair (n = 6, 15%), and poor (n = 7, 17.5%); in 4 cases, no data were available (10%). Acute and late toxicity outcomes are shown in Table 4. Unfortunately, we do not have any data on cosmetic outcomes after primary treatment.
Discussion
The present retrospective study describes survival and treatment-related toxicity outcomes in a series of 40 patients who underwent tumorectomy followed by either intraoperative or post-operative multicatheter brachytherapy as a salvage treatment for IBTR. Our findings show that survival outcomes using this technique are good, with OS and CSS rates at 5 years of 85.3% and 96%, respectively. Importantly, only two patients in this series died of cancer-related causes, and only one developed local relapse and bone metastasis. In the last 30 years, several studies have been performed to validate the use of a second BCT in patients with IBTR. While mastectomy is still widely used for salvage treatment, there is a growing trend towards breast-conserving approaches consisting of tumorectomy plus re-irradiation (particularly APBI). The available data suggest that this approach is a valid alternative to mastectomy [26,27,28]. Although no non-inferiority phase III studies are currently available, there is a growing body of evidence indicating that re-treatment with breast conserving procedures is both safe and effective, with excellent local control, survival, cosmesis, and patient’s satisfaction [26,27,28].
One of the main concerns in patients with IBTR is the risk of developing metastatic disease. The degree of risk appears to be associated with tumor-related prognostic factors and with the time elapsed between diagnosis of the original breast cancer and disease recurrence, which is considered an independent prognostic factor. Previous hormonotherapy or chemotherapy are also associated with the risk of developing systemic disease [3,29]. Interestingly, the overall risk of developing distant metastases is approximately 30%, even in patients who undergo mastectomy or mastectomy plus re-irradiation. Overall survival rates range from 31% to 80% [2,30,31,32,33].
In our series, three patients developed a second relapse after salvage treatment. Published reports indicate that anywhere from 0% to 26% of patients will develop a second local recurrence after BCS with re-irradiation, with a 5-year disease-free survival (DFS) rate of approximately 60% (range, 31% to 85%). Voogd et al. [30] retrospectively evaluated 266 patients with IBRT treated by mastectomy alone and finding that 25% of patients developed a second local recurrence. In our series, the 5-year local control was higher than 95%. The results reported in the study conducted by the GEC-ESTRO Breast Cancer Working Group suggest that BCT with interstitial brachytherapy is feasible and effective in preventing second local recurrences, and that this approach achieves OS, DFS, and local recurrence rates that are at least equivalent to those obtained with salvage mastectomy.
In our series, we inserted a median of 14 catheters, with an average PTV volume of 115 cc. We used large PTV volumes to ensure better coverage of the tumor bed, in accordance with the report by Hannoun-Levi et al. [8] who found that the second local recurrence rate was lower in patients who received higher delivered doses with a larger irradiated volume.
Cosmesis
Cosmetic outcomes and fibrosis were slightly worse in our series compared to other reports. However, these bad cosmesis results can be explained by the fact that our patients were treated for recurrent disease, which means they had already undergone two surgeries plus adjuvant external WBI. Although cosmesis was considered satisfactory in most of the patients, our results suggest that patients with locally-recurrent disease should be informed that cosmetic outcomes may be less than optimal with this technique. Nevertheless, patients – and clinicians – may consider this to be an acceptable trade-off given the good survival rates achieved with this treatment approach, especially since the only alternative is mastectomy (with or without reconstructive surgery). Although several cases of acute and chronic mastitis were observed in our series, these were successfully managed with supportive therapy without need for additional surgery.
Study strengths and limitations
The main limitations of this study are the retrospective study design and the relatively small sample size. Another limitation is the lack of a homogenous treatment scheme, which was modified during the study period. Nonetheless, the EQD2 was equivalent.
Conclusions
The use of the APBI for primary breast cancer is well-established in clinical practice. In patients who develop ipsilateral breast cancer recurrence, the available evidence shows that a second conservative treatment should be considered in well-selected patients. The data reported in this study support the feasibility and safety of APBI, with multicatheter interstitial brachytherapy as a salvage treatment. The body of evidence from this and other studies suggests that this breast-conserving treatment approach is a reasonable alternative to mastectomy. In our series, local control, survival, and toxicity outcomes were good. Although cosmetic outcomes were less than fully satisfactory in some patients, the only alternative that these patients have is mastectomy. Salvage brachytherapy after tumorectomy seems to be safe and effective. However, randomized trials are needed to compare this approach to mastectomy.



