Introduction
Adolescence is a period which favors the development of some somatic and mental disorders due to the high dynamics of biological changes occurring in the organism. It is often difficult to differentiate between symptoms that are still within the developmental norm and those that are considered a pathology. It is a time when we start to observe many autoimmune disorders, for instance juvenile-onset systemic lupus erythematosus (jSLE), which often develops insidiously without any symptoms matching the criteria.
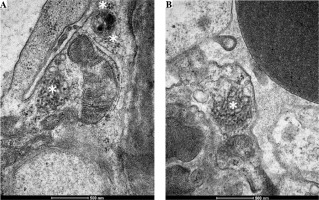
We present a case of a 16-year-old female patient with jSLE which manifested only with severe depression resistant to treatment. For a long time it was not accompanied by any somatic symptoms. Because of isolated proteinuria and presence of antinuclear antibodies renal biopsy was performed. Light microscopy showed only findings characteristic for membranous nephropathy. Examination of the specimen on electron microscopy showed characteristic tubuloreticular inclusions (TRIs). This finding aids in the diagnosis of lupus nephritis (LN) when other criteria for lupus are not met.
Case report
The 16-year-old female patient had presented with anxiety, suicidal thoughts and episodes of self-harm at the age of 12. The symptoms occurred about 12 months after menarche. At that time, the patient was hospitalized in a psychiatric department due to the ingestion of a large dose of ibuprofen for suicidal purposes. A moderate depressive episode was diagnosed based on the observation and diagnostic tests (Beck Depression Inventory). An improvement in mood was observed after treatment with fluoxetine and opipramol dihydrochloride, followed by a tendency to somatization (gastrointestinal complaints and fainting). The somatic basis of symptoms was not found. Brain magnetic resonance imaging was normal. The patient continued drug therapy and attended psychotherapy. However, behavioral disorders were more intense, she became isolated and was reluctant to attend school. Suicidal thoughts also became more intense. The patient also presented with lowered mood and apathy, and had problems with maintaining personal hygiene. She also erotized relationships with the medical personnel and peers. The treatment was modified and sertraline and flupentixol were administered.
At the age of 14, a routine urinalysis showed proteinuria (0.4 g/l). Regular urine examinations performed for 6 months also showed proteinuria (0.4-1.1 g/l). To diagnose this condition, the patient was hospitalized in the Department of Pediatric Nephrology. On admission, physical examination revealed excessively developed subcutaneous tissue and stretch marks. The patient did not report any complaints. Laboratory tests are given in Table 1. She was positive for antinuclear antibodies (ANA); other autoantibodies were negative. Abdominal ultrasound showed normal size and echogenicity of the kidneys. The orthostatic test was negative. A diagnostic renal biopsy was performed to determine the cause of proteinuria. Light microscopy showed only the presence of C4d and IgG deposits around the glomerular capillary walls, which confirmed the diagnosis of membranous nephropathy. At the time when primary membranous nephropathy was suspected, tests for anti-PLA2R and anti-THSD7A antibodies were performed. However, they were negative. Tests for viral infections were also performed (hepatitis C virus [HCV], hepatitis B virus [HBV], Epstein-Barr virus [EBV], Cytomegalovirus [CMV]). They were suspected as potential pathogens causing secondary membranous nephropathy. However, the results were also negative. Ultrastructural examination of the renal biopsy showed changes in the structure of the capillary basement membrane in the form of thickening and an irregular contour. Electron dense subepithelial and mesangial deposits were found. In addition, many TRIs were observed in the endothelial cells of the vascular bundle (Fig. 1). They were detected in the cytoplasm and in the dilated cisternae of the endoplasmic reticulum. Single TRIs were also located in close proximity to subepithelial deposits. After obtaining these results, the criteria for lupus were met (depression as a sign of neuropsychiatric systemic lupus erythematosus (NPSLE), proteinuria, the presence of ANA, renal biopsy results) and appropriate treatment was provided. It included ramipril, steroids and cyclosporine A. Due to persistent psychiatric symptoms, steroid doses were reduced and steroid therapy was discontinued after 5 months. The treatment resulted in the resolution of proteinuria and normal renal function (estimated glomerular filtration rate [eGFR] 104 ml/min/1.73 m2). No proteinuria was found in the urine and the urine output was 0.12 g/24 h.
Table 1
Results of laboratory tests of the patient
Discussion
Early onset of nephropathy and the occurrence of symptoms from the nervous system are typical of the clinical course of jSLE, particularly when the disease occurs at a younger age. These two systems are particularly predisposed to be involved in the disease process in pediatric patients [1].
Patients with NPSLE may present with one or more neuropsychiatric symptoms such as cognitive impairment, anxiety, mood disorders, or psychosis [2]. Among the many possible manifestations, depression is the most common presentation, and its prevalence is established at 17% to 75% in the general population [3]. In adults with lupus, the prevalence of depression is the subject of many studies [4]. However, such studies have not been conducted on the pediatric population and related data are very inconsistent. According to a systematic review, the prevalence of depressive disorders in SLE in pediatric patients was estimated at 6.7% to 59%, and anxiety disorders at 34-37% [5]. Most studies have shown that symptoms of NPSLE in the form of depression occur at different times of the disease (mostly during the first 3-5 years after diagnosis) [2]. Occasionally, they occur at the time of disease manifestation and can be rarely the first symptom (as in the case of our patient), preceding the onset of other clinical and serological markers of lupus. Brazilian authors presented a case of a 12-year-old girl in whom depression was the first symptom of lupus. Investigation for a systemic disease was made when the nephrotic syndrome occurred in the course of LN and positive ANA tests were found [6]. In our patient, the symptoms of major depression, self-harm and suicide attempts preceded the onset of other symptoms of lupus by almost three years and persisted throughout psychiatric treatment and after the diagnosis of jSLE.
Currently, there is no specific test that could clearly distinguish NPSLE from other neuropsychiatric diseases. The lack of specific, reliable and validated diagnostic markers results in the fact that a correct diagnosis of NPSLE is based on the exclusion of other causes. Despite efforts to identify biomarkers of NPSLE by laboratory and imaging studies, none of the markers has proven sufficiently reliable for use in clinical practice. Among autoantibodies, the most promising candidates for biomarkers include antiphospholipid (aPL) antibodies, anti-ribosomal P antibodies, and anti-neuronal and anti-NR2 antibodies (to a lesser extent). Concentrations of various cytokines, chemokines, products of the complement cascade and other proinflammatory mediators are increased in the cerebrospinal fluid (CSF) of NPSLE patients. Conventional MRI (cMRI) is currently the gold standard of neuroimaging in the assessment of patients with NPSLE. However, as many as 40-50% of patients with a clinical diagnosis of NPSLE have no abnormalities on cMRI, while many chronic abnormalities on cMRI are not associated with clinically overt NPSLE [2].
Isolated proteinuria, especially in adolescents, is usually not an indicator of renal disease. Orthostatic or postural proteinuria is common in adolescents and should be ruled out first in cases of isolated mild proteinuria [7]. Proteinuria may also be the first sign of LN, which is one of the most common manifestations of juvenile SLE. Renal involvement in lupus affects 50-80% of children. More than 90% of patients develop LN within 2 years from the diagnosis [8]. The coexistence of other clinical, laboratory or serological features of lupus is an indication for a renal biopsy [8]. The occurrence of proteinuria in the third year of psychiatric treatment was a breakthrough for the diagnostic process and the suspicion of the somatic basis of depression. The patient was positive for antinuclear antibodies (ANA). Other antibodies were not detected. According to the 2012 American College of Rheumatology recommendations, a renal biopsy should be performed in every case of active SLE, when renal involvement is suspected, and when the diagnosis is uncertain and serologic test results are inconclusive [9].
Transmission electron microscopic (TEM) evaluation of biopsy specimens is currently also recommended because it provides further valuable details of intracellular structure, such as the presence of TRIs [10]. These are subcellular structures located in the cisternae of the endoplasmic reticulum, and their formation was linked to exposure to excess endogenous or exogenous interferon (IFN) [11, 12]. The presence of TRIs in LN is not a specific finding as they commonly occur in viral diseases. However, different studies have shown that TRIs are significantly associated with early manifestations of SLE, especially in pediatric patients [12, 13]. In our patient, the presence of a large number of TRIs was the basis for establishing the diagnosis of jSLE and linking treatment-resistant depression to an insidiously developing systemic disease. Japanese authors described a similar case. The presence of TRIs on electron microscopy considerably preceded meeting other criteria for lupus. At the time of the first relapse of nephrotic syndrome, the patient did not meet clinical or serological criteria for lupus. The biopsy findings on light microscopy corresponded to membranous nephritis (the ultrastructure of the glomeruli was not assessed at that time). After 11 years, during the relapse of nephrotic proteinuria, when ANA and anti-dsDNA antibodies were found, the biopsy was re-examined and the assessment was extended by electron microscopic evaluation. The ultrastructure of the biopsy showed the presence of many TRIs [14], which supported the thesis that such structures could be an ultrastructural marker of developing lupus many years before a definitive diagnosis.
The assessment for TRIs was very useful and conclusive in our patient. The criteria for lupus were not met until the biopsy results were available. TRI expression in endothelial cells of glomerular capillaries is a significant early morphological sign of SLE, which often precedes disease progression [12]. The evaluation of renal biopsy specimens by electron microscopy could be a useful diagnostic step to confirm the diagnosis, especially in difficult cases where the criteria for SLE are not fully met.